Anterior Cruciate Ligament Reconstruction in the Skeletally Immature Patient
J. Todd R. Lawrence
R. Jay Lee
Mininder S. Kocher
DEFINITION
Skeletally immature patients have open growth plates, or physes, and thus have growth potential remaining.
Intrasubstance anterior cruciate ligament (ACL) injuries were once considered rare in this population, with tibial eminence avulsion fractures considered the pediatric ACL injury equivalent.14 However, intrasubstance ACL injuries in children and adolescents are being seen with increasing frequency and result in an “ACL-deficient knee” as in adult patients.
ACL deficiency in the skeletally immature patient usually results in an unstable knee at risk for further injury and accelerated degeneration.
Conventional surgical reconstruction techniques risk potential iatrogenic growth disturbance due to physeal violation, and thus special consideration must be given to this patient population.10
The physiologic age of the patient reflects the amount of remaining growth potential and knee size and thus heavily influences the treatment options.
ANATOMY
The ACL originates from a semicircular area on the posterior portion of the medial aspect of the lateral femoral condyle and courses obliquely to the anteromedial aspect of the tibial plateau at the anterior tibial eminence (or spine).
The primary role of the ACL is to resist anterior translocation and rotation of the tibia on the femur.
The ligament is composed of two anatomically and biomechanically distinct bundles: the anteromedial and the posterolateral bundles.
The anteromedial bundle is more anterior and vertical in orientation. It largely resists anterior translation and tightens in the last 30 degrees of extension.
The posterolateral bundle is more posterior and oblique in orientation. It is more isometric and plays a greater role in rotational control.
Not all skeletally immature patients are the same. Some have a tremendous amount of growth remaining, whereas others are essentially done growing.
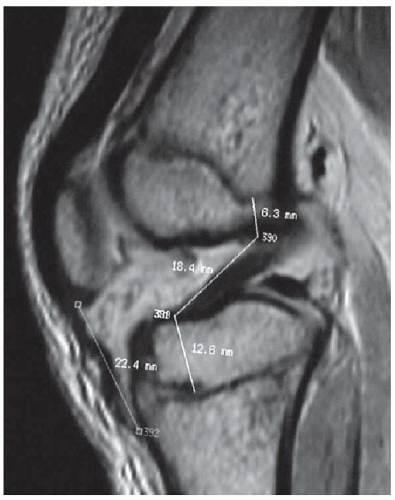
Most of the longitudinal growth of the lower extremities comes from the distal femur and the proximal tibia. The tibial physis can be as close as 15 to 20 mm to the tibial spine. The femoral physis comes within millimeters of the femoral attachment of the ACL at the most posterior aspect of its insertion (FIG 1).
PATHOGENESIS
The etiology of ACL injury in skeletally immature patients is similar to that in the adult population. It is usually due to a noncontact injury involving a cutting, pivoting, or rapid deceleration maneuver.
Patients often report hearing a “pop” followed by swelling of the knee. ACL injury has been reported in up to 65% of pediatric patients with acute traumatic hemarthrosis.17
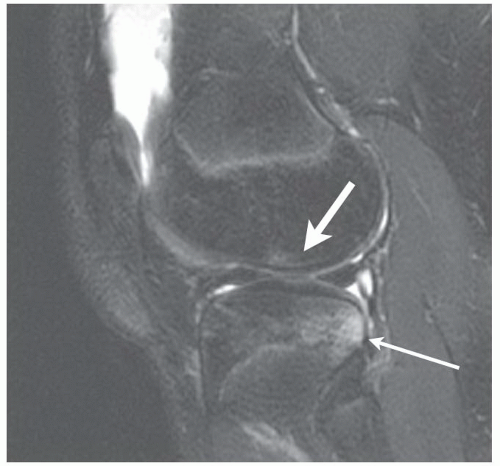
The “shift” that occurs with the ACL-deficient knee at the time of injury causes an impaction injury on the posterior aspect of the tibial plateau against the distal femur at the sulcus terminalis as the tibia translates anteriorly on the femur. Characteristic bone bruises in this location on magnetic resonance imaging (MRI) are pathognomonic for ACL injury (FIG 2).
Ligamentous, meniscal, and chondral injuries are commonly associated with ACL injury.
The medial collateral ligament is commonly injured with the ACL.
The posterolateral corner is less often injured with the ACL but is a common cause of failure of ACL reconstruction if it is not addressed as well.
Tears of the lateral meniscus are associated with acute tears of the ACL.
The posterior horn of the medial meniscus is a secondary restraint to anterior translation of the tibia. In the chronically ACL-deficient knee, the posterior horn of the medial meniscus assumes a greater role in preventing anterior translation and is thus at increased risk of injury.
NATURAL HISTORY
Partial tears may be successfully managed nonoperatively in some patients.9
Complete tears in skeletally immature patients generally have a poor prognosis, with instability leading to further meniscal and chondral injury.1,12
Over half of patients show evidence of early degenerative changes 4 to 5 years after their injury with nonoperative management.12
Patients who have a greater amount of instability, as measured objectively with KT-1000 arthrometry, or pursue higher level cutting and jumping sports, are at greater risk for recurrent injury.3
ACL reconstruction can reduce the risk of ongoing mechanical meniscal and chondral injury associated with instability. However, how this influences the risk of developing degenerative joint disease is not clear at this time.
PATIENT HISTORY AND PHYSICAL FINDINGS
Adolescents are notoriously bad historians, but every attempt should be made to garner an appreciation for the mechanism of injury, a history of acute or recurrent effusions, and a sense of instability with activities or mechanical symptoms.
Physiologic age should be established informally in the office using the Tanner staging system.18 This can be confirmed in the operating room after the induction of anesthesia. Skeletal age can be determined via hand and wrist radiographs per the method of Greulich and Pyle.4
A complete examination of the knee should be performed. Particular attention should be given to evaluating the knee for associated pathology.
Overall, lower extremity alignment, angular deformity, and any leg length discrepancy should be noted.
Patellar ballottement and fluid wave test should be done to evaluate for the presence of an effusion.
Range of motion (ROM) is important to assess because regaining full ROM before ACL reconstruction may be critical to prevent postoperative arthrofibrosis. Loss of extension should alert the clinician to the possibility of a displaced bucket-handle tear or preoperative arthrofibrosis. Loss of flexion may be due to pain secondary to a tense effusion.
Tenderness to palpation should be assessed and localized specifically as it can greatly direct the diagnosis of related injuries.
Tenderness to palpation along the joint line, particularly the posterior aspect of the joint line, should alert the clinician to the possibility of a meniscal tear. Pain or palpable popping with provocative maneuvers, such as McMurray, Apley compression, or duck walk, will help to confirm this finding.
Pain along the course of or at the femoral or tibial insertion points for the collateral ligaments should alert the clinician to the possibility of a collateral ligament tear.
Pain at the physis should prompt an investigation for a physeal injury, although in our experience, this is not commonly associated with complete ACL injuries.
Tenderness along the medial retinaculum or the course of the medial patellofemoral ligament can indicate an acute patellar dislocation that reduced spontaneously.
Ligamentous evaluation should include the anterior and posterior cruciate ligaments, the medial and lateral collateral ligaments, and the posterolateral corner.
Skeletally immature athletes have a greater degree of physiologic laxity than adult athletes and as such a comparison should always be made to the uninjured knee.
Evaluation of the ACL is best done with the Lachman test in the cooperative patient. In the patient who voluntarily or involuntarily guards against traditional Lachman testing, the prone Lachman or the anterior drawer tests may encourage relaxation and give a more reliable examination.
Pivot shift testing may be performed in the office but is usually not well tolerated by pediatric patients. It should be performed in the operating room as part of the preoperative evaluation of every patient.
The posterior cruciate ligament should be evaluated using the posterior drawer test. The relative starting point should always be assessed first and compared to the contralateral side. The use of posterior drawer stress radiographs is unclear at this time. Injuries of grade II and above should alert the clinician to the possibility of an associated posterolateral corner injury.
Medial and lateral collateral ligament injuries are assessed through stress opening with valgus and varus stress at 0 and 30 degrees of knee flexion. In the pediatric patient, opening with varus and valgus stress can be due to physeal injuries, and the clinician should always be vigilant for this.
Evaluation of the posterolateral corner is best done with the dial test. The posterolateral drawer and the external rotation recurvatum tests are also useful for evaluating posterolateral corner injuries.
Evaluation for patellar instability with apprehension testing should be performed.
Evaluation of quadriceps bulk and strength is important for postoperative recovery.
IMAGING AND OTHER DIAGNOSTIC STUDIES
All pediatric patients with a complaint of knee pain should receive an initial plain radiographic evaluation including anteroposterior (AP), lateral, and patellar views. With a traumatic injury, both oblique views should be obtained. If there is a concern for an osteochondritis dissecans lesion in the differential, a notch view should also be obtained. In scrutinizing the radiographs, special attention should be given to evaluate for physeal injuries as well as other injuries on the differential diagnosis.
AP and frog-leg lateral plain radiographs of the hip should be considered in the evaluation of all pediatric patients with complaints of knee pain.
Overall varus and valgus malalignment or leg length discrepancies, if present clinically, should be evaluated with fulllength, hip-to-ankle radiographs.
MRI is the diagnostic imaging test of choice for further evaluation of ACL tears in the skeletally immature patient. Recent high-field strength magnets with quality imaging has shown high sensitivity and specificity for diagnosing ACL injuries in this population15 despite earlier reports noting decreased diagnostic value compared with the adult population.6 Findings on MRI signifying an ACL tear include a discontinuity in the fibers on the ACL and a characteristic bone bruise pattern on the distal femur and the posterior tibial plateau of the lateral hemijoint.
MRI in the pediatric population has a high false-positive rate for meniscal tears. This is likely due to the increased vascularity of the meniscus, which is often interpreted as intrasubstance degeneration or a tear of the meniscus.6
DIFFERENTIAL DIAGNOSIS
Tibial eminence (spine) fracture
Other intra-articular or physeal fracture
Patellar dislocation
Meniscal tear
Posterior cruciate ligament tear
Medial or lateral collateral tear
Posterolateral corner injury
Physiologic laxity
Hip etiology
NONOPERATIVE MANAGEMENT
Partial or incomplete tears can be successfully managed nonoperatively in some patients if clinical and functional stability is present. The following criteria have been shown to be associated with successful nonoperative treatment of partial tears9:
Tears of less than 50% of the ligament
Relative preservation of the posterolateral bundle
Age younger than 14 years
Normal or near-normal Lachman or pivot shift test
Up to a third of patients may require subsequent reconstruction and should be made aware of that risk at the onset of treatment.
Successful treatment based on the earlier criteria includes the following:
A hinged knee brace is worn for 12 weeks.
Touchdown weight bearing is maintained for 6 to 8 weeks.
Passive terminal extension is restricted for the first 6 weeks.
Open-chain activities and active terminal extension is restricted for 12 weeks.
Physical therapy emphasizes hamstring muscle strengthening.
Return to sports and active play is permitted at 3 to 6 months if strength and functional testing are symmetric with good form on all activities. A functional knee brace is recommended for 2 years for cutting and pivoting activities.
Nonoperative management of complete tears in skeletally immature patients generally has a poor prognosis.
For prepubescent patients with a complete ACL tear but without a concurrent chondral injury requiring stabilization or meniscal injury requiring repair, we still discuss nonoperative treatment with activity modification, functional bracing, and continued rehabilitation.
In our experience, compliance with activity modification and brace use and effectiveness limits the success of this treatment.
Delay in surgical stabilization can lead to further meniscal and chondral injury due to recurrent instability.
Although results of nonoperative management are generally poor, the risk of further intra-articular injury by waiting until skeletal maturity to undergo reconstruction must be weighed against the risk of growth disturbance with early reconstruction.
Some patients are able to cope with their ACL insufficiency or modify their activities, allowing for further growth and aging such that the reconstruction may be performed when little or no growth remains, minimizing risk for growth disturbance.
For prepubescent patients with ongoing instability, early reconstruction with a physeal-avoiding procedure is indicated.
For adolescent patients with growth remaining who have a complete ACL tear, we do not advocate initial nonoperative treatment because the risk of functional instability resulting in injury to the meniscal and articular cartilage is high and there are anatomic reconstruction options that have a minimal risk of growth disturbance.
SURGICAL MANAGEMENT
Conventional adult ACL reconstruction techniques risk potential iatrogenic growth disturbance due to physeal violation, and cases of growth disturbance have been reported in animal models and clinical series.10
The following principles should always be followed with any reconstructive strategy:
No hard fixation, such as with an interference screw, should cross the physis because it has a high risk of inducing a growth disturbance.
No bone, such as that associated with a bone-patellar tendon-bone graft, should cross the physis because it also has a high risk of inducing a growth disturbance.
The following principles should be taken into consideration and approached with great caution when deciding on a reconstructive strategy:
Drill holes across the physis should be as small and as central in the physis as possible.
Oblique drill holes across the physis affect a larger portion of the physis than do perpendicular drill holes of the same diameter. This is especially important when considering placement of the femoral tunnel.
A tensioned soft tissue graft in a bone tunnel across the physis can also induce a growth disturbance.
Excessive dissection around the posterolateral aspect of the femoral physis or performance of an aggressive
notchplasty should be avoided to prevent injury to the perichondral ring and subsequent deformity.
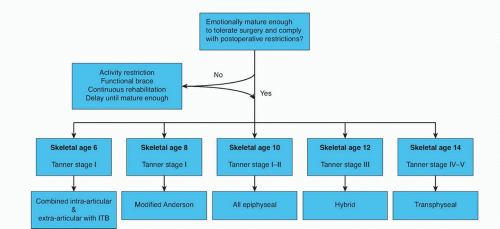
The approach to ACL reconstruction in the skeletally immature patient should be based on physiologic age and growth remaining. Knee size can also be considered in the feasibility of various techniques (FIG 3).
A variety of reconstructive techniques have been used, including physeal-sparing, partial transphyseal, and transphyseal methods using various grafts.
In prepubescent patients with large amounts of growth potential remaining, and smaller knees, a physeal-sparing, combined intra-articular and extra-articular reconstruction using autogenous iliotibial band should be considered.
Recognizing that the combined intra-articular and extraarticular reconstruction using autogenous iliotibial band described here is nonanatomic, we still counsel patients and families that revision reconstruction may be needed if recurrent instability develops, but this procedure may temporize for further growth such that the patient may then undergo a more conventional reconstruction with drill holes.
However, we have found that few revision reconstructions are necessary with the combined intra-articular and extraarticular reconstruction and that long-term function is similar to other reconstructions.
In prepubescent patients with large amounts of growth potential remaining, and larger knees, an all-epiphyseal reconstruction using autogenous hamstrings may be considered.
In adolescent patients with significant growth remaining, transphyseal ACL reconstruction with autogenous hamstring tendons with fixation away from the physes can be considered.
In adolescent patients approaching skeletal maturity, we perform conventional adult ACL reconstruction with interference screw fixation using either autogenous central-third patellar tendon or autogenous hamstrings (see Chap. 10).
A variety of other physeal-sparing or physeal-respecting hybrid reconstructions have been described and may be used in cases where patients are in between the previously noted categories (FIG 4). One common reconstruction technique is the epiphyseal femoral tunnel combined with the transphyseal tibial tunnel to avoid creating such an oblique femoral tunnel in a younger adolescent with significant growth remaining.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree