Chapter 41 Anterior Cruciate Ligament Injuries and Reconstruction
Indications, Principles, and Outcomes
Injury to the anterior cruciate ligament (ACL) is the most common ligament injury in the knee and results in between 50,000 and 105,000 reconstructions/year in the United States.51,82 Greater participation in sporting and recreational activities by the general population continues to expose more individuals to the risk of ACL rupture. As the experience of orthopedic surgeons with ACL injuries has expanded, so have the science and technique of ACL reconstruction. Numerous methods for reconstructing the ligament exist, including the use of patellar tendon autograft, hamstring tendons, and allograft material. The most extensive research has been performed on the use of patellar tendon autograft, and this technique remains the gold standard for ACL reconstruction.66 Since the last edition of this text, there have been a significant number of meta-analyses and systematic reviews of the literature in this area in an attempt to combine studies and achieve greater success. We have revised this chapter to include these important additions to the literature.
History of Anterior Cruciate Ligament Reconstruction
Use of the central third of the patellar tendon for reconstructing a torn ACL was first described by Jones71 in an effort to provide a more physiologic procedure than those previously described. His technique involved transferring the patellar tendon with a patellar bone block to the intercondylar region of the femur while maintaining the distal attachment of the tendon to the tibial tubercle. Other authors subsequently modified Jones’ technique by using the medial third of the patellar tendon.5,47 Marshall and colleagues84 have described using the central third of the patellar tendon along with the prepatellar fascia and central portion of the quadriceps tendon. These modifications of Jones’ technique also involved creating a more anatomic placement of the reconstructed ligament by passing it through a tibial tunnel, from the anterior aspect of the tibia to the normal tibial ACL insertion site, and leaving the distal attachment of the patellar tendon in place on the tubercle. The femoral side of the graft was passed either through bone tunnels in the femur or over the top of the lateral femoral condyle and secured with sutures or staples. Clancy and associates,39 in an effort to obtain bony union at the femoral fixation site, first described harvesting a block of patellar bone along with the proximal portion of the patellar tendon. They also described detaching the tibial origin of the graft along with a block of bone when the graft was found to be too short. The bone-patellar tendon-bone graft (BPTB) is now the gold standard in ACL reconstruction. Advantages of this type of autograft include its increased stiffness and energy to failure, as well as its ability to revascularize.11 It has been shown that a 14- to 15-mm-wide BPTB graft has a mean strength that is approximately 168% that of a normal ACL.98 Current graft widths are closer to 10 mm, but continue to possess greater tensile strength than a native ACL.140 In addition, the BPTB autograft has a superior ability to achieve stable initial fixation as a result of the bone plugs providing bone to bone healing.
Predisposing Factors and Associated Injuries
Several studies have attempted to identify factors predisposing to ACL injury and have found an association between such injury and intercondylar notch stenosis.79,133 Souryal and Freeman132 prospectively examined 902 high school athletes and noted that athletes who sustained ACL tears had statistically significant stenosis of the intercondylar notch when compared with those who did not have such injuries. Harner and coworkers63 compared 31 patients with noncontact, bilateral ACL injuries with 23 controls who had no history of knee injury. Computed tomography (CT) analysis of the lower extremities revealed that the width of the lateral femoral condyle was significantly larger in the injured knee group and was the predominant contributor to intercondylar notch stenosis. A study comparing notch width measurements in men and women with and without ACL tears revealed a narrower intercondylar notch width in women than in men, as well as a narrower width in patients with ACL tears than in controls.120 These results may enable identification of individuals at increased risk for unilateral and, in particular, bilateral ACL tears, which have an overall incidence of approximately 4%. In addition, this may be one factor responsible in part for the increased incidence of ACL tears in female athletes.
Much attention has been focused on the cause of ACL tears in women. Studies investigating injury rates noted that women sustain four to eight times the number of ACL injuries as men in the same sports.10,24 Possible reasons for this discrepancy include extrinsic factors, such as muscle strength, and intrinsic factors, such as joint laxity, notch dimensions, and lower stiffness to applied load.116 Little objective evidence is currently available, however, to support a single hypothesis. The association between female athletes’ menstrual cycle and ACL injuries has been examined.20,103 More injuries than expected were noted during the preovulatory and ovulatory142 phases of the cycle, when a surge in estrogen production occurs. This finding suggests that noncontact ACL tears in female athletes may be related in part to hormonal fluctuations. The hormones responsible for this observed association and the effect of the mechanism of action on the mechanical properties of the ACL have yet to be determined. A recent meta-analysis has concluded that neuromuscular training and strengthening can reduce the risk of ACL injury in female athletes, particularly those less than 18 years of age.144
Associated injuries at the time of ACL tear affect surgical management and outcomes. Jumping versus nonjumping ACL injuries were reviewed in 263 patients. Those associated with a jumping mechanism were associated with a significantly higher rate of meniscal tears.8,107 Postulating that anthropomorphic characteristics were associated with intra-articular injury at the time of ACL tear, Bowers and colleagues26 reviewed their ACL database, for height, weight, and body mass index (BMI). Increases in all three variables were associated with higher rates of associated specific intra-articular pathologies at the time of ACL reconstruction. It was thus hypothesized that by reducing weight and BMI, patients could reduce associated injuries and improve outcomes following ACL reconstruction.
Indications for Reconstruction
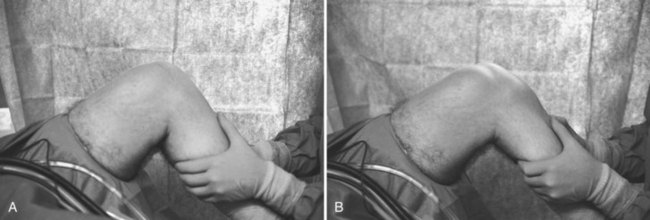
Identification of patients with an ACL injury can usually be made on the basis of the history and physical examination. Patients commonly describe a history of a deceleration injury, with or without contact, during such maneuvers as cutting and pivoting. Patients with this injury mechanism associated with an audible pop, severe pain, and significant swelling of the knee can be assumed to have a torn ACL. Physical examination confirms the diagnosis by demonstrating a positive pivot shift, Lachman,138 or anterior drawer test in the injured knee as opposed to a contralateral normal knee (Fig. 41-1).
After the acute phase of knee pain and swelling subsides, symptomatic patients complain of persistent instability and giving way of the knee, which can be associated with intermittent episodes of swelling. Once a torn ACL is diagnosed, one must decide whether to recommend nonoperative or operative treatment. Satisfactory results from conservative treatment of ACL tears have been reported.52 McDaniel and Dameron89 have noted that 70% of patients with complete ACL tears treated conservatively return to strenuous sports. Similarly, Giove and associates55 reported a 59% rate of return to sports activities after a program emphasizing hamstring strengthening. However, sports requiring sudden stopping and pivoting had the lowest rate of return to participation. Buss and coworkers32 evaluated the results of conservative treatment of acute, complete ACL injuries in older, lower demand patients. They noted that 70% of patients were able to continue with moderate-demand sports at an average follow-up of 46 months. They concluded that conservative treatment in this group of patients can be successful, despite a modest amount of residual instability.
Numerous other studies, however, have reported less successful outcomes of non-operative treatment.8,49,98,99,129 Noyes and colleagues100 have studied 103 athletically active patients an average of 5.5 years after ACL injury. Despite an initial return to sports activity by 82% of the participants,
Fifty-five percent sustained a significant reinjury within 1 year of the original injury and only 35% were participating in strenuous sports at the most recent follow-up. Hawkins and associates65 reported on 40 patients treated nonoperatively with an average follow-up of 4 years and noted 87.5% fair or poor results; only 14% of patients were able to return fully to unlimited athletic activity. Similarly, Barrack and coworkers17 reported 69% fair or poor results after nonoperative treatment in an active naval midshipmen population. Daniel and colleagues43 have determined that the best predictor for later meniscal or ligament reconstruction surgery is total hours per year of levels I and II sports participation before injury. This observation highlights the fact that individuals who engage in demanding recreational or vocational activities do not respond well to nonoperative treatment of ACL injuries.
The decision to reconstruct an ACL tear should be based not only on the presence of symptomatic instability, but also on the lifestyle and activity level of the patient. In a prospective nonrandomized trial of an ACL reconstruction algorithm by Fithian and associates,50 patients were categorized as low, medium, or high activity level and had reconstructions if they fell into the medium or high level group. At an average 6.6-year follow-up, early reconstruction was associated with a reduced rate of knee laxity, symptomatic instability, late meniscal tears, and further surgery.
We do not use guidelines based on age in our practice because the more important factor is the overall level of activity. It is generally agreed that younger individuals have higher levels of activity and, therefore, place greater demands on their knees. However, many older individuals are participating in higher levels of recreational sports and are doing so for longer periods. Consequently, age itself should not be a contraindication to ACL reconstruction. Plancher and coworkers109 have reported 97% good or excellent results after ACL reconstruction in patients older than 40 years at a mean follow-up of 55 months. All patients were satisfied with the procedure, and most were able to return fully to their sports activities, including tennis and skiing.
Symptomatic patients with a more sedentary lifestyle and those who are willing to modify their level of activity can be considered for nonoperative treatment, consisting of a supervised rehabilitation program. One option is initially to treat all patients with an ACL rupture nonoperatively and perform reconstruction on those for whom this form of treatment fails. This approach can involve several months of rehabilitation, followed by several more months if reconstruction is ultimately performed. In our experience, we have found that most patients are unwilling to accept this amount of time away from their recreational activities; therefore, we recommend early reconstruction for symptomatic patients with greater lifestyle demands. The goal of early reconstruction in this patient population is to provide stability, which allows a return to previous activity levels without further damage to the knee, such as meniscal tears and arthrosis. The significant reinjury rates in nonreconstructed knees50,99 emphasizes the potential sequelae of continued high levels of activity in patients with ACL injury.
In a review of 3475 patients in the Norwegian National Knee Ligament Registry undergoing ACL reconstruction between 2004 and 2006,59 timing of reconstruction was examined for its relationship to meniscal tears and cartilage lesions. The odds of cartilage lesion increased by almost 1% for each month elapsed between injury and reconstruction.
Timing of Surgery
The timing of ACL reconstruction has been debated; however, no consensus has yet been reached regarding the ideal timing. Initial concern existed over reconstruction of the ACL during the early postinjury period because of the increased risk for arthrofibrosis and difficulty gaining full motion of the knee postoperatively. Shelbourne and colleagues128 have demonstrated a higher rate of arthrofibrosis in patients undergoing ACL reconstruction within the first week after injury than in those who underwent reconstruction 21 days or longer after injury. The same authors noted, however, that when an accelerated rehabilitation protocol was followed postoperatively, the rates of arthrofibrosis in the two groups were comparable. Noyes and Barber-Westin97 reported that 69% of knees with chronic rupture scored in the normal or very good range after reconstruction as compared with 100% of knees with an acute rupture. Other studies have also found earlier return to sporting activities as well as better clinical and laxity testing results in knees undergoing early reconstruction.83 Hunter and associates69 have shown that the use of modern arthroscopic surgical techniques and an aggressive rehabilitation protocol can yield results that are independent of the timing of surgery. We agree that the specific number of days after injury when the reconstruction should be performed is not as important as the preoperative condition of the knee. Criteria for successful results of ACL reconstruction are minimal or no swelling, good leg control, and full range of motion, including full hyperextension.125
Surgical Technique
Arthroscopic reconstruction of a torn ACL with a BPTB autograft is our procedure of choice and is the technique described here. Steps of the reconstructive procedure include diagnostic arthroscopy, harvesting the graft, preparing the graft, performing the notchplasty, drilling of the tibial and femoral tunnels, passing the graft, and femoral and tibial fixation of the graft. Before beginning the reconstructive procedure, however, the knee is examined under anesthesia. A positive Lachman test and pivot shift sign are sought on the injured knee as clinical evidence of a torn ACL. These maneuvers are repeated on the uninjured contralateral knee for comparison and to determine the degree of normal laxity in the knee for the individual patient. A positive pivot shift under anesthesia is the most sensitive clinical test of the functional status of the ACL because it demonstrates a loss of rotational stability imparted by an intact ligament.15,81 The injured extremity is then prepared and draped in the usual sterile fashion after the application of a thigh tourniquet well above the operative site.
Graft Harvesting
We have examined the effect of graft diameter on postoperative knee stability by testing ACL-reconstructed knees with the KT arthrometer after the use of a 9- or 10-mm-diameter graft.56 The average time from surgery to KT arthrometer testing was 6.6 months, and at the time of testing the average side to side difference for the 9-mm group was 1.02 mm. The average side to side difference for the group receiving 10-mm grafts was 1.14 mm. No significant differences between the two groups could be identified with regard to knee stability.
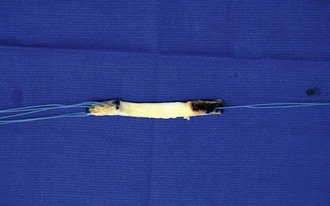
Graft Preparation
Excess soft tissue is first removed from the graft, and the diameter of the bone plugs is trimmed with a rongeur to the appropriate width (9 or 10 mm). The plug from the tibial tubercle is prepared for placement in the femoral tunnel, where its anatomy and less curved geometry provide maximum bone fill. The edges of the plugs are rounded to permit smooth passage of the graft and the diameters are checked by passing the graft through a tunnel template of the correct size. Three drill holes are then made in the patellar bone plug and one in the tibial tubercle bone plug, followed by passage of no. 5 nonabsorbable suture through these holes (Fig. 41-2). The suture facilitates passage and tensioning of the graft. Finally, the total length of the graft is measured. In general, if the total length is between 92 and 97 mm, fixation with interference screws can be achieved. Fixation with a screw and washer on the tibial side is usually required for grafts measuring outside this range.
Notchplasty
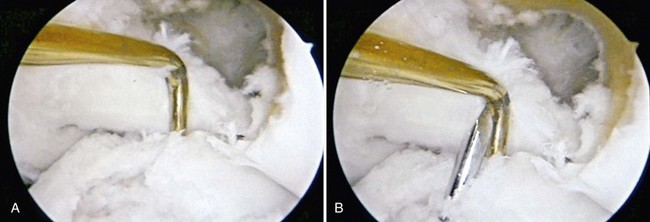
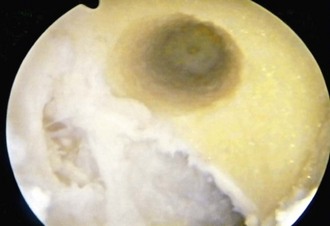
Several studies have attempted to establish guidelines for assessing the adequacy of the notchplasty.57,137 Odensten and Gillquist102 have noted an average maximum distance of 21 mm between the inner surfaces of the medial and lateral femoral condyles in 20 normal cadaver knees. As a result, they suggested that the notchplasty should restore the notch width to this diameter. Berg18 has defined an adequate notchplasty on the basis of the notch width index133 and stated that this index, which is the ratio of the intercondylar width to the total femoral condylar width at the level of the popliteal groove, should be at least 0.250 to prevent impingement of the graft. Howell and associates68 have described the relationship between the placement of the tibial tunnel and the required size of the notchplasty. A more anteriorly placed tibial tunnel requires up to 6 mm of bone removal from the intercondylar roof as compared with only minimal removal of bone for tunnels placed 2 to 3 mm posterior to the ACL tibial insertion site. Berns and Howell19 have further defined the requirements for notchplasty by determining the flexion angle at which the graft contacts the roof through the use of a force transducer in cadaver knees. The angle at which contact occurs averages 12.8 degrees for knees with an eccentrically placed tibial tunnel and requires 4.6 mm of bone removal to achieve zero impingement. This angle of contact decreases to 4.1 degrees when the tibial tunnel is placed 4 to 5 mm posterior to the slope of the intercondylar roof and requires only 1.3 mm of bone removal to prevent impingement. We prefer a generous notchplasty, in which up to 6 mm of bone is removed from the anterior edge of the lateral wall of the notch to prevent any possible impingement on the graft (Fig. 41-3).
The effect of the extent of the notchplasty on the patellofemoral articulation has been investigated. Morgan and coworkers93 have measured patellofemoral contact area and pressure after increasing degrees of notchplasty (3, 6, and 9 mm) and found no statistical differences among the groups. They concluded that routine notchplasty, including up to 9 mm, does not affect the patellofemoral articulation. Patellofemoral complications related to the size of the notchplasty have similarly not been a problem in our experience.
Tunnel Placement
The choice of location for the tibial and femoral tunnels can have a significant effect on the outcome of ACL reconstructive surgery. Several studies have examined the effect of tunnel site on graft impingement,67,143 range of motion,111 and overall clinical results.73 It is recognized that anterior placement of the femoral tunnel is to be avoided to prevent excessive tightness of the graft and thus limit full knee flexion. Similarly, excessive anterior placement of the tibial tunnel may result in graft impingement and early failure. In an attempt to identify definitive landmarks for reproducible tibial tunnel placement, Morgan and colleagues93 have determined that the ACL central insertion point on the intercondylar floor averages 7 mm anterior to the anterior border of the PCL with the knee flexed to 90 degrees; therefore, this is the ideal location for the tibial tunnel.
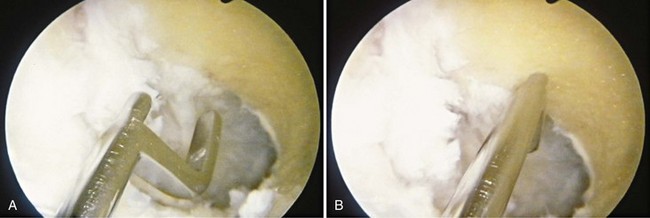
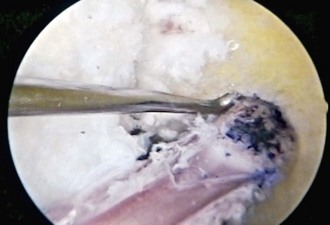
We routinely set the tibial drill guide at 55 degrees. The guide tip is placed through the medial portal and positioned with the use of several landmarks, including the anterior border of the PCL, posterior border of the anterior horn of the lateral meniscus, and interspinous area of the tibial plateau. The tunnel is positioned to enable the graft to drape the PCL (Fig. 41-4). The starting point for the guide pin on the proximal end of the tibia is approximately one fingerbreadth medial to the tibial tubercle and two fingerbreadths distal to the medial joint line. After insertion of the guide pin, the tunnel is drilled with a reamer, and the intra-articular edges of the tunnel are smoothed with a rasp to prevent abrasion of the graft (Fig. 41-5). Attempts have been made to produce the correct tibial tunnel length consistently to prevent graft extrusion with tunnels that are too short, as well as prevent difficult distal fixation and femoral tunnel placement with tunnels that are too long.92 We have found, however, that this is not always accurate and may be altered by small variations in operative technique.105
Attention is then turned to the femoral tunnel. We use a transtibial technique for placement of this tunnel. The guide pin, which represents the center of the tunnel, is placed in the 1:30- to 2-o’clock position for the left knee or the 10- to 10:30-o’clock position for the right knee and 6 or 7 mm anterior to the over the top position, depending on whether a 9- or 10-mm graft, respectively, is used (Fig. 41-6). It is inserted to a depth of 35 mm, or 1.5 inches, to ensure that there is room for the tunnel without violating the posterior cortex (Fig. 41-7). An indentation, or footprint in the bone is then made with the reamer by hand over the guide pin to confirm the correct position in relation to the posterior cortex. This also ensures that the posterior cortex is intact (Fig. 41-8). The tunnel is then reamed to 30 mm with the knee in a flexed position. The reamer is removed, and the arthroscope is placed in the medial port, to assess the integrity of the posterior cortex by visualizing the tunnel directly before passage of the graft (Fig. 41-9).
Testing for isometry can be performed at this point or just before committing to the femoral tunnel. Isometer readings are obtained to determine the position of the graft that will result in equal length and tension throughout a full range of motion. However, it has been shown that these readings may vary widely from the final graft isometry because of eccentric placement of the graft within the bone tunnels.40 Additionally, because the normal ACL is nonisometric, intra-articular testing for isometry is not required if anatomic zones are maintained.141
Graft Passage
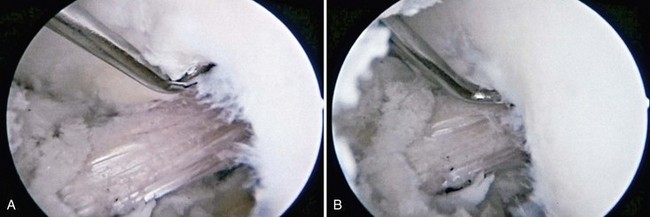
A Beath pin is drilled through the femoral tunnel while maintaining the hip and knee in a hyperflexed position. This position allows the tip of the needle to be pushed through the soft tissues and exit the skin on the anterolateral aspect of the distal part of the thigh. The Beath pin is used to pull the suture in the femoral bone plug through the femoral tunnel. The graft is passed through the tunnels by grasping the sutures on either end of the bone plugs and pulling the graft into the joint. The graft is inserted so that the cancellous bone of the femoral plug is facing anterolaterally in the femoral tunnel (Fig. 41-10). This allows interference screw placement against the cancellous surface of the graft, because insertion of a fixation screw on the cortical surface of the plug may lead to disruption of the ligamentous attachment. Tension is applied to the graft through manual pull on the bone plug sutures and the orientation of the graft is assessed (Fig. 41-11). The arthroscope is used to visualize the intra-articular side of the tibial tunnel to verify that the tibial bone plug does not enter into the joint. Assessment of graft clearance from the notch roof is performed both at 15 degrees of flexion and in full knee extension (Fig. 41-12).
Graft Fixation
Kurosaka and associates77 introduced the self-tapping interference screw, which demonstrated improved mechanical properties when compared with buttons or staples. Regardless of technique, failure occurred at the fixation site. Interference screw fixation demonstrated an increase in ultimate failure load. Paschal and coworkers106 have compared fixation strengths between 9-mm interference screws and sutures tied over a cancellous screw and washer (post fixation) in porcine knees. Higher ultimate failure loads and less displacement of the bone graft were noted with interference screw fixation. Matthews and colleagues87 found no difference in the force to failure of patellar tendon-bone grafts in cadaveric knees when comparing interference screw fixation with post fixation. They did note, however, that post fixation strength is dependent on the type of suture used; no. 5 nonabsorbable suture material provided optimal strength. Despite the conflicting biomechanical results, no studies to date have demonstrated any differences in clinical outcome when comparing interference screw fixation with post fixation.
Absorbable interference screws have been introduced, and several studies have examined the biomechanical properties and clinical results of these screws versus standard metal interference screws.70 Pena and associates108 investigated the insertional torque and failure load for metallic and absorbable interference screws in young and middle-aged cadaveric knees. They noted a higher mean insertional torque for the metal screws as well as a greater mean failure load. Other laboratory studies, however, did not demonstrate any differences between the two types of screws.35,70 Caborn and coworkers36 have compared the maximum load to failure of titanium alloy interference screws with that of absorbable screws in a human cadaveric model with the approximate physiologic strain rate of in vivo BPTB graft loading. No statistical differences were noted between the two groups in the failure mode or the maximum load to failure. Similarly, clinical studies did not demonstrate significant differences in use of the screw types.85 Barber and colleagues16 performed a randomized, prospective, multicenter comparison of bioabsorbable and metallic interference screws in 110 patients undergoing arthroscopic ACL reconstruction with patellar tendon autografts. At a minimum 12-month follow-up, postoperative Tegner and Lysholm scores and KT arthrometer maximum side to side differences were not statistically different between the two groups. It was concluded that the absorbable screw is a reasonable alternative to the metal interference screw for bone plug fixation.
Potential problems with the use of interference screws include length mismatch in the tunnel, graft, and screw, divergence of the screw, graft fracture, and suture laceration.12 Screw divergence has been implicated in failure of graft fixation87; however, others have observed that screw divergence less than 30 degrees does not appear to lead to early failure provided that intraoperative stability is noted.46 Similarly, we examined the effect of divergence between the femoral interference screw and femoral bone plug.117 Radiographs and KT-2000 values from 100 consecutive endoscopic autologous BPTB ACL reconstructions were reviewed at a minimum follow-up of 1 year. The mean anteroposterior divergence angle was 6.6 degrees (range, 0 to 32 degrees), and no association was found between the divergence angle and KT-2000 measurements.
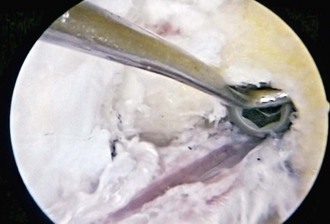
The guide pin for the femoral interference screw should be inserted between the edge of the femoral tunnel and the cancellous surface of the bone plug in a direction parallel to the orientation of the graft. The interference screw is passed over the guide pin and advanced into the femoral tunnel. The screw should engage at least 75%, if not 100%, of the bone block (Fig. 41-13). A 7-mm interference screw is recommended if the bone plug-tunnel gap is 2 mm or less. A gap greater than 2 mm requires the use of a 9-mm screw.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree