Ankle Fractures
Rena L. Stewart
Jason A. Lowe
INTRODUCTION
Ankle fractures are among the most common musculoskeletal injuries. These injuries span a spectrum from simple closed fractures to complex open injuries. As a result, the orthopedic management is varied and can range from nonoperative casting to staged surgery with a primary focus on damage control procedures followed by definitive fixation. Treatment of ankle fractures is also dictated by patient-related factors. The presence of diabetes and a growing population of geriatric patients, with osteoporotic, increase the complexity of ankle fracture management.
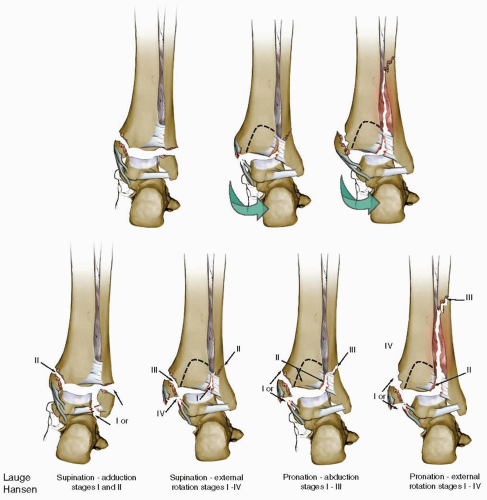
These fractures typically result from a low-energy rotational force to the tibia about a planted foot but can also present as a more complex, high-energy injury. The AO/Danis-Weber and Lauge-Hansen (Fig. 33.1) systems are the most commonly used classifications to describe ankle fractures. The AO/Danis-Weber classification is an anatomic system based upon the location of the fracture with regard to the tibiotalar joint (Weber A—below the joint; Weber B—at the joint; Weber C—above the joint). Lauge-Hansen described four ankle injury patterns based upon the mechanism of injury (Fig. 33.1). These patterns are determined by the foot’s position (supination or pronation) at the time of fracture and the direction of applied force (external rotation, adduction, and abduction).
Injury to the supinated foot begins anterior-lateral and moves around the osteoligamentous structures (posterior then medial) as the force vector continues. If the foot is externally rotated from a supinated position, supination-external rotation (SER), the anterior, inferior tibiofibular ligament (stage I) is the first structure to fail. With continued external rotation, a classic fibula fracture (stage II) occurs. Fibula fractures resulting from an SER injury will have a spiral pattern that moves from anterior-interior to posterior-superior. The long posterior-superior spike of the distal fragment is a hallmark of SER injuries. Continued external rotation results in disruption of the posterior-inferior tibiofibular ligament or fracture of the posterior malleolus (stage III). The most severe SER, stage IV, injury pattern occurs as the rotational force tears through the deltoid ligament or fractures the medial malleolus (typically a transverse fracture). Adduction of the supinated foot will lead to disruption of the lateral collateral ligaments or a tension (transverse) fracture of the distal fibula. As more force is directed medial to the supinated foot, the medial malleolus will fracture. An important distinction of this injury pattern is that the medial column fracture is typically associated with articular impaction of the tibial plafond. In contrast to supination fractures, injuries to the pronated foot begin at the medial malleolus/deltoid ligament to the anterior-inferior tibia-fibula ligament before exiting laterally. Pronation-external rotation injuries are classically observed with a high (suprasyndesmotic) fibula fracture, while pronation-abduction fractures are associated with comminution of the fibula. Questions over the reproducibility and reliability of the Launge-Hansen schema have been raised; however, it remains a useful classification when correlating the mechanism or injury and radiographs following ankle injuries (1).
INDICATIONS AND CONTRAINDICATIONS
Making a decision to treat ankle fractures operatively or nonoperatively depends largely upon the fracture personality: open versus closed, stable versus unstable, displaced versus nondisplaced, and the presence or absence of articular impaction. Many of these injuries, such as isolated closed lateral or medial malleolar fractures, can be successfully treated nonoperatively (2,3). Fibula fractures with displacement of 2 mm or less, without ankle instability, can be managed conservatively in a walking cast or boot. Similarly, medial malleolar fractures with
up to 5 mm of displacement, with no mortise instability, or articular impaction can be successfully treated with cast immobilization and regular radiographic follow-up (Fig. 33.2) (2). Nonoperative treatment is also recommended for patients whose medical condition precludes operative intervention. Operative management is recommended for open fractures and unstable fractures patterns, which include bimalleolar, bimalleolar equivalent (fibula fracture with deltoid ligament disruption), and trimalleolar fractures (3,4).
up to 5 mm of displacement, with no mortise instability, or articular impaction can be successfully treated with cast immobilization and regular radiographic follow-up (Fig. 33.2) (2). Nonoperative treatment is also recommended for patients whose medical condition precludes operative intervention. Operative management is recommended for open fractures and unstable fractures patterns, which include bimalleolar, bimalleolar equivalent (fibula fracture with deltoid ligament disruption), and trimalleolar fractures (3,4).
Determination of ankle stability is crucial during the initial evaluation and assessment of the fracture. If unrecognized, ankle instability may alter the joint contact pressure and can result in abnormal loading of the articular cartilage. Such changes can lead to posttraumatic osteoarthritis of the ankle joint (5, 6, 7 and 8). Since physical exam findings including medial tenderness, with or without swelling and ecchymosis, do not consistently correlate with disruption of the deep deltoid ligament, radiographic landmarks identified on high-quality anterior-posterior (AP), mortise, and lateral radiographs are employed when determining ankle stability (discussed below).
PREOPERATIVE EVALUATION AND PLANNING
Good preoperative planning is essential for successful outcomes in all ankle fractures and begins with a thorough history and physical exam. Medical comorbidities such as diabetes, obesity, and osteoporosis negatively affect the patient’s functional outcome. Recognizing these illnesses in the preoperative period allows modification of the operative plan (fixation scheme), rehabilitation protocol, and optimization of the medical disease in the perioperative period.
A complete neurovascular physical exam of ankle fracture patients, particularly the medically ill and polytraumatized patient, is required. We routinely do not evaluate ankle range of motion in patients with known unstable fracture; however, we routinely assess for the presence of palpable pulses and intact motor function of the ankle and toes. Additionally, peripheral nerves are evaluated for light touch sensation. In diabetic patients, protective sensation is assessed with a 5.07 Semmes Weinstein monofilament. The location and condition of preinjury chronic wounds or acute soft-tissue injury, including ecchymosis, fracture blisters, lacerations, and abrasions, are documented.
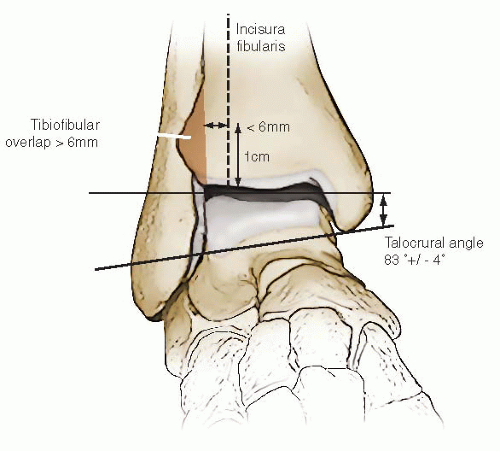
An ankle fracture is assessed for stability using anatomic landmarks identified on radiographs. A clear symmetric joint line along the medial, lateral, and superior joint should be observed. Disruption of the syndesmosis is a marker of instability and can be observed on the AP or mortise radiograph by assessing the tibia-fibula overlap. The distance between the medial fibular cortex and the fibular incisura should be <6 mm when measured 1 cm proximal to the joint. Similarly, the tibia should overlap the fibula by >1 mm on a mortise view and 6 mm on a true AP radiograph. Disruption of the syndesmosis will increase the clear space between the fibula and incisura as well as decrease the tibia-fibula overlap either of which is a sign of instability. Another radiographic indication of instability is disruption of the deep deltoid ligament, which can be assessed on the ankle mortise view. Disruption of the deltoid is appreciated when there is asymmetry of the joint, talar tilt, or translation. The space between the medial malleolus and talar dome (medial clear space) should measure <4 mm and the talocural angle 83 ± 4 degrees (Fig. 33.3). A medial clear space >4 mm indicates disruption of the deltoid ligament or a bimalleolar equivalent fracture.
Ankle instability, however, may not be readily visualized on injury radiographs. SER injuries in particular do not immediately reveal the full extent of the injury. In “apparent isolated” SER II fibular fractures, 38% to 65% of fractures may also have disruption of the deltoid ligament (SER IV) (4,9). While a true SER II injury is stable and can be treated nonoperatively, an SER IV injury represents an unstable fracture pattern and internal
fixation is recommended. The dynamic instability present in these injuries can be better appreciated following an external rotation stress radiograph (manual stress or gravity stress) (9, 10 and 11). During the stress test, it is important that the foot be in either neutral or slight dorsiflexion so as to not falsely reduce the radiographic medial clear space (12). Alternatively, a magnetic resonance imaging (MRI) can also show an occult deltoid ligament injury (1,13). The cost difference between a MRI and stress radiograph is substantial, and the authors do not recommend routine use of an MRI to determine injury to the medial deltoid complex.
fixation is recommended. The dynamic instability present in these injuries can be better appreciated following an external rotation stress radiograph (manual stress or gravity stress) (9, 10 and 11). During the stress test, it is important that the foot be in either neutral or slight dorsiflexion so as to not falsely reduce the radiographic medial clear space (12). Alternatively, a magnetic resonance imaging (MRI) can also show an occult deltoid ligament injury (1,13). The cost difference between a MRI and stress radiograph is substantial, and the authors do not recommend routine use of an MRI to determine injury to the medial deltoid complex.
Contralateral films should be obtained when comminution of the fibula is present. These images aid in restoring the correct fibular length and rotation thereby avoiding a malreduction. A CT scan is recommended if articular impaction is present, or further delineation of the posterior malleolar fragment is needed (14).
Open wounds should be irrigated at the bedside but will need emergent, formal I & D in the operating room. Initially, the fractures should be reduced and splinted. The majority of rotational ankle fractures are adequately reduced with longitudinal traction and rotation opposite the deforming force. A well-padded, posterior and “U” splint with the ankle in neutral dorsiflexion reduces pain and provides fracture immobilization. An adequate splint combined with judicious elevation and cryotherapy helps reduce swelling. The immediate application of a circumferential cast should be avoided. Even if nonoperative therapy is indicated, ongoing swelling can result in dangerous constriction and may exacerbate the soft-tissue injury.
While most ankle fractures requiring surgery can be treated within the first 24 hours, they do not constitute a surgical emergency. It is our practice that the isolated, closed, reduced, and splinted ankle fractures are sent home with an office appointment and subsequent surgery within 5 to 7 days. In contrast, patients with significant medical comorbidities, polytraumatized patients, or those with an emergent surgical indication (open/irreducible fracture) are admitted and have definitive operative treatment as soon as their medical condition and soft-tissue envelope allow.
It is important to ensure that the soft tissues will safely permit surgical intervention. Implementation of a staged, “damage control” protocol is indicated when the soft-tissue envelope precludes early operative intervention (Fig. 33.4) or when a reduction cannot be maintained in a splint. We recommend application of a spanning external fixator in patients with fracture blisters at the incision sites, open contaminated or degloving injuries that require multiple débridements and soft-tissue coverage, or soft-tissue swelling that is preclusive of subsequent wound closure. The external fixator stabilizes the fracture while allowing for management of soft-tissue wounds and facilitates patient mobility. Definitive fracture fixation surgery is delayed until there is
resolution of soft-tissue trauma. This is commonly judged by epithelization of fracture blisters and the presence of wrinkles on the dorsum of the foot when in neutral dorsiflexion (wrinkle sign).
resolution of soft-tissue trauma. This is commonly judged by epithelization of fracture blisters and the presence of wrinkles on the dorsum of the foot when in neutral dorsiflexion (wrinkle sign).
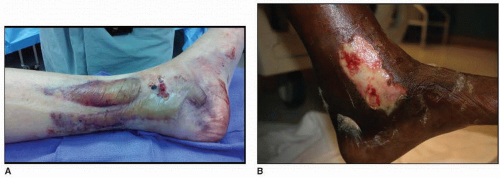 FIGURE 33.4 Clinical photographs of two ankles. (A) Trimalleolar fracture with blisters over the lateral malleolus. (B) Bimalleolar fracture dislocation with abrasions over the medial malleolus. |
We believe that many ankle fractures are regarded as “simple” fractures, and a lack of preparation can lead to unnecessary errors or poor outcomes. A clear understanding of the patient’s condition and fracture morphology is necessary for selection of correct patient positioning and operative approach.
SURGERY
Patient Positioning
Patients are most commonly positioned supine, and a general or regional anesthetic technique is utilized. A towel roll placed beneath the ipsilateral hip allows the leg to lie in neutral rotation (Fig. 33.5). A pneumatic tourniquet is applied to the upper thigh. The leg is shaved and prepped, and a sterile sheet is placed beneath the leg to prevent inadvertent contamination of surgical gowns during draping. The leg is sterilely draped free, and the toes are sealed with a plastic adhesive drape.
Prone positioning may be indicated for selected trimalleolar ankle fractures with a large, displaced posterior malleolar fracture or posterior articular impaction. With chest rolls positioned from the shoulders to the anterior superior iliac spines, care is taken to place the arms in a tension-free (90/90) position. Next, the anterior knees are padded with a foam/gel pad and the legs placed in a tension-free position with the knees slightly bent. From this position, the posterior malleolus and fibula may be fixed through a posterior-lateral approach (Fig. 33.6). Reduction and instrumentation of the medial malleolus in the prone position may be more easily performed with the knee flexed.
In closed fractures, a first-generation cephalosporin is used unless there is an allergic contraindication, in which case an alternative antibiotic is chosen. In type II or III open fractures, an aminoglycoside is added to the pre-operative antibiotic regimen.
 FIGURE 33.5 Clinical photograph of right leg on a radiolucent ramp with the leg resting in neutral rotation (patella facing the ceiling) after placement of a hip bump. |
Technique
Bony landmarks (medial/lateral malleoli and joint line) are localized and identified with a surgical marking pen. The location of the fracture can also be marked based on palpation or, if needed, fluoroscopic imaging. Surgery can be performed with or without a tourniquet. Meticulous homeostasis during the surgical approach should be obtained and typically obviates the need for a tourniquet.
In bimalleolar ankle fractures, it is the author’s preference to fix the fibula first.
MEDIAL MALLEOLAR FIXATION
Our preferred medial approach is a straight incision just anterior to the midsagittal axis of the tibia (Fig. 33.7). This incision allows inspection of distal medial tibia and the talar dome, while facilitating instrumentation of the fracture. Some may favor a curved “J” incision for better access to the ankle joint. Care must be exercised when placing the distal extent of this incision so as to not preclude access to the medial malleolus for instrumentation. As with all approaches to the medial ankle, the saphenous vein and nerve should be preserved and protected from inadvertent injury.
Adequate exposure is required to ensure an anatomic reduction. Because of the fracture orientation, anterior or posterior malreductions may not always be appreciated when inspecting the medial cortical surface. We therefore recommend exposure of the anterior articular aspect of the medial malleolus (the shoulder or axilla), which aids in assessing the reduction. In addition, visualization of the anterior malleolus will facilitate inspection of the joint surfaces. As small osteochondral abrasions or defects are not uncommon, distal retraction of the fragment allows irrigation, débridement, and inspection of the joint (Fig. 33.8). Minimal dissection of the periosteum (2 mm) is performed along the fracture edges to assess fragment interdigitation and cortical reduction.
Reduction of the medial malleolus is performed with a bone tenaculum or small (1.6 mm) Kuntscher-wires (K-wires). A small, pointed bone tenaculum can be placed on the medial malleolar fragment from anterior to posterior and used to guide the reduction. Alternatively a 1.6-mm K-wire can be placed into the lateral cortex and used as a joy-stick to guide reduction of the distal fragment. With either technique, a second pointed bone tenaculum or Weber clamp is used to hold and compress the fragment. A drill hole (2.5 mm) is placed in the intact distal medial metaphysis allowing insertion of one tine of the clamp while the other is placed around the medial malleolar fragment (Fig. 33.9). A second K-wire may be inserted across the fracture to prevent fragment rotation, at which point the first tenaculum/joy-stick can be removed.
 FIGURE 33.7 Clinical photograph of a left ankle outlining the contour of the medial malleolus and planned incision. |
 FIGURE 33.8 Retraction of the medial malleolar fragment distally allows inspection and irrigation of the ankle joint. |
Large, one-piece, medial fragments are typically secured with two 4.0 mm, partially threaded, cancellous screws. With the tenaculum centered on the fragment, a scalpel is used to split the superficial deltoid ligament in-line with its fibers. With the foot slightly everted, a 2.5-mm drill bit is placed against the anterior colliculus and directed in-line with long axis of the tibia. A second drill bit is placed in the intercollicular groove and directed parallel to the first drill bit. While placing the second screw in the posterior colliculus has been common practice, it increases the risk of injury to the posterior tibial tendon and can result in postoperative pain (15). If the size of the fragment precludes placement of two 4.0-mm screws, then alternative methods of fixation should be considered. These include a single lag screw with a K-wire, small diameter screws, or tension band wiring. Long 2.0, 2.4, and 2.7-mm screws should be available and are well suited for small medial malleolar fragments. Alternatively, tension band fixation can be performed by inserting 1.6-mm K-wires in a direction similar to the standard screw fixation. Eighteen-gauge wire or a large nonabsorbable suture is passed around the K-wires and crossed in a figure-of-eight fashion around a screw placed in the tibial metaphysis. The ends of the K-wires are then bent and impacted.
Vertical medial malleolar fractures, as commonly seen with supination-adduction injuries, deserve special attention. These fractures may be accompanied by marginal impaction of the anterior-medial plafond (16). Reduction and fixation of the impacted distal tibia joint surface is mandatory. Small osteotomes and bone tamps can facilitate anatomic restoration of the joint surface. The resulting cancellous bone void is filled with bone graft, and the medial malleolus fracture is reduced (Fig. 33.10). While vertical, shear, medial malleolar fractures can be stabilized with lag screws placed perpendicular to the fracture line, we recommend buttress plate fixation using a 1/3 tubular plate. Cortical screws can be inserted, using a lag technique through the plate for added stability (17).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree