Ankle Arthroscopy
Christopher F. Hyer DPM
Matthew M. Buchanan MD
Terrence M. Philbin DO
Thomas H. Lee MD
Gregory C. Berlet MD
History of the Technique
Ankle arthroscopy derives from early 1900s Japan when Takagi began adapting endoscopes for use in joints in the lower extremity, beginning in the knee.1 In 1925, arthroscopy was introduced in the United States, but it was not until later in the 1950s when arthroscopy technical manuals were published.2,3 In the past 30 years, however, there has been a dramatic increase in the indications and use of ankle arthroscopy as the technology and skill level of the surgeon have evolved.
Indications and Contraindications
Anterior ankle arthroscopy is both diagnostic and therapeutic for many ankle disorders. Diagnostic indications for ankle arthroscopy include unexplained symptoms of pain, swelling, or stiffness as well as in patients with symptoms unresponsive to conservative therapies. Therapeutic indications include ankle synovitis, anterolateral ankle impingement lesion, anterior bony impingement, osteochondral lesions of the talus or tibia, intra-articular loose bodies, arthrofibrosis, ankle fractures, and degenerative joint disease. Ankle arthroscopy also has a role in lateral ankle stabilization procedures and arthrodesis, as well as for irrigation and débridement of septic arthritis.
Overlying soft tissue infection is a contraindication to ankle arthroscopy. Severe degenerative joint disease and ankle malalignment are relative contraindications as they can influence the ability to establish arthroscopic portals into the ankle.
The specific conditions of ankle synovitis, anterolateral impingement lesion, anterior bony impingement, osteochondral lesions of the talus, and lateral ankle instability are specifically addressed.
Ankle Synovitis
Patients with ankle synovitis complain of global ankle pain. Most commonly, this pain is perceived across the anterior ankle joint line, but posterior pain is possible. Symptoms can be relieved with oral anti-inflammatories and with intra-articular injections, which are used to aid diagnosis as well as for symptomatic treatment. Patients may relate a history of a previous significant ankle injury that seemed to incite the current complaints. Co-morbid medical conditions such as rheumatoid arthritis often present with synovitis in the ankle.
On physical exam, there is pain with palpation along the anterior joint line and with end ranges of motion. Joint motion is typically smooth without any popping or catching. Joint laxity may be present from previous injury and an anterior drawer should be attempted. Radiographs are typically negative for synovitis, but magnetic resonance imaging (MRI) can detect inflammation of the joint lining (Fig. 65-1). Ankle arthroscopy with synovectomy is indicated if conservative therapies such as cortisone injection, physical therapy, and oral anti-inflammatories are unsuccessful and the patient continues to have pain and disability.
Anterolateral Impingement Lesion
A soft tissue impingement lesion can develop in the anterior lateral corner of the ankle joint, often after injuries such as
fracture or severe ankle sprain. Patients may point specifically to this area as the source of pain and often will perceive a catching or clicking. On exam, maximal dorsiflexion and deep palpation to the anterior lateral corner of the ankle joint reproduces the pain. The “charger” stance, with the patient weight bearing, flexing the knee, and keeping the heel flat on the ground, also will produce pain in this corner of the ankle (Fig. 65-2). Radiographs are typically negative for soft tissue impingement lesions. MRI can detect a focal impingement lesion at the anterolateral corner, particularly on the T2 or SPIN images, when fluid outlines the abnormal soft-tissue structure.4 Ankle arthroscopy with débridement of the anterolateral impingement lesion is indicated if conservative therapies such as cortisone injection, physical therapy, and oral anti-inflammatories are unsuccessful and the patient continues to have pain and disability.
fracture or severe ankle sprain. Patients may point specifically to this area as the source of pain and often will perceive a catching or clicking. On exam, maximal dorsiflexion and deep palpation to the anterior lateral corner of the ankle joint reproduces the pain. The “charger” stance, with the patient weight bearing, flexing the knee, and keeping the heel flat on the ground, also will produce pain in this corner of the ankle (Fig. 65-2). Radiographs are typically negative for soft tissue impingement lesions. MRI can detect a focal impingement lesion at the anterolateral corner, particularly on the T2 or SPIN images, when fluid outlines the abnormal soft-tissue structure.4 Ankle arthroscopy with débridement of the anterolateral impingement lesion is indicated if conservative therapies such as cortisone injection, physical therapy, and oral anti-inflammatories are unsuccessful and the patient continues to have pain and disability.
 Fig. 65-1. T2 MRI. Sagittal plane image of anterior ankle synovitis with joint effusion. White arrow indicates area of effusion. |
Anterior Ankle Bony Impingement
Often called “footballers ankle,” this bony impingement is a source of decreased ankle dorsiflexion and anterior ankle pain.5 Limited ankle dorsiflexion is found on exam with a “bony end feel” or abrupt end to the range of motion (Fig. 65-3). Anterior bony impingement lesions occur most commonly in the athletic population, particularly dancers, soccer, football, and basketball players.6 Anterior ankle capsular strain from forced plantarflexion with resultant calcific deposits or repetitive dorsiflexion, resulting in subchondral injury and new bone formation, are both possible mechanisms of anterior exostoses.6,7 The chronically unstable ankle often develops anterior bony exostoses, which may represent capsular strain from rotational instability. These spurs are offset with the talar spur anteromedial and the tibia spur anterolateral8 (Fig. 65-4). “Kissing” spurs can occur with degenerative joint disease with the tibial and talar spurs directly impinging, although there is no conclusive evidence that chronic ankle
instability leads to degenerative joint disease.9 Radiographs can illustrate the orientation of the spurs, particularly if an oblique lateral view is used.10 If further workup is necessary, computed tomography (CT) scan is recommended to fully evaluate the orientation of the bony impingement. Ankle arthroscopy with decompression of the anterior bony impingement is indicated if conservative therapies such as cortisone injection, physical therapy, and oral anti-inflammatories are unsuccessful and the patient continues to have pain and disability. Large exostoses are a relative contraindication due to the technical difficulty associated with a minimally invasive procedure.
instability leads to degenerative joint disease.9 Radiographs can illustrate the orientation of the spurs, particularly if an oblique lateral view is used.10 If further workup is necessary, computed tomography (CT) scan is recommended to fully evaluate the orientation of the bony impingement. Ankle arthroscopy with decompression of the anterior bony impingement is indicated if conservative therapies such as cortisone injection, physical therapy, and oral anti-inflammatories are unsuccessful and the patient continues to have pain and disability. Large exostoses are a relative contraindication due to the technical difficulty associated with a minimally invasive procedure.
Osteochondral Lesions of the Talus
Osteochondral lesions of the talus (OLT) are most commonly attributed to trauma either acute or remote in nature.11,12,13 Lateral and medial talar dome lesions are unique and distinct from one another. Lateral talar dome lesions are more likely from acute trauma.14,15 The mechanisms of injury of lateral lesions are dorsiflexion and inversion, in which the anterolateral aspect of the talus impacts the fibula (Figs. 65-5, 65-6, 65-7). These anterolateral lesions typically are thin and waferlike in appearance.
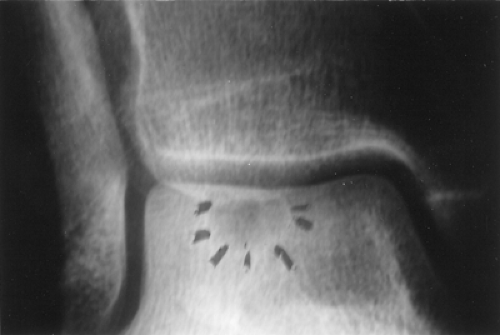
 Fig. 65-5. Anterior-posterior (AP) radiograph of intact anterolateral osteochondral lesion of the talus (OLT). |
 Fig. 65-6. Lateral radiograph of intact anterolateral OLT. The lesion is a subtle finding in this view. |
Medial lesions result from combined inversion, plantar flexion, and external rotational forces. The medial lesion is caused by the posteromedial talar dome impacting the tibial articular surface and is typically deep and cup-shaped. The results of several biomechanical studies indicate that a
repetitive overuse syndrome may also be responsible for medial lesions.16
repetitive overuse syndrome may also be responsible for medial lesions.16
 Fig. 65-7. T2 MRI. Coronal plane image of intact anterolateral OLT from Fig. 65-5. Marrow edema is noted beneath the lesion within the talus. |
 Fig. 65-8. AP radiograph of central-medial (arrow) OLT. This demonstrates the sometime subtle findings seen on plain film studies. |
 Fig. 65-9. T1 MRI. Axial plane image of central-medial OLT from Fig. 65-8. |
Patients may complain of generalized ankle tenderness that is worse with weight bearing and activity. A history of prior injury may be given, but often is not recalled by the patient. A catching or locking sensation may be perceived if there is a loose chondral flap or free floating loose body. Often, there is the overlying pain of ankle synovitis or an anterolateral impingement lesion that can cloud the diagnosis. Radiographic evaluation of the ankle can reveal osteochondral lesions, but findings can be subtle. MRI is helpful in identifying injuries of the subchondral bone and cartilage and precisely locating the lesion (Figs. 65-8, 65-9, 65-10, 65-11). Staging of the lesion is performed according to one of several classification systems published previously.17,18 The classification described by Hepple et al.18 incorporates MRI findings. Stage 1 represents articular cartilage damage only. Stage 2a is cartilage injury with underlying fracture and edema. Stage 2b is the same as stage 2a without the edema. In Stage 3, the fragment is detached (rim signal) but not displaced. In stage 4, the fragment is displaced, and stage 5 shows subchondral cyst formation.
Arthroscopic treatment of OLT depends on the lesion itself. In acute chondral fractures, where significant bone remains attached to the chondral flap, securing the OLT back to the talar dome using absorbable fixation can be performed with arthroscopic visualization and débridement of interposed tissue.
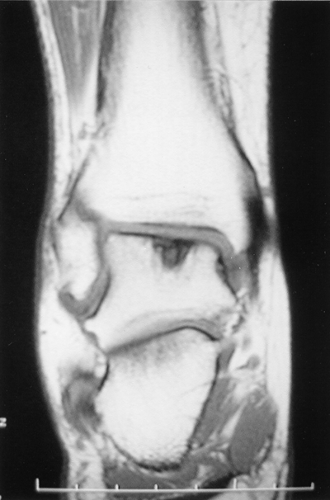 Fig. 65-10. T1 MRI. Coronal plane image of central-medial OLT from Fig. 65-8. |
 Fig. 65-11. T1 MRI. Sagittal plane image of central-medial OLT from Fig. 65-8. |
In older lesions, removal of loose bodies with débridement and microfracture techniques stimulate development of fibrocartilage. The microfracture technique entails perforating subchondral bone and creating vascular access channels to release substances such as mesenchymal stem cells and growth factors to promote new tissue formation. Ultimately, fibrocartilage can form and fill the original defect. The excision, curettage, and microfracture technique has a success rate of 85% in a meta-analysis of the literature.19
In OLTs with an intact cartilage cap and subchondral cystic formation, retrograde drilling of the defect may be possible (Figs. 65-12, 65-13). For medial lesions, the drilling begins laterally from the sinus tarsi and is used to perforate the subchondral cyst. The drill path supplies a route for revascularization and the cyst is back filled with bone graft or bone graft substitute. A cannulated system facilitates easy and accurate positioning of the drill hole and provides a delivery cannula for bone graft substitute or autograft. Arthroscopy is used to monitor the integrity of the cartilage cap during the procedure and ensure that bone graft does not enter the joint. As the bone fills the cystic void, the cartilage cap is anchored to the subchondral plate.
Ankle arthroscopy with treatment of the OLT is indicated if conservative therapies such as immobilization, physical therapy, and oral anti-inflammatories are unsuccessful and the patient continues to have pain and disability. Surgical treatment is also indicated in stage 3 and 4 lesions in which loose bodies or chondral flaps are already present.
Chronic Ankle Instability
Ankle sprains are common injuries, occurring in an estimated one out of 10,000 persons per day.20 The anterior talofibular ligament (ATFL) is the most commonly injured ligament during ankle sprains. It serves as the primary restraint to inversion and translation of the talus within the ankle mortise. During an inversion ankle sprain, the anterolateral capsule is typically injured first, followed by the ATFL, calcaneal fibular ligament (CFL), and posterior talofibular ligament (PTFL).
The majority of acute ankle sprains heal with physical therapy/ankle rehabilitation; however, approximately 29% to 42% of patients experience chronic functional ankle instability.21 Chronic lateral ankle instability is defined as instability for greater than 6 months with repeated episodes of “giving out,” persistent pain, and inability to resume preinjury activity levels.22 Physical exam will reveal laxity of the ATFL with a positive anterior drawer on the affected ankle as compared to the contralateral side. An anterior drawer maneuver that reveals anterior subluxation of the talus on the tibia
greater than 4 mm as compared with the contralateral side is considered indicative of ATFL laxity or rupture. Diminished ankle proprioception is frequently seen in chronic instability. To test proprioception, have the patient in a single limb stance close his or her eyes for 20 seconds and maintain balance. The patient should be able to do this without assistance and recover balance if you lightly push him or her. Functional instability fails to demonstrate gross ankle laxity, but the patient perceives instability and is unable to trust the ankle. Neuromuscular deficits are present in proprioception, muscle strength, muscle reaction time, and postural control.
greater than 4 mm as compared with the contralateral side is considered indicative of ATFL laxity or rupture. Diminished ankle proprioception is frequently seen in chronic instability. To test proprioception, have the patient in a single limb stance close his or her eyes for 20 seconds and maintain balance. The patient should be able to do this without assistance and recover balance if you lightly push him or her. Functional instability fails to demonstrate gross ankle laxity, but the patient perceives instability and is unable to trust the ankle. Neuromuscular deficits are present in proprioception, muscle strength, muscle reaction time, and postural control.
 Fig. 65-13. T1 MRI. Coronal image of cystic OLT with an apparent intact cartilage cap from Fig. 65-12.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|