CHAPTER 8 Anesthesia for Shoulder Procedures
This chapter covers unique aspects of anesthesia care as it relates specifically to shoulder surgery. The role of the interscalene brachial plexus nerve block—its indications, contraindications, benefits, and complications—in the intraoperative and postoperative care of patients undergoing shoulder procedures is central to the discussion. Developments in the use of ultrasound (US) guidance for performing interscalene brachial plexus block and advances in continuous catheter techniques are reviewed. Issues pertinent to the preoperative, intraoperative, and postoperative phases of anesthetic care for shoulder surgery are examined.
In 1884, Halsted1 produced the first regional block of the upper extremity by injecting cocaine onto the roots of the brachial plexus under direct vision. In 1911, Hirschel2 described the first percutaneous axillary block; this same year Kulenkampff3 attempted a supraclavicular approach to local anesthetic block of the brachial plexus.
Etienne4 in 1925, Burnham5 in 1958, and Winnie and Collins in 19646 contributed to the development of the subclavian perivascular technique involving a single injection using a supraclavicular approach. This approach risked puncture of the subclavian artery and the lungs. Although satisfactory for the arm, the axillary, supraclavicular, and subclavian perivascular techniques did not provide good anesthesia for shoulder surgery unless dangerously large volumes of local anesthetic were used. In 1970, Winnie developed the interscalene approach, using smaller volumes of local anesthetic injected into the brachial plexus sheath at the level of the sixth cervical vertebra. This approach produced excellent anesthesia for the shoulder.4
ANESTHESIA
Choice of Anesthesia: Regional Versus General
The alternatives to regional anesthesia for shoulder procedures are general anesthesia or a combination of the two techniques. When compared with general anesthesia, interscalene brachial plexus block has been shown to optimize operating conditions, reduce postoperative pain, decrease postoperative nausea and vomiting, reduce postoperative anesthesia care unit stay, and, in the ambulatory setting, minimize unplanned hospital admissions.7–18
Interscalene blocks can be used alone (patient awake), with sedation (light or heavy), or with a general anesthetic (laryngeal mask airway or endotracheal tube). Studies from university medical centers and community-based practices estimate the success rate of the blocks to be 81% to 100%, with the majority reporting rates around 95%.8–10,13,17,19–27 Success in these studies has been variably defined according to the anesthetic goal for the block, that is, either as a primary anesthetic or as effective postoperative analgesia. The goals may be different for outpatient arthroscopic surgery when compared to major open inpatient procedures, such as arthroplasty.
In experienced hands, regional anesthesia can provide significant advantages to the patient having shoulder surgery, with low rates of significant long-term complications.8,17,19,20,23,26,28–30 Advantages claimed for an interscalene brachial plexus block over a general anesthetic include decreased blood loss, decreased postoperative analgesia requirements, and avoidance of the risks and side effects of general anesthesia.11,12,16,17,22,31 The decreased blood loss reported is postulated to be due to the dilation of capacitance vessels coupled with blood drainage away from the wound in the semi-sitting position. This mechanism is speculative,17,32 based on the assumption that a successful interscalene brachial plexus block causes a sympathectomy, similar to the effects of spinal and epidural anesthesia in lower-extremity surgery. Interscalene block has been shown to provide adequate muscle relaxation, and some view it as superior muscle relaxation when compared with systemic muscle relaxants because it does not fluctuate like the degree of intravenous (IV) pharmacologic neuromuscular blockade.26,32
Initiating the interscalene block in a preoperative holding area can improve cost containment and efficiency by reducing the nonoperative time in the operating suite. Conversely, a survey of orthopaedic surgeons indicated that when regional anesthesia is not efficiently integrated into the perioperative care process, the resulting delay in the operating room schedule is one of the primary reasons for not favoring regional techniques.33
Postoperatively, the length of stay in the postoperative anesthesia care unit and unplanned admissions for pain, sedation, nausea, vomiting, and urinary retention can be decreased.10–12,16,31,34 Better postoperative pain control facilitates outpatient surgery and allows earlier mobilization and physical therapy.11,12,14 Anecdotally, in our institution interscalene blocks facilitate immediate postoperative use of continuous passive movement machines and, to a lesser extent, immediate postoperative physical therapy.
Other advantages of regional anesthesia over general anesthesia might exist in some patients with serious underlying medical conditions. Changes in physiologic function of major organ systems can often be avoided using regional anesthesia. A number of investigators have documented that a general anesthetic is unnecessary in the presence of a successful regional anesthetic block.10–12,15,19,26,31
Patient refusal is an absolute contraindication to regional anesthesia. Surgical concerns can also militate against having the patient awake during surgery. Other contraindications to regional anesthesia of the shoulder include impaired coagulation and infection at the site of the block. Preexisting nerve deficits on the side of the intended nerve block could be considered relative contraindications to a block, in part because theoretically there is a potential for increased vulnerability to nerve injury. The loss of the ability to test nerve function immediately after the surgery may be considered a relative contraindication for some patients and procedures, particularly in the operative treatment of fractures at sites of nerve vulnerability. Significantly impaired pulmonary function is also a contraindication because typically the interscalene block reduces diaphragmatic excursion and vital capacity by 20% to 40%.35,36 Patients with minimal respiratory reserve may be unable to tolerate this transient reduction in respiratory function.
Technique: Interscalene Brachial Plexus Block
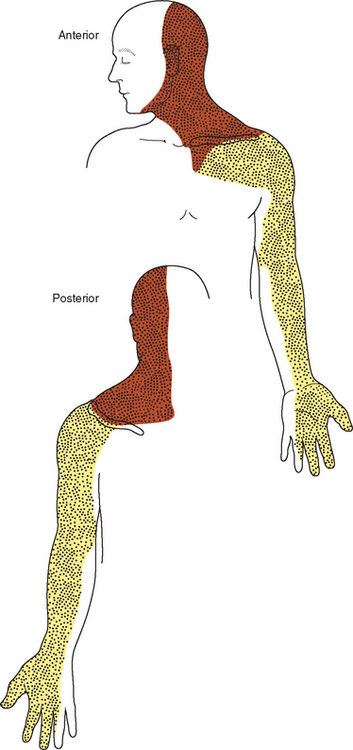
The superficial cervical plexus is composed of cervical nerves one through four and innervates parts of the anterior shoulder. The superficial cervical plexus can be blocked selectively with a field block at the posterior border of the sternocleidomastoid muscle.37 Figure 8-1 demonstrates the distribution of cutaneous analgesia after an interscalene block and a superficial cervical plexus block.
Before a block is performed, the patient must have IV access and appropriate monitoring including electrocardiogram, noninvasive blood pressure, and continuous pulse oximetry. Interscalene blocks can be performed in a block room, a preoperative holding area, or the operating room. Specific requirements for the area include an oxygen source, a bag valve mask, suction, standard airway equipment (e.g., oral airway, mask, laryngoscope, endotracheal tube), and emergency drugs immediately available (including an induction agent and a muscle relaxant).
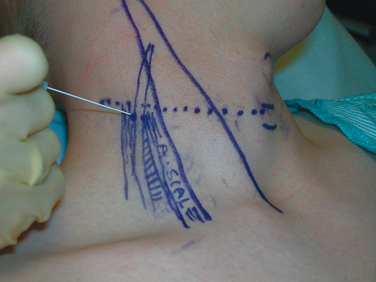
In addition to the technique originally published by Winnie in 1970 (Fig. 8-2), Borgeat and Meier have described a modified lateral approach to the interscalene brachial plexus,19,38 and Boezaart has published a description of a posterior paracervical approach.39 The authors assert that these techniques are superior to the Winnie technique for placing catheters and for avoiding injections and needle trauma to the cervical cord.
Another significant addition to the choice of techniques is US guidance for performing interscalene brachial plexus blocks. The preference for the needle insertion site and nerve localization technique (nerve stimulator, paresthesia technique, or US guidance) depends on the skills and experience of the operator. The literature consists primarily of case series reporting on a single block technique, and the very limited number of head-to-head comparisons of techniques does not conclusively demonstrate an advantage with regard to the safety and the success of one technique over the others.17,24,30,38,40–48 Due to the relatively uncommon occurrence of significant complications with interscalene block and with published success rates in the most experienced hands of 95%, studies examining the techniques have been underpowered to adjudicate between techniques on the issues of safety and efficacy.
Even in the absence of conclusive data, there are reasons to reconsider the use of the paresthesia technique. This technique does not provide any information to the practitioner about the relative distance between the needle and the plexus, because the paresthesia either is there or it isn’t. If the plexus is not encountered on the first needle pass, there is limited information on which to base a new search pattern for the nerves. The technique also involves intentionally eliciting a response that most patients would describe as uncomfortable, if not painful. The specific neurophysiologic event corresponding to the paresthesia is not known because it does not necessarily correlate with other markers of nerve-to-needle proximity, such as nerve stimulation at a current of 0.5 mA or US-visualized position of the needle tip.40,47,48 Finally, it does not provide information that will guide the insertion of continuous interscalene catheters.
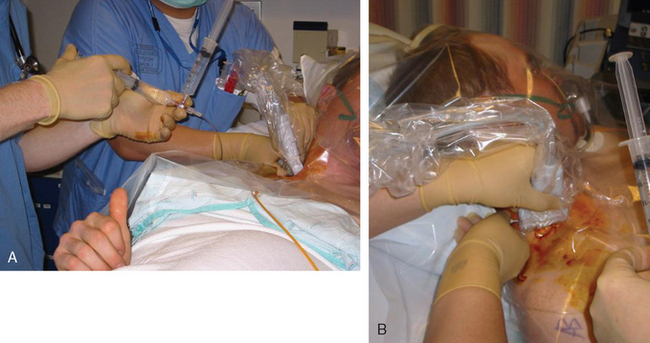
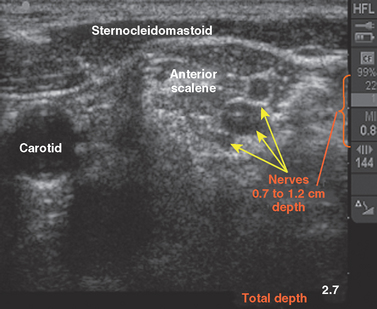
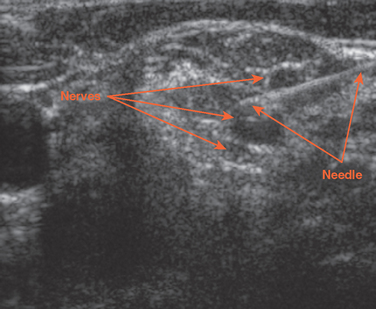
At this early stage of its application for nerve blocks, US guidance, either added to peripheral nerve stimulation or on its own, appears to be at least comparable in efficacy to the PNS technique, with potential for further safety advantages.49–51 For performing interscalene blocks, a linear US transducer with an upper range of 10 to 13 MHz combines good image resolution and adequate penetration depth. US guidance enables the practitioner to visualize needle and nerve proximity and monitor the spread of local anesthetic in real time, adding an extra margin of protection against problems caused by anatomic variation that might result in a failed block or intravascular injection. In both the paresthesia and nerve-stimulator techniques, the practitioner has information about the relationship between the needle and the nerve at the initiation of the injection but no information about any subsequent movement of the needle and the spread and deposition of the anesthetic, both of which are provided by US guidance (Figs. 8-3 to 8-5).52
The shortcomings of US guidance relate primarily to the expense of purchasing a high-resolution US machine and the possibility that practitioners experienced with other techniques might find that the time required to complete a block is increased during the early stages of learning the new technique. Because of the relative infrequency of significant complications, a very large trial would be needed to definitively determine whether the theoretical safety advantage for the use of US could be conclusively demonstrated.52,53
For the Winnie technique, after locating the interscalene groove, a needle is advanced perpendicular to the skin in all planes and into the groove in a slightly caudal direction to locate the brachial plexus.4 The modified lateral technique involves the use of the same needle insertion site, but the needle is directed toward the junction of the medial and lateral third of the clavicle at a 45- to 60-degree angle to the skin.19,38 Boezaart’s posterior cervical approach involves the use of a Tuohy needle and a loss-of-resistance technique in conjunction with peripheral nerve stimulation.39 A variety of needles are available for performing the block. B-bevel (19-degree angle), short bevel (45-degree angle), or pencil-point needles are preferred over standard A-bevel (cutting) needles.54
With the PNS technique, an insulated needle with a nerve stimulator is used to determine optimal needle placement by demonstrating upper arm or forearm muscle twitching. When optimal needle placement is achieved, the needle is then held fixed by the operator while an assistant aspirates for blood. Having the needle attached to the syringe by extension tubing facilitates immobility of the needle during injection. If aspiration is negative, 1 mL of local anesthetic is then injected as a test dose. If there are no signs or symptoms of intra-arterial injection (transient nausea, dizziness, slurred speech, sedation, loss of consciousness, or grand mal seizures),55–57 continued aspiration alternating with injection of 3 to 5 mL of local anesthetic solution needs to be repeated to a final volume of 20 to 40 mL total.
After the extent of the block is determined, it might have to be supplemented with a superficial cervical block.25 From our experience and studies examining distribution of the interscalene block, it is more likely that when a block is used as the primary anesthetic for major open procedures, it will require supplementation to cover the T1-T2 dermatomes that can extend into the area of a deltoid–pectoral incision.25,58,59 This can be accomplished through additional local anesthetic infiltration by the surgeon or through thoracic paravertebral blocks at the appropriate levels.25,58
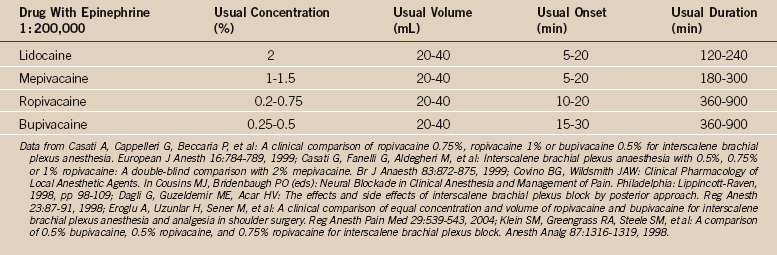
The choice of local anesthetic to be used is based on the desired duration of the block, density of the block, time to onset, and the toxicity profile (Table 8-1). This decision can also be influenced by whether the interscalene block is the primary anesthetic or is used for postoperative pain control only. For single-shot analgesic blocks, concentrations of 0.125% bupivacaine or 0.2% ropivacaine appear adequate, whereas 0.375% to 0.5% bupivacaine and 0.5% to 0.75% ropivacaine may be required to provide a block appropriate for surgical anesthesia in an awake or lightly sedated patient. A perineural catheter has the advantage of allowing the use of an intermediate-acting anesthetic, such as lidocaine or mepivacaine, for denser intraoperative anesthesia, with the opportunity to transition to motor activity–sparing concentrations of bupivacaine or ropivacaine postoperatively.
Complications of Interscalene Brachial Plexus Block
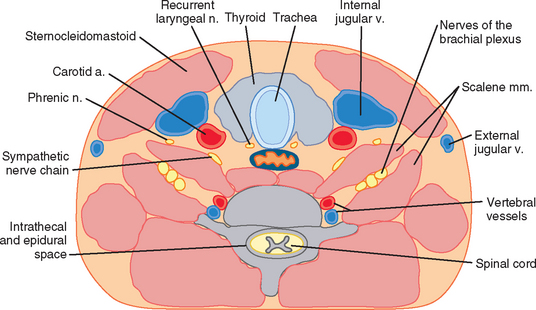
Complications due to interscalene block can be separated into expected transient, associated effects (ipsilateral hemidiaphragmatic weakness, Horner’s syndrome, hoarseness); shorter term, treatable complications (respiratory failure due to hemidiaphragmatic weakness, pneumothorax, seizures, central nervous system local anesthetic effects); and untreatable complications (peripheral nerve injury, central nervous system injury, brachial plexitis). Figure 8-6 shows a cross section of the neck at the C6 level emphasizing the structures that are vulnerable during interscalene block.
An obvious but important consideration that applies to interscalene block anesthesia (and any other medical intervention) is that the results from centers that have the necessary case load and interest in publishing studies are in part due to the techniques used and in part due to a concentration of expertise and experience. The published results might not be readily realizable in all centers. Lenters and colleagues reported on complications associated with interscalene blocks, noting a very strong inverse association between the experience of the anesthesiologist and the frequency of complications.60 Weber and Jain published a study in the orthopaedic literature with a lower success rate and higher rate of complications than other series, demonstrating variability in the success of the technique.27 The exchange in the letters to the editor following the publication of this retrospective series confirmed that an anesthesiologist’s and surgeon’s thoughts on the risks and benefits of interscalene blocks are strongly influenced by their direct experience with or knowledge of significant complications that have occurred with their use and are not necessarily determined by the optimal published data in the literature.22
Transient Associated Effects
It is useful to forewarn patients of the potential for ipsilateral hemidiaphragmatic weakness, Horner’s syndrome, and hoarseness to avoid undue concern. These effects usually have minimal clinical significance and are considered normal sequelae of the block.26,59,61 The phrenic nerve, originating with the C4 nerve root and lying on the anterior surface of the anterior scalene muscle, is blocked in 100% of patients receiving an interscalene block.35,36,62,63 Ipsilateral hemidiaphragmatic paresis has an onset of 5 to 30 minutes from the initiation of the block and lasts for the duration of the motor block. Occasionally, patients have a subjective awareness of mild shortness of breath. This is usually not a problem, but it could become so in patients with severe respiratory disease, obesity, or advanced pregnancy.
Horner’s syndrome, due to blockade of the cervical sympathetic nerve, occurs in 18.5% to 75% of patients64,65 and results in ipsilateral ptosis, miosis, anhidrosis, and nasal congestion for the duration of the block. Cases of prolonged Horner’s syndrome have been reported following interscalene block.64,66
Recurrent laryngeal palsy is less common.59,65 It causes ipsilateral vocal cord paralysis and hoarseness. Patients with preexisting contralateral vocal cord paresis are at risk for bilateral vocal cord paralysis and possible complete airway obstruction due to unopposed adduction of the cords.67
Finally, subtle and temporary auditory disturbances, possibly due to an indirect effect of blockade of the cervical sympathetic chain, have been reported in patients receiving an interscalene block.32
Short-Term, Treatable Complications
Interscalene blocks are not recommended in patients unable to tolerate a 25% to 30% reduction in pulmonary function,35,43 for example, patients with contralateral diaphragm dysfunction or those dependent on intact bilateral diaphragmatic function (ankylosing spondylosis). The potential for subclinical left hemidiaphragm weakness exists after coronary artery bypass graft surgery with left internal mammary artery dissection.62 There is a paucity of data that would enable the practitioner to predict which patients will not tolerate the hemidiaphragmatic paresis.
When an interscalene block is considered to be particularly beneficial for patients at higher risk for respiratory failure, a continuous catheter with careful induction of the block and using shorter-acting local anesthetics needs to be considered, rather than a single shot of a long-acting local anesthetic. This can shorten the period of respiratory distress and ventilator dependency if the diaphragmatic paresis from the block is not tolerated. In patients with severe pulmonary compromise, the relative risk of general anesthesia versus an interscalene block is not clear. A detailed discussion concerning the risk of respiratory failure is initiated with the patient and the surgeon regarding an immediate respiratory rescue plan including noninvasive ventilator support and sedation for intubation and ventilation. One case of persistent phrenic nerve palsy has been reported.68
Pneumothorax is more common with the supraclavicular approach,63 but it can occur following interscalene block.20,59,63,69 It is best seen on an upright chest x-ray during full expiration and is part of the differential diagnosis of dyspnea, chest pain, or persistent oxygen saturations below 95% in room air (or 5% below baseline) following interscalene block. Bronchospasm also has been reported in asthmatic and nonasthmatic patients having interscalene blocks and has been attributed to sympathetic blockade with unopposed vagal activity.70,71
Inadvertent intrathecal, epidural, or subdural blocks are rare but can occur during attempted interscalene block, causing apnea and hemodynamic instability and necessitating emergency intubation, ventilation, and cardiovascular support until the block resolves.72–81 Emergency drugs and airway equipment always must be close at hand. Possible mechanisms for these problems include direct injection into the intrathecal, epidural, or subdural space secondary to incorrect needle placement, prevertebral spread of injected drug, or injection into an abnormally long dural root sleeve. There has been one reported case of inadvertent epidural catheter placement while placing a continuous interscalene block.82 Bilateral interscalene block without evidence of central spread has also been reported.60
Many blood vessels are present near the injection site. Intravascular injection of a small volume of local anesthetic into the vertebral or carotid artery will cause seizures.56,57 Negative aspirations for blood before injection and repeated several times during injection should further reduce the incidence of this uncommon complication. Theoretically, injection of local anesthetic with US guidance while monitoring the spread of local anesthetic could also reduce the incidence of misdirected injections.
Although rare, cardiac arrest and transient carotid bruit have both been reported following interscalene block.74,83 Vasovagal episodes, manifesting with profound hypotension and bradycardia, are more common and are thought to be due to activation of the Bezold–Jarisch reflex, with patients in the sitting position.61,84 Usually this response is transient and relatively insignificant if diagnosed and treated promptly with atropine, glycopyrrolate, or ephedrine. If it is undetected, cardiac arrest can ensue. Prophylaxis with an IV β-blocker can prevent vasovagal episodes in this setting.85
NEUROLOGIC INJURY AFTER SHOULDER PROCEDURES
Peripheral nerve injury following shoulder surgery usually becomes apparent once the patient is awake or the interscalene brachial plexus block has resolved. In some patients, symptoms are delayed. Many factors are considered when trying to determine the etiology of the injury (Box 8-1). A preoperative evaluation noting and documenting preexisting neurologic deficits is crucial in differentiating preoperative and postoperative nerve deficits.
BOX 8-1 Risk Factors Contributing to Perioperative Nerve Injury
Adapted from Neal JM, Hebl JR, Gerancher JC, Hogan QH: Brachial plexus anesthesia: Essentials of our current understanding. Reg Anes Pain Med 27:402-428, 2002.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree