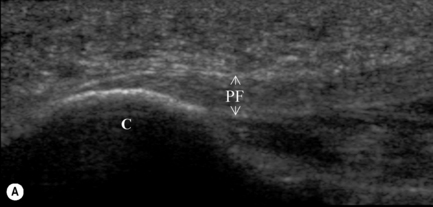
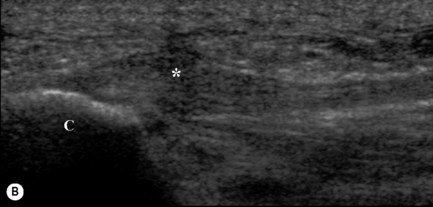
5.9 Anatomy of the plantar fascia The plantar fascia, or plantar aponeurosis, forms part of the deep fascia of the sole of the foot and provides a strong mechanical linkage between the calcaneus and the toes. Arising predominantly from the calcaneal tuberosity, the plantar fascia attaches distally, through several slips, to the plantar aspect of the forefoot as well as the medial and lateral intermuscular septa. Anatomically, the fascia can be divided into three bands: the medial, lateral, and central. While the medial and lateral bands are variable in nature, the central aponeurotic band represents the major component of the plantar fascia both structurally and functionally and is often cited as the plantar fascia proper (Sarrafian 1983). The apex of the plantar fascia proper originates from the plantar aspect of the medial process of the calcaneal tuberosity, where its deep surface also serves as a partial origin for the flexor digitorum brevis. At the mid-metatarsal level, the plantar fascia separates into five longitudinally orientated bands, with each band subsequently dividing to form superficial and deep tracts just proximal to the metatarsal heads. While the two marginal superficial tracts course obliquely to the sides of the foot, the central superficial tracts insert into the skin, anterior to the metatarsal heads and contribute to the formation of the mooring and natatory ligament (Sarrafian 1983). The five strong deep tracts of the central band bifurcate to form medial and lateral sagittal septa, which course anteriorly and deeply to surround the medial and lateral aspect of the digital flexor, before inserting sequentially into the flexor tendon sheath, interosseous fascia, the fascia of the transverse head of the adductor hallucis, the deep transverse metatarsal ligament, and the base of the proximal phalanges via the plantar plate and collateral ligaments of the metatarsophalangeal joints. The most medial pair of septa also insert into the tibial and fibular sesamoids as well as the two heads of the flexor hallucis brevis muscle. By effectively spanning both the medial and lateral longitudinal arches of the foot, the plantar fascia maintains the height of the longitudinal arch in humans. The plantar fascia supports the longitudinal arch of the foot during static stance. Metatarsal splaying and a deterioration in arch shape occur with sectioning of the plantar fascia during simulated static stance (Ker et al. 1987), suggesting that the plantar fascia forms part of a transverse and longitudinal tie-bar system within the foot. During static stance, the medial longitudinal arch has been likened to a truss, with the plantar fascia acting as a tension element, or tie-bar, connecting two compressive elements (Hicks 1955). With weightbearing and internal tibial rotation, elongation of the arch is restricted, in part, by tension within the plantar structures (Sarrafian 1987). While all of the plantar ligaments appear important in restricting movement, Huang et al. (1993), demonstrated that the plantar fascia provided the largest contribution to arch maintenance, with plantar fasciotomy resulting in a 25% reduction in the stiffness of the arch. Interestingly, however, the arch retained 65% of its original stiffness following resection of the long and short plantar ligaments, the spring ligament and the plantar fascia, suggesting that other structures, such as bone geometry, may have the greatest effect on the stability of the medial longitudinal arch during static stance. Nonetheless, during static stance, the plantar fascia is thought to form part of a passive mechanism that is capable of modifying the stiffness of the medial longitudinal arch in relation to the applied load. Under nonweightbearing conditions, dorsiflexion of the toes has been shown to increase tension within the plantar fascia, resulting in plantarflexion of the corresponding metatarsals and raising of the medial longitudinal arch; the so-called windlass mechanism (Hicks 1954). Under weightbearing conditions, however, such as during static stance, plantarflexion of the metatarsals is resisted by ground reaction force, and elevation of the arch is achieved by a complex movement of supination and external rotation of the foot and lower limb. Such a movement pattern is thought to increase the stability of the arch and activation of the windlass mechanism is clinically believed to be important during the propulsive period of gait. When toe dorsiflexion is coupled with calf muscle activity, as occurs during terminal stance, internal loading of the plantar fascia may be effectively amplified. Carlson et al. (2000) noted that dorsiflexion of the first metatarsophalangeal joint beyond 30° induced fascial loads in excess of those of the Achilles tendon when terminal stance (45% of the gait cycle) was simulated by applying loads of up to 500 N through the Achilles tendon. While the findings are consistent with motion analysis studies in which approximately 20° of hallux dorsiflexion has been shown to occur before an increase in arch height (windlass mechanism) is evident, the model did not consider the arch-supporting effect of the intrinsic and extrinsic flexor muscles of the foot. The long digital flexors, and in particular the tibialis posterior, have been shown to exert an arch-supporting influence during quasistatic testing (Kitaoka et al. 1997), which is further amplified once the heel is elevated from the support surface (Sharkey et al. 1998). Moreover, the increase in arch height associated with the windlass effect during gait has been reported to coincide with peak intrinsic muscle activity, reduced activity in the gastroc-soleus complex, reduced vertical loading, ankle plantarflexion, peak horizontal propulsive force, and the onset of double limb support. Collectively, these factors would act to minimize the internal loading of the plantar fascia (Wearing et al. 2006). Thus, rather than producing an arch-raising (windlass) effect, the plantar fascia may be alternately viewed as a dynamic coordinator of movement, effectively synchronizing digital dorsiflexion with supination of the foot and external rotation of the leg. The role of the plantar fascia during gait has largely been inferred from static loading of cadaver specimens and few studies have evaluated the internal loading of the plantar fascia during dynamic activities such as walking and running. Scott & Winter (1990) employed a two-dimensional, four-segment model of the lower extremity, in which plantar fascia was assumed to account for 50% of the bending moment at the midtarsal joint during running. Peak fascial loads in the order of 2.8 times bodyweight were predicted during the midstance and early propulsive periods of gait. Giddings et al. (2000) predicted comparable fascial loads (1.8 and 3.7 times bodyweight) during walking and running using a two-dimensional, three-segment finite-element model of the foot in which the orientation and movement of osseous segments were obtained from cineradiography. While internal stress was noted to peak late in stance (60–70%), the predicted loads from both studies exceeded the ultimate tensile strength (1189 ± 244 N) reported for human bone–plantar–fascia–bone preparations during load-to-failure testing (Kitaoka et al. 1994). Erdemir et al. (2004) estimated considerably lower peak fascial loads (538 ± 193 N) during simulated walking, which occurred at 80% stance and were equivalent to 47% of the force applied to the Achilles tendon (1041 ± 213 N), and approximately 40% of the ultimate tensile strength of the plantar fascia (1372 ± 347 N). The findings suggest that the plantar fascia has a strength–safety factor of approximately 2.5, comparable to the ACL (2.4), but considerably lower than bone (~ 6) and most animal tendons (~ 8), even high-stress tendons in which recovery of elastic strain energy is believed to be important (~ 2–4) (Frost 2001). However, these models have failed to consider the influence of intrinsic foot muscles on the internal loading of the plantar fascia. The intrinsic muscles are anatomically well positioned to reduce fascial loading and, although normally quiescent during static bipedal stance, they have been reported to be active throughout the midstance and propulsive periods of gait. The plantar fascia has been viewed by some as a purely tensile structure and the organization of collagen within the midsubstance supports such a hypothesis. However, the midsubstance of the plantar fascia does not attach directly to the calcaneus but, rather, a zone of uncalcified and calcified fibrocartilage is interposed between the midsubstance and bone proper. While such attachments are thought to provide a gradual transition from hard to soft tissue that assists with the dissipation of stress, fibrocartilage is typically found at sites within tendons and ligaments that are subjected to bending, shear or compressive forces, or their combination (Benjamin & Ralphs 1998). Given that the calcaneal attachment of the plantar fascia also serves as the origin of the flexor digitorum brevis muscle, the enthesis is likely exposed to bending, shear, and compression forces, which may predispose the attachment to injury (Wearing et al. 2006). Plantar fasciitis is the most common disorder of the foot, affecting 10% to 20% of injured athletes (Rome 1997). The overall prevalence, however, is unknown, as plantar fasciitis predominantly occurs in sedentary, middle-aged individuals and may increase with senescence. Similarly, little is known regarding the clinical course of plantar fasciitis. Although 5 to 10% of sufferers progress to surgery, the majority ostensibly resolve within 6 to 18 months of the initiation of conservative therapy, leading some to suggest that plantar fasciitis is a self-limiting condition. Radiographic examination may demonstrate the presence of an inferior calcaneal spur of unknown significance. Although bony spurs are more common in heel pain, spurs are not typically located within the fascia itself but are generally found either deep to its fibrocartilaginous attachment (Kumai & Benjamin 2002) or involving other structures, such as the origin of the flexor digitorum brevis, quadratus plantae, and long plantar ligaments. Given the proposed role of fibrocartilage in redistributing compressive, bending and shear forces, plantar heel spurs have been suggested to develop in response to bending at the fibrocartilage attachment, challenging the widely held assumption that they result from excessive traction within the fascia (Kumai & Benjamin 2002; Wearing et al. 2006). The typical finding of plantar fasciitis on sagittal sonograms involves diffuse or localized hypoechoic areas within a thickened calcaneal attachment (Fig. 5.9.1). A sagittal thickness in excess of 4 mm at the fascial insertion, in addition to hypoechoic change, is a widely used clinical indicator of plantar fasciitis. The sensitivity and specificity of ultrasound in detecting plantar fasciitis ranges from 74–100% and 71–91%, respectively. Such studies, however, have adopted clinical features, rather than histologic evidence, as the diagnostic standard and are difficult to interpret in light of the relatively low specificity of clinical findings in heel pain. While similar observations in tendon have been reported to coincide with histologically verified areas of degeneration, increased fascial thickness has also been reported in both Achilles tendinopathy and seronegative arthritis (Gibbon & Long 1999). Moreover, there is evidence that the thickness of the plantar fascial enthesis, at least in healthy individuals, is dependent on demographic characteristics such as bodyweight. In the absence of bodyweight-adjusted data, therefore, the sensitivity and specificity of ultrasound in the diagnosis of plantar fasciitis remains unknown. Fig. 5.9.1 • Sagittal sonogram of the plantar fascia in individuals with and without plantar fasciitis (A) In pain free individuals, the plantar fascia (PF) is characterized by a moderately echogenic, striated appearance and is approximately 3 mm thick at its calcaneal (C) attachment. From Tsai et al. 2000; Wearing et al. 2007 with permission. (B) Plantar fasciitis is characterized by diffuse or localized hypoechoic areas (*) within a thickened calcaneal attachment. From Gibbon & Long, 1999, with permission. A sagittal thickness in excess of 4 mm has been advocated for the diagnosis of plantar fasciitis. From Tsai et al., 2000, with permission. Note that the normally echogenic borders of the plantar fascia are poorly defined in plantar fasciitis. From Wall et al., 1993, with permission.
Biomechanical function of the plantar fascia
Internal loading of the plantar fascia
Plantar fasciitis
Imaging in plantar fasciitis
Sonographic
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Anatomy of the plantar fascia






