(1)
Department of BioMedical Engineering, Steadman Philippon Research Institute, 181 W. Meadow Dr., Suite 1000, 81657 Vail, CO, USA
Keywords
Posterolateral cornerPosteromedial cornerFibular collateral ligamentPopliteus tendonPopliteofibular ligamentSuperficial medial collateral ligamentDeep medial collateral ligamentPosterior oblique ligamentPosterolateral Corner Anatomy
Introduction
Injury to the posterolateral corner (PLC) of the knee is common; however, it may often be missed during a diagnostic workup due to the lack of understanding of PLC anatomy. The PLC consists of three primary static stabilizers: the fibular collateral ligament (FCL), popliteus tendon (PLT), and popliteofibular ligament (PFL; Fig. 3.1) [1, 2]. In addition, the iliotibial band, biceps femoris, and peroneal nerve are important surgical landmarks (Fig. 3.2). The common peroneal nerve is located approximately 2–3 cm posterior to the long head of the biceps femoris and must be protected during any PLC surgical procedure (Fig. 3.3). Recent advances in PLC anatomy have facilitated the development of anatomic-based repair and reconstruction techniques, which in turn have led to improved outcomes in patients following anatomic PLC repair and reconstruction procedures [3–7].

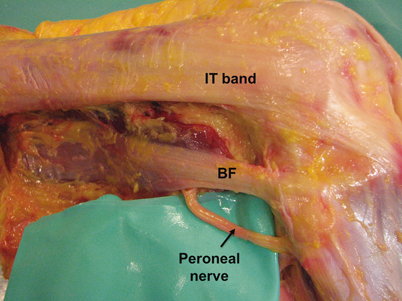
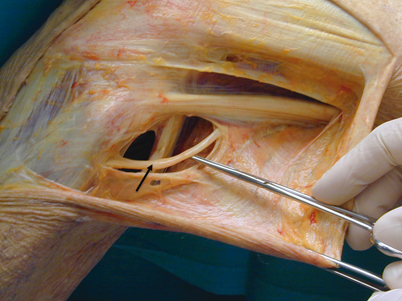

Fig. 3.1
A cadaveric photograph (a) and illustration (b) of the fibular collateral ligament, lateral gastrocnemius tendon, popliteofibular ligament, and popliteus tendon. (From LaPrade et al. 2003 [1]. Reproduced with permission)
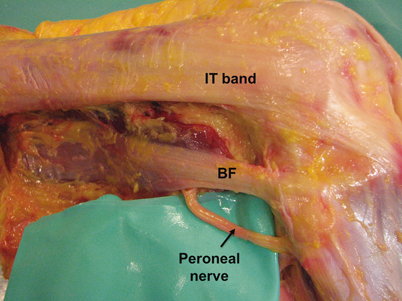
Fig. 3.2
A gross anatomic view of the lateral knee including the iliotibial band, biceps femoris, and peroneal nerve. BF biceps femoris, IT band iliotibial band
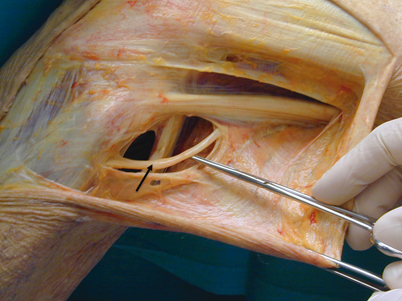
Fig. 3.3
The common peroneal nerve is located approximately 2–3 cm posterior to the long head of the biceps femoris and courses distally along the lateral aspect of the fibular head
Fibular (Lateral) Collateral Ligament
The FCL courses proximal to distal along the lateral aspect of the knee and averages 69.6 mm in length [1]. The FCL proximal attachment is located on the femur in a small bony depression approximately 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle [1]. On anteroposterior radiographs, Pietrini et al. reported that the FCL femoral attachment was located 27.1 mm proximal to the femoral condylar line [8]. LaPrade et al. reported that the average distance between the FCL and PLT femoral attachments was 18.5 mm (Figs. 3.4 and 3.5). At its distal insertion, the FCL inserts 28.4 mm distal to the tip of the fibular styloid in a small bony depression that can be accessed through an incision in the biceps bursa (Fig. 3.6) [1]. On anteroposterior radiographs, the FCL was reported to attach 34.7 mm distal to the tibial plateau [8]. Supplemental FCL fibers have also been described and extend distally along the peroneus longus fascia.
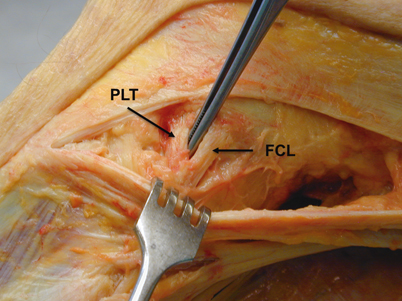
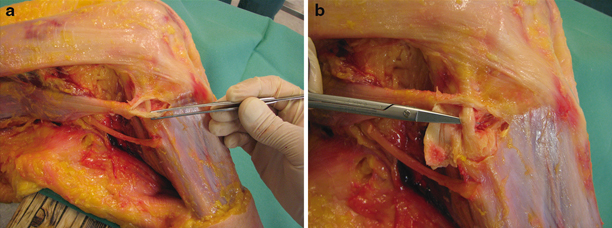
Fig. 3.4
The popliteus tendon and fibular collateral ligament femoral attachments are spaced by an average of 18.5 mm. (From LaPrade et al. 2003 [1]. Reproduced with permission)
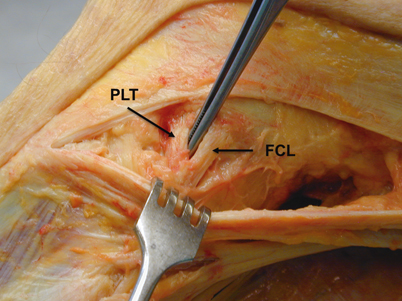
Fig. 3.5
The femoral attachment of the fibular collateral ligament is located through a longitudinal incision in the iliotibial band and is separated from the popliteus tendon attachment by 18.5 mm. FCL fibular collateral ligament, PLT popliteus tendon
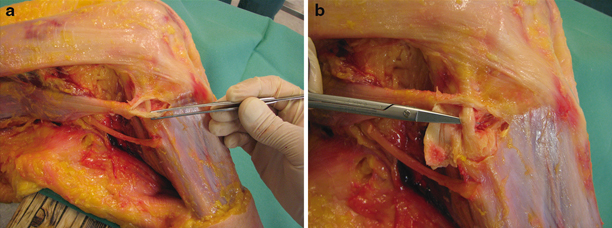
Fig. 3.6
Visualization of the distal FCL attachment is made through the biceps bursa (a) (forceps) and attaches along the lateral aspect of the fibular head (b) (scissors). FCL fibular collateral ligament
Popliteus Tendon
The PLT emerges from the popliteus muscle in the lateral third of the popliteal fossa before becoming intra-articular and coursing proximolaterally around the lateral femoral condyle through the popliteal sulcus [1]. The PLT attaches on the anterior fifth and proximal half of the popliteal sulcus, deep and anterior to the FCL (Fig. 3.7). On radiographic anteroposterior views, the PLT has been reported to attach 14.5 mm proximal to the femoral condylar line [8]. On lateral radiographic views, the PLT attached 14.2 mm anterior to the femoral attachment of the FCL. As the knee cycles through flexion, LaPrade et al. reported that the PLT disengaged from the popliteal sulcus near extension and reengaged with the sulcus at 112° of flexion (Fig. 3.8) [1]. The length of the tendon was also measured to be 54.5 mm from the popliteus musculotendinous junction to the femoral attachment.
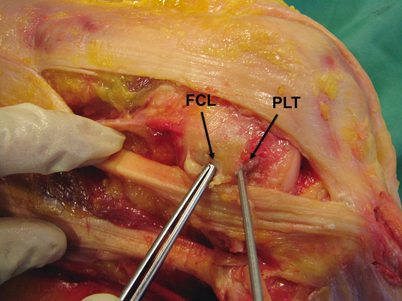
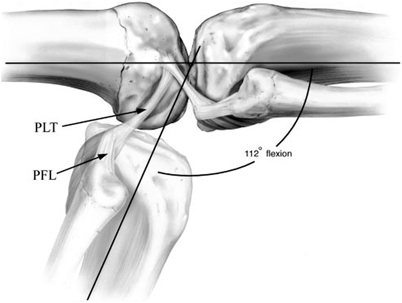
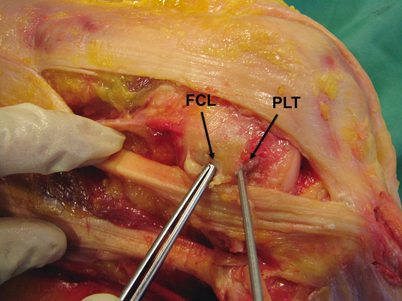
Fig. 3.7
A cadaveric photograph showing the relationship of the fibular collateral ligament and popliteus tendon footprints with both structures removed. FCL fibular collateral ligament, PLT popliteus tendon
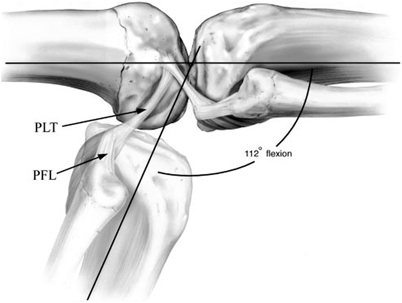
Fig. 3.8
The popliteus tendon engages with the popliteal sulcus at an average of 112° of flexion. (From LaPrade et al. 2003 [1]. Reproduced with permission)
Popliteofibular Ligament
The PFL originates at the musculotendinous junction of the popliteus muscle and consists of an anterior and posterior division [1]. The PFL extends distolaterally before inserting onto the fibular head. The anterior division inserts 2.8 mm distal to the tip of the fibular styloid on the anteromedial downslope. By contrast, the posterior division inserts 1.6 mm distal to the tip of the fibular styloid on the posteromedial downslope. The width of the posterior division is larger than the anterior division at 5.8 and 2.6 mm, respectively. On anteroposterior radiographic views, the PFL was reported to insert 21.0 mm distal to the tibial plateau joint line on the fibular head and 14.1 mm proximal to the fibular insertion of the FCL [8].
Summary
The primary PLC structures include the FCL, PLT, and PFL. Improved quantitative understanding of PLC anatomy has been essential for developing improved diagnostic techniques and anatomic-based repair and reconstruction techniques.
PLC Biomechanics
Introduction
In addition to basic anatomy, the biomechanics of PLC structures have been extensively studied. A comprehensive understanding of PLC biomechanics is necessary to understand the functional consequences of injury, develop improved diagnostics, and validate repair and reconstruction techniques. While the PLC consists of numerous static and dynamic components, this section highlights the biomechanical properties of the primary static stabilizers, including the FCL, PLT, and PFL.
Fibular (Lateral) Collateral Ligament
The FCL functions as the primary static varus stabilizer in the knee at 0 and 30° of knee flexion and a secondary stabilizer to external rotation [2, 9, 10]. When the FCL is injured, static varus stability is compromised, leading to a varus thrust gait pattern, medial compartment osteoarthritis, and medial meniscus tears [11]. LaPrade et al. reported that a clinician-applied varus stress resulted in an increase of 2.7 mm of side-to-side lateral compartment gapping after an isolated FCL tear [12]. In addition, Coobs et al. reported significantly increased varus rotation and internal rotation at 0, 15, 30, 60, and 90° of knee flexion and external rotation at 60 and 90° after sectioning of the FCL in comparison to the intact knee [13].
Popliteus Tendon
While the popliteus complex combines both static and dynamic functional components, the PLT functions in a ligament-like manner. Under a clinician-applied varus stress, sectioning of the PLT and FCL increased the lateral compartment by 0.8 mm in comparison to the isolated FCL sectioning [12]. The sectioning of both structures resulted in 3.5 mm of lateral gapping in comparison to the intact knee. Isolated sectioning of the PLT has also been reported to result in significant increases in external rotation at 30, 60, and 90° of knee flexion ; internal rotation at 0, 20, 30, 60, and 90°; varus angulation at 20, 30, and 60°; and anterior translation at 0, 20, and 30° [7]. No significant differences were noted for posterior translation at any angle. These results lead the authors to propose that the PLT functions as the “fifth ligament” of the knee by providing primary static stability to external rotation and performing a smaller but significant function with respect to internal rotation, varus angulation, and anterior translation. Therefore, repair or reconstruction of the PLT is essential to restore stability to patients with injuries in the PLC of the knee.
Popliteofibular Ligament
The PFL functions as a stabilizer for external rotation, especially from 30 to 60° of knee flexion [2, 14, 15]. In addition, the PFL functions as a secondary stabilizer against varus gapping with the most pronounced effect at 30° of knee flexion [15]. In light of these functional contributions, McCarthy et al. demonstrated that a PFL tibial component is required to reproduce native knee kinematics during a PLC reconstruction. LaPrade et al. reported that sectioning of the PFL, PLT, and FCL, representing a grade III posterolateral injury, resulted in increased lateral gapping of 4.0 mm in comparison to the intact knee [12]. A grade III posterolateral injury resulted in 0.4 mm of increased lateral gapping in comparison to the FCL- and PLT-sectioned state (PFL intact); however, this increase was not deemed to be significant.
Summary
Together, these three posterolateral structures function as essential stabilizers for the PLC of the knee. These structures limit varus laxity, tibial internal rotation, external rotation, and posterior translation. By understanding the biomechanics of posterolateral knee structures, the diagnosis of injuries is improved. In particular, the use of varus stress radiographs has been shown to result in reproducible results that may aid diagnosis of these injuries. Lastly, by understanding native knee biomechanics, repair and reconstruction techniques can be compared to the functional properties of various intact and sectioned states.
PLC Surgical Implications
Introduction
The PLC of the knee consists of both static and dynamic stabilizers that together provide stability to the lateral compartment of the knee. Injuries to the PLC structures are commonly associated with damage to numerous structures. It has been reported that 56 % of PLC injuries include two or more of the major PLC structures, while 70 % of PLC injuries are combined with an anterior cruciate ligament (ACL) tear [16]. Untreated PLC injuries often do not heal due to the convex-on-convex contours of the lateral femoral condyle articulating on the lateral tibial plateau, leading to residual instability and increased risk for medial compartment osteoarthritis (Fig. 3.9) [17]. In addition, biomechanical studies have reported that simulated PLC injuries significantly increase the forces on both ACL and posterior cruciate ligament (PCL ) grafts [18, 19]. These increased forces after PLC injury have, therefore, been validated as contributors to graft failure after cruciate ligament reconstruction. For this reason, proper diagnosis is imperative to optimize outcomes in patients with isolated or combined PLC injuries to prevent secondary complications to other structures in the knee.
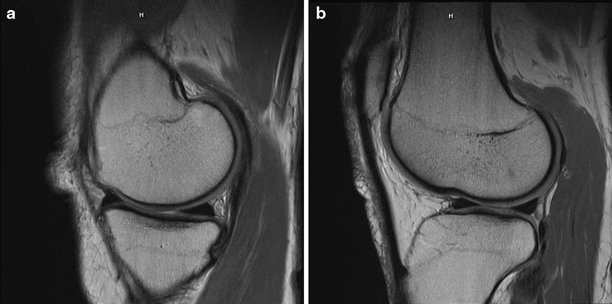
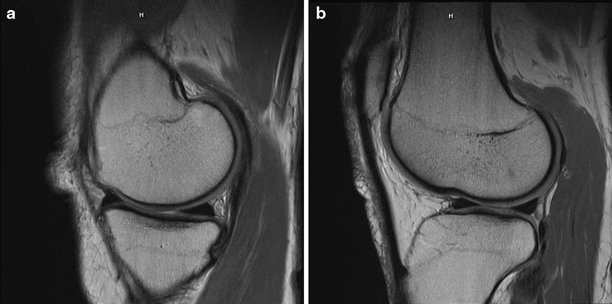
Fig. 3.9
a The medial tibiofemoral compartment has convex-on-concave articulating surfaces, providing increased stability to the medial compartment. b The lateral tibiofemoral compartment has convex-on-convex articulating surfaces creating an inherent degree of instability (b)
Physical Exam
A thorough physical examination of both the injured knee and uninjured knee is essential to diagnose PLC injuries. Inspection and palpation of the PLC should be performed followed by passive and active range-of-motion testing. Special tests include the posterolateral drawer test, dial test, varus stress test, reverse pivot shift test, and standing apprehension test [11]. The external rotation recurvatum test is used to assess for combined PLC and cruciate ligament injuries [20, 21]. Peroneal nerve dysfunction has been reported in 15 % of PLC injuries and must always be considered [22]. Nerve function is evaluated by looking for numbness in the first dorsal web space and weakness to dorsiflexion, foot eversion, and great toe extension. Two widely accepted classification systems for posterolateral knee injury include the Fanelli scale based on the location of injury [23] and the Hughston scale based on the grade of instability [24]. Finally, the results of physical examination can be used to determine injury patterns and develop a treatment plan.
Imaging
Imaging is an important diagnostic tool to augment the assessment of posterolateral knee injury. Plain radiography is used to rule out the presence of avulsions and tibial plateau fractures. In chronic cases, long-leg radiographs should be obtained to assess for the presence of a varus mechanical axis deformity (Fig. 3.10). Varus stress radiographs at 0 and 20° offer an objective and retrievable assessment of lateral compartment gapping. The mean side-to-side difference in lateral compartment gapping in isolated grade III FCL injuries is 2.1 and 2.7 mm at 0 and 20°, respectively (Fig. 3.11) [12]. The side-to-side difference in lateral compartment increases to 3.4 and 4.0 mm in knees with a complete grade III PLC injury. In addition, intra- and interobserver reliability is high, indicating that varus stress radiography is a reliable tool in the diagnostic armamentarium [12, 25].
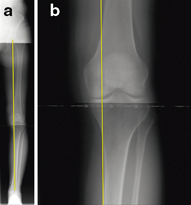
Fig. 3.10
A long-leg radiograph demonstrating a varus weight-bearing axis (a); a close view showing the weight-bearing axis point passing medial to the medial tibial eminence (b)
Fig. 3.11
Varus stress radiographs are an objective and a retrievable method of assessing lateral compartment stability
Magnetic resonance imaging (MRI ) is essential to further assess PLC structural integrity in the FCL, PFL, PLT, cruciate ligaments, and medial and lateral menisci. High sensitivities have been reported for the detection of injury to the FCL and PLT femoral attachment (94.4 and 93.3 %, respectively); however, the sensitivity of the PFL has been reported to be much lower (68.8 %). In addition, while the FCL has been reported to have a specificity of 100 %, the femoral attachments of the PLT and PFL have been reported to have lower specificity values (80 and 66.7 %, respectively) [26]. It is also important to assess for the presence of bone bruise patterns on MRI, which often present as a secondary sign of a PLC injury (Fig. 3.12). In a prospective series of 102 acute PLC injuries, 55 % of patients had a bone bruise on the anterior aspect of the medial femoral condyle [4]. Together, imaging results should be synthesized with findings on physical exam to identify structural and functional deficits and to assist with formulating a treatment plan.
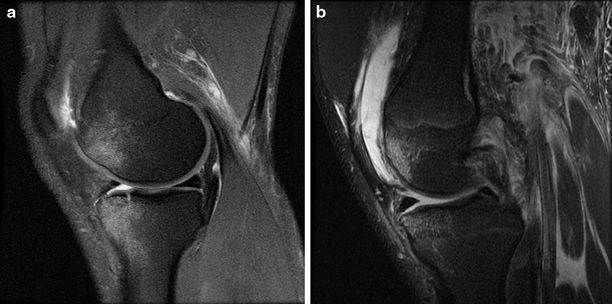
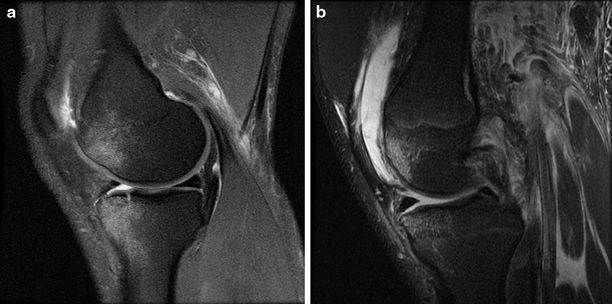
Fig. 3.12
Magnetic resonance images demonstrating bone bruising on the anteromedial femoral condyle (a) and bone bruising on the anteromedial femoral condyle plus a fracture on the anteromedial tibial plateau (b)
Surgical Indications
In acute injuries, primary repair of the PLT or FCL avulsions may be performed within the first 2–3 weeks after injury. Primary repair is contraindicated for midsubstance tears, with reconstruction yielding superior outcomes [27, 28]. Nonoperative management should be considered for the initial management of grade I and II injuries, focusing on edema management, range of motion, and quadriceps muscle exercises [11]. However, many patients with low-grade injury may not always present for treatment.
Patients with combined acute or chronic PLC and cruciate ligament injury should undergo posterolateral reconstruction to avoid recurrent instability and the risk of cruciate ligament graft failure [18, 19]. Therefore, PLC reconstruction functions in two major ways: (1) to eliminate symptomatic lateral knee instability that leads to increased stress on the medial compartment of the knee [4] and (2) to protect concurrent cruciate ligament reconstructions by limiting the strain on reconstruction grafts [18, 19].
While primary reconstruction is indicated in patients with acute grade III injuries [11, 29], limb alignment must be assessed first in patients with chronic posterolateral knee injuries. In chronically injured knees, limb alignment must be assessed during surgical planning. Failure to correct underlying varus alignment places the soft tissue posterolateral reconstruction grafts at a high risk of failure. When varus alignment is detected, a proximal tibial opening wedge osteotomy can be used, which resolved posterolateral instability without reconstruction in 38 % of patients in one case series [30].
Surgical Techniques
Grade III injuries to the FCL, PFL, and PLT almost always require repair or reconstruction. Numerous techniques have been described that can be divided into nonanatomic procedures, including the “arcuate complex” advancement [31], biceps femoris tenodesis [32], anterior or posterior tibialis allograft reconstruction [28], single femoral tunnel reconstruction [33], and anatomic procedures utilizing two femoral tunnels with or without popliteus bypass and PFL reconstruction [3, 34–36]. The authors prefer an anatomic reconstruction utilizing a split Achilles tendon allograft to reconstruct the FCL, PFL, and PLT, which has been validated to improve clinical outcomes after surgery [3, 5, 15].
Posteromedial Corner Anatomy
Introduction
The posteromedial corner (PMC) of the knee is a very commonly injured area of the knee. The most clinically relevant structures of the PMC are the superficial medial collateral ligament (sMCL), the deep medial collateral ligament (dMCL), and the posterior oblique ligament (POL) [37]. In addition, the saphenous nerve courses through the medial aspect of the knee and must be avoided during medial knee surgery (Fig. 3.13). The understanding of the anatomy of each of these ligamentous structures as well as relevant bony landmarks of the medial knee has continued to evolve, which has resulted in a more refined approach to repairing and reconstructing these ligaments.
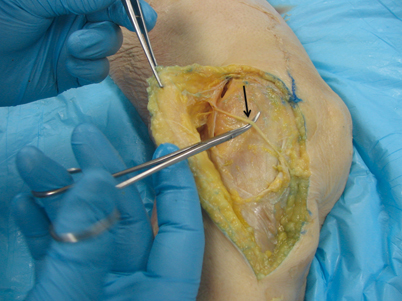
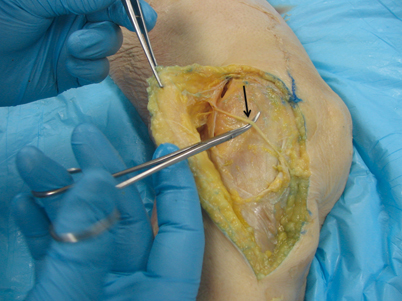
Fig. 3.13
The saphenous nerve courses across the medial aspect of the knee and may be at risk of iatrogenic injury during medial knee surgery (arrow)
Medial Femoral Bony Landmarks
The qualitative and quantitative anatomy of the prominent femoral bony landmarks of the medial epicondyle, adductor tubercle, and gastrocnemius tubercle has helped to allay the confusion in the literature regarding the attachment sites of the PMC ligaments [38–41]. LaPrade et al. examined the relationship of all three bony landmarks and reported the qualitative and quantitative relationships among these structures [40]. The medial epicondyle is the most anterior and distal of the three medial bony landmarks (Fig. 3.14). The adductor tubercle is at the distal edge of the medial supracondylar line on the distal aspect of the femur, located 12.6 mm proximal and 8.3 mm posterior to the medial epicondyle. The newly described gastrocnemius tubercle can be referenced off either the medial epicondyle or the adductor tubercle. This structure is 9.4 mm distal and 8.7 mm posterior to the adductor tubercle and adjacent to a depression where the medial gastrocnemius tendon attaches. In addition, it can be located 6.0 mm proximal and 13.7 mm posterior to the medial epicondyle.
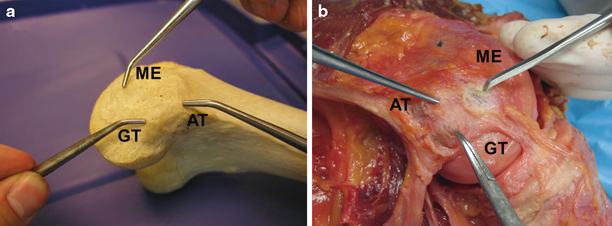
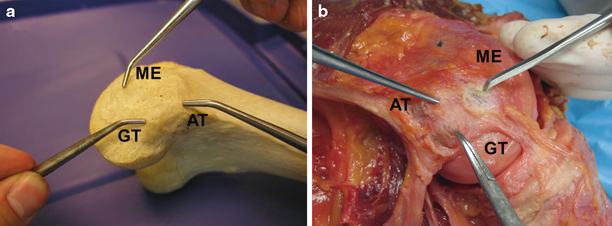
Fig. 3.14
Bony medial knee landmarks (a–b) can be readily identified during a medial knee dissection. AT adductor tubercle, GT gastrocnemius tubercle, ME medial epicondyle
Superficial Medial Collateral Ligament
The anatomy of the sMCL was first reported by Brantigan and Voshell, which they termed the tibial collateral ligament [42]. The authors reported that the sMCL attached to the femur at the medial epicondyle and split into two separate attachments on the tibia. Later reports clarified that the sMCL has one femoral attachment and two tibial attachments (Fig. 3.15) [40]. The femoral attachment is located in a depression 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle and 26.8 mm proximal to the femoral joint line (Fig. 3.16). The authors reported that there was no functional attachment between the sMCL and dMCL or any bursae between the two structures. In addition, Wijdicks et al. reported the sMCL attachments in relation to radiographic reference points [43]. The femoral attachment of the sMCL was reported to be 30.5 mm distal to the femoral condylar line on anteroposterior views and 6.0 mm from the medial epicondyle on lateral views.