Anatomic Double Bundle Anterior Cruciate Ligament Reconstruction
Steven B. Cohen MD
James Starman MD
Freddie H. Fu MD
The anterior cruciate ligament (ACL) is composed of two major bundles. The posterolateral (PL) bundle is posterior and lateral on the tibial footprint and the anteromedial (AM) bundle is anterior and medial on the tibial footprint.
The posterolateral bundle originates more distally and anteriorly relative to the AM bundle on the wall of the intercondylar notch.
When the knee is extended, the PL bundle is under tension and the AM
bundle is moderately lax. With knee flexion, the AM bundle tightens and the PL bundle becomes lax.
Patients who are having recurrent instability or giving way episodes or who are unable to return to activities of daily living or sport are appropriate for anatomic double bundle ACL reconstruction.
ACL injury typically is the result of an acute pivoting episode, which is most commonly noncontact.
Before ACL reconstruction, it is important to determine and address any associated injuries involving the meniscus and chondral surfaces.
Radiographs include weight-bearing anteroposterior (AP) 30-degree flexion, lateral, and sunrise views. Magnetic resonance imaging is essential for assessing both bundles of the ACL, other ligamentous structures, menisci, chondral surfaces, and bone bruises.
Patients wear a hinged knee brace postoperatively for 6 weeks. Continuous passive motion is started immediately after surgery. Noncutting and nontwisting sports are allowed after 12 weeks.
No long-term study results are yet available on anatomic double bundle ACL reconstruction. Further studies are needed to show the apparent potential for reconstruction with separate AM and PL bundles to better recreate normal anatomy and biomechanics of the knee than with single bundle ACL reconstruction.
Complete anterior cruciate ligament (ACL) ruptures can lead to recurrent knee instability, meniscal tears, and articular cartilage degeneration. Traditionally, reconstruction of the ACL has been performed using a single-bundle reconstruction technique that attempts to recreate the anteromedial bundle (AM) of the normal ACL. Review of the literature suggests that the success rates of single-bundle ACL reconstruction vary between 69% and 95%. A potential explanation for unsatisfactory results of the conventional single-bundle reconstructions may be that simply reconstructing the AM bundle does not restore the complex function of the intact ACL.
To fully understand the principles of ACL reconstruction, it is important to understand the complex anatomy of the ACL, which is composed of two major bundles. These specific bundles are named relative to their relationship on the tibial footprint; the PL bundle is posterior and lateral on the tibial footprint and the AM bundle is anterior and medial on the tibial footprint. However, the PL bundle originates more distally and anteriorly relative to the AM bundle on the wall of the intercondylar notch. When the knee is extended, the PL bundle is under tension and the AM bundle is moderately lax. With knee flexion, the AM bundle tightens and the PL bundle becomes lax. Additionally, with internal and external rotation of the tibia at 90 degrees of flexion, the PL bundle tightens.
Biomechanical studies have shown that ACL single-bundle reconstruction using either patellar tendon or quadrupled hamstring autograft is successful in limiting anterior tibial translation but is insufficient in controlling a combined rotatory load of internal and valgus torque (1). In addition, Loh et al. (2) showed that the 2 or 10 o’clock femoral tunnel position of a single-bundle ACL reconstruction improved rotatory stability when compared with the 1 or 11 o’clock position. However, neither the 10 o’clock nor the 11 o’clock tunnel position could restore the kinematics and the in situ forces of the intact knee.
Traditional techniques in ACL surgery that simply reconstruct the AM bundle do not fully address the anatomic insertion sites and the biomechanical complexity of the intact ACL. Therefore, we have begun to perform the arthroscopic technique for anatomic double-bundle ACL reconstruction that reconstructs both the AM and the PL bundle through separate anatomically based tunnels with either autogenous semitendinosus and gracilis or tibialis anterior allograft.
The indications for anatomic double bundle ACL reconstruction are similar to those for traditional single bundle reconstruction. Patients who are having recurrent instability or giving way episodes or who are unable to return to activities of daily living or sport are appropriate for surgical reconstruction. In addition, patients with complaints of instability and a single bundle or “partial” tear may benefit from single bundle augmentation or double bundle reconstruction in the event the remaining bundle is incompetent. The double bundle reconstruction has been especially useful in the revision setting, particularly when the previous femoral tunnel placement has been in the traditional “over the top” position which is too high in the femoral notch. This allows anatomic placement of the two femoral tunnels without interfering with the previous tunnel.
We have not found a contraindication to the procedure in the skeletally mature patient. The height of the patient or size of the knee has not been a factor when performing the surgery.
A thorough history and physical examination are required prior to surgical reconstruction. Typically there is a history of an acute pivoting episode associated with an injury, most commonly noncontact. In a chronic setting, the patient complaints are generally related to knee instability or repeated giving way. Specific examination abnormalities consist of Lachman, anterior drawer, and pivot shift. It is important to determine any associated injuries involving the meniscus and chondral surfaces. A KT-1000 exam is used to determine side-to-side antero-posterior (AP) translational difference. Radiographs include weight-bearing AP 30-degree flexion, lateral, and sunrise views. Magnetic resonance imaging is essential for assessing both bundles of the ACL, other ligamentous structures, menisci, chondral surfaces, and bone bruises. Patient education is also critical prior to ACL reconstruction.
The patient is identified in the preoperative holding area and the surgeon marks the correct limb. The procedure can be performed with general or spinal anesthesia according to the preference of the patient and the anesthesiologist. In the operating room, the patient is positioned supine on the operating table and the nonoperative leg is placed in a well-leg holder in the abducted lithotomy position. A pneumatic tourniquet is applied around the upper thigh of the operative leg, the operative limb is exsanguinated by elevation for 3 minutes, and the tourniquet is insufflated to 300 to 350 mm Hg depending on the patient size. The limb is positioned in an arthroscopic leg holder and the operative leg is prepared and draped (Fig 34.3-1). The portals used for this procedure are slightly different from standard arthroscopy portals. The anterolateral portal is placed more superior at the level of the inferior pole of the patella just lateral to the patella tendon. The anteromedial portal is placed just below the inferior pole of the patella approximately 1 cm lateral to the medial edge of the patella tendon (intratendinous portal). Finally an accessory inferior medial portal is established using direct visualization with an 18-gauge spinal needle, which is inserted medially and distally to the inferomedial portal just above the meniscus (Fig 34.3-2). This is done for better access of the lateral wall of the intercondylar notch when placing the femoral PL tunnel and femoral AM tunnel if transtibial tunnel location placement is unacceptable. Importantly, the arthroscope is placed in the anteromedial portal during femoral tunnel placement for better
visualization of the intercondylar notch, while the camera is maintained in the anterolateral portal for tibial tunnel placement.
visualization of the intercondylar notch, while the camera is maintained in the anterolateral portal for tibial tunnel placement.
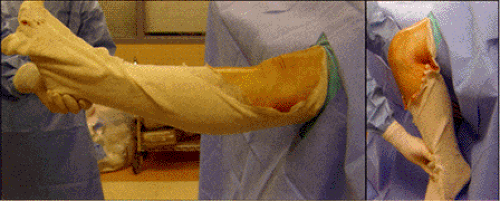 Fig 34.3-1. Leg positioning. It is essential to allow for a full range of motion between extension and 120 degrees flexion. |
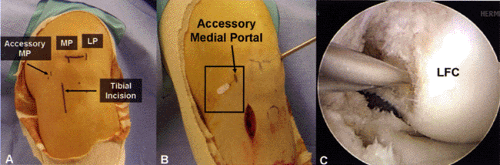 Fig 34.3-2.A: Arthroscopic portal placement. MP, medial portal; LP, lateral portal; AM, accessory medial portal. B, C: Accessory medial portal visualization with 18-gauge needle. |
Any associated meniscal or chondral lesions are addressed prior to the ACL reconstruction. The torn ACL is carefully dissected using a thermal device to determine the injury pattern (Fig 34.3-3) and with special attention to the anatomic footprints of the two ACL bundles on the lateral wall of the intercondylar notch and on the tibial insertion (Fig 34.3-4). The tibial footprints are left intact because of their proprioceptive and vascular contributions. The PL femoral tunnel is the first tunnel to be drilled, using the accessory anteromedial portal. A 3/32 Steinman pin is inserted through the portal and the tip of the guidewire is placed on the femoral footprint of the PL bundle on the lateral wall of the intercondylar notch (Fig 34.3-5). It is important to note that the femoral footprint of the ACL changes with the position of knee flexion. When the knee is positioned at 90 degrees of flexion, the PL and AM bundles’ orientation on the femur is horizontal and in full extension, the orientation is vertical (AM bundle superior to PL bundle). Once the tip of the guidewire is placed in the correct anatomic position, the knee is flexed to 120 degrees and the guidewire is manually tapped into the femur. Hyperflexion while placing the PL femoral tunnel is performed to avoid injury to the peroneal nerve when passing a beath pin. The femoral PL tunnel is drilled with a 7 mm acorn drill that is inserted over the guidewire taking care to avoid injury to the medial femoral
condyle articular cartilage. The PL tunnel is drilled to a depth of 25 mm to 30 mm (Fig 34.3-6). Then the far cortex is breached with a 4.5-mm EndoButton drill (Smith & Nephew, Andover, MA), and the depth gauge is used to measure the distance to the far cortex.
condyle articular cartilage. The PL tunnel is drilled to a depth of 25 mm to 30 mm (Fig 34.3-6). Then the far cortex is breached with a 4.5-mm EndoButton drill (Smith & Nephew, Andover, MA), and the depth gauge is used to measure the distance to the far cortex.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



