Allograft Prosthesis Composite Replacement for Bone Tumors of the Proximal Femur
George C. Babis
Vasileios I. Sakellariou
Franklin H. Sim
Limb salvage has become the standard method of treatment of aggressive benign tumors and most bone malignancies (1) such as osteosarcoma, Ewing sarcomas, malignant fibrous histiocytomas, giant cell tumors, and metastatic bone lesions. Limb salvage requires en bloc resection of the involved bone with adequate margins, followed by reconstruction (1).
Allograft prosthesis composites have been used since the late 1980s in orthopaedic oncology (2,3,4,5). The main advantage, comparing to resection megaprosthesis, is the effective reattachment of the tendons of the hip abductors and iliopsoas muscles, thereby preventing dislocation and allowing better function (6). Additionally, incorporation and fusion of the allograft to the host bone decreases the possibility of resorption of the host bone around the proximal part of the prosthetic stem due to stress shielding (6). The allograft provides a dry virgin lattice for good cementing, but it does not need to be fixed to the distal part of the host femur with cement; hence, it does not compromise following revisions (7). Comparing to structural osteoarticular allografts, the main advantage is that joint deterioration and collapse that can be encountered with allograft cartilage is avoided (8). Subsequently, the biological capabilities of the allograft are combined with predictability and modularity of an implant.
The main disadvantages of segmental placement with allograft prosthesis composite are the technical difficulties and their cost. The long period of time that is necessary for healing at the graft-host junction and the potential for the transmission for disease are also major disadvantages. In addition to transmission of HIV, which has attracted the greatest attention, the possible transmission of hepatitis and other viral agents should be considered (9,10).
Besides, the biological characteristics of the allograft bone may lead to nonunion, resorption, or even fracture of the graft. Loosening of an allograft-prosthesis composite is not less problematic than loosening of a proximal femoral replacement. Allograft antigenicity and immune rejection, even yet unclear (11), may be related to incidents of resorption (9,12,13).
INDICATIONS
The precise indications for use of allograft composite vary from center to center, but essentially it is preferred in the following:
For younger patients with a longer life expectancy
When substantial portions of the periacetabular muscles and tendons can be spared
When it is not planned to use radiation therapy, which can interfere with bone healing
Also used in cases of short resections (<12 cm, mainly in treating benign tumors) because some modular resection prostheses have a minimal length of 12 cm (6).
SURGICAL TECHNIQUE
Preoperative Planning
A thorough oncological assessment is necessary before proceeding to this reconstructive procedure. Classification and staging of the tumor should be known. Life expectancy is a parameter that may alter the decision for the kind of reconstructive procedure. As previously referred, patients with short life expectancy should be better treated with proximal femoral replacement rather than an allograft reconstruction for which a long period of non-weight bearing is demanded. Technically, plain x-rays of the pelvis and the femur are essential to determine the level of resection, possible limb length discrepancy, as well as the size of the allograft to be used. Magnetic resonance images could also be helpful for the specification of the anatomical margins of the tumor.
The hip joint should be carefully examined preoperatively assessing the abductors sufficiency and the limb length. The patient should be informed for the potential of postoperative limb length discrepancy. If an elongation of more than 4 cm is expected, electrophysiology monitoring of the femoral and sciatic nerves could be beneficial.
A longer allograft than that templated should be available. The diameter of the allograft should preferably be matching with that of the host femur. As the allograft is usually underreamed and cemented to the stem, the medullary canal of the allograft should be equal to or slightly larger than the femoral canal of the host femur. The stem is templated according to the diameter of the host femoral canal. Cementless press fit fixation is preferred preserving host bone stock for future revisions. The femoral stem should be planned to bypass the allograft and the femoral isthmus. If that is not possible, additional screws and plates should be placed to stabilize allograft-host junction. Generally, we try to insert as less screws as possible as screw holes weaken the allograft and act as stress raisers, leading to allograft fractures. Intraoperative alterations of the initial templating are not rare, and allograft-host fixation alternatives should be scheduled and be available during surgery. Long strut grafts and cables or circlage wires should be available to be placed at the allograft-host junction. Dall-Milles cables or wires should be available for the trochanteric reattachment to the allograft. Templating of megaprosthesis should also be done, as intraoperative fracture of the only size matching allograft is possible.
ANESTHESIA AND PATIENT POSITIONING
Regional epidural anesthesia is generally preferred for the potential of postoperative pain control. The group of anesthesiologists should be aware of the duration of this procedure, which has a mean time of 4 hours and may exceed 6 hours, as well as the amount of blood loss, which has a mean value of 2,000 mL and sometimes may exceed 5,000 mL (14). Unfortunately, blood conservation techniques, such as intraoperative cell saving and postoperative autologous blood transfusion, should be avoided due to the risk of spreading the initial malignant disease.
The patient is positioned in a true lateral position with the affected hip uppermost. It is important that bony prominences of the legs and pelvis are protected with pads under the lateral malleolus and knee of the bottom leg and a pillow between the knees. The limb should be draped leaving free room for movement during the operation. The drapes should leave uncovered the lateral aspect of the femur and the knee as the incision may be extended distally.
ALLOGRAFT CHARACTERISTICS AND PREPARATION
Frozen structural allografts primarily possess the osteoconductive, and not the osteoinductive, property of bone grafts (7). They are biologically inert and therefore function as implants. Fresh allograft bone evokes an immune response in the host that may result in resorption of the graft or in a marked delay in the incorporation of the graft.
Deep-freezing and freeze-drying at -70°C have a shelf life of 5 years (15) and decrease the immunogenicity of allograft bone. These methods allow for long-term preservation and storage of allograft bone. Freeze-dried bone is weaker in bending and torsion than fresh-frozen bone (16,17,18), but it has the advantage of being less antigenic (19). The American Association of Tissue Banks have set standards in order to reduce the risk of diseases transmission (20,21). The risk of transmission of the human immunodeficiency virus is thought to be less than one in one million (20,21). Irradiation of the graft further reduces this risk (22), but radiation may weaken the allograft bone (23).
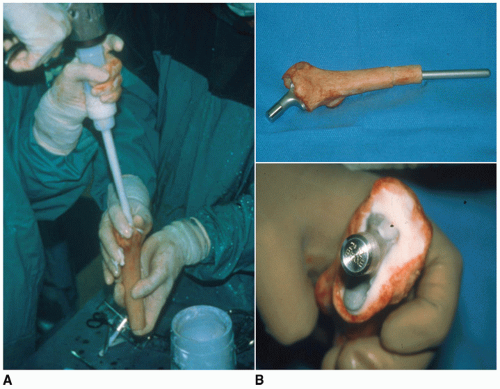
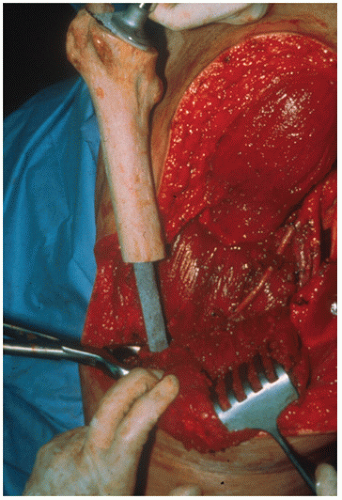 FIGURE 12.1 Intraoperative image, showing the trial reduction of the implant in the host femur and into the acetabulum, in order to assess the appropriate length of the graft. |
At the time of reconstruction, the allograft is unwrapped, specimens are obtained from it for culture, and it is then placed in a warm antibiotic-containing solution. To reduce operative time, the graft is prepared on a separate table by part of the surgical team. The length of the bone resection is templated and measured before operation. An allograft that is longer than needed is ordered to allow for any intraoperative variations. The approximate length of the graft required is assessed by a trial reduction (Fig. 12.1) of the implant in the host femur and into the acetabulum. Hip stability and any preoperative limb-length discrepancy are taken into account in determining the length of the allograft.
The allograft is cleaned of soft tissue and then is reamed and broached (Fig. 12.2) until a good fit for the implant is achieved while allowing for a cement mantle of at least 2 mm around the stem. The graft does not have to be excessively reamed while still having a cement mantle of at least 2 mm.
A long-stem modular femoral prosthesis offering distal fixation is used. The femoral stem must be long enough to reach the distal femoral diaphyseal-metaphyseal junction, or else to achieve at least 6 cm of
prosthesis-shaft contact bypassing the allograft-host junction (6). Trial reduction of the prosthesis-allograft composite is done, and a transverse, oblique or step-cut osteotomy of approximately 2 by 3 cm is marked and made, according to the surgeon’s preferences and allograft-host femoral canal matching. Adjustments are usually needed for correct anteversion and length. On the back table, the graft canal is cleaned and dried, and cement is pressurized into the graft. The stem is then inserted in the correct anteversion (see Fig. 12.2). Great care is taken to ensure that the cement is recessed around the allograft-host junction to allow host-bone contact. The composite is then inserted into the host stem, and the hip is reduced. Finally, wires or cables are passed around the lesser trochanter of the allograft for later attachment to the greater trochanter of the host.
prosthesis-shaft contact bypassing the allograft-host junction (6). Trial reduction of the prosthesis-allograft composite is done, and a transverse, oblique or step-cut osteotomy of approximately 2 by 3 cm is marked and made, according to the surgeon’s preferences and allograft-host femoral canal matching. Adjustments are usually needed for correct anteversion and length. On the back table, the graft canal is cleaned and dried, and cement is pressurized into the graft. The stem is then inserted in the correct anteversion (see Fig. 12.2). Great care is taken to ensure that the cement is recessed around the allograft-host junction to allow host-bone contact. The composite is then inserted into the host stem, and the hip is reduced. Finally, wires or cables are passed around the lesser trochanter of the allograft for later attachment to the greater trochanter of the host.
SURGICAL TECHNIQUE OF RECONSTRUCTION
We mostly use the lateral approach (Hardinge) or the posterolateral approach (Moore). Oncological principles should be followed first. Open incision biopsy tracts should be excised. En bloc resection of the tumor should be done without compromising other compartments. Rising of large muscle flaps should be avoided. Reconstruction procedure should not interfere with meticulous en bloc tumor resection. In all cases, samples for biopsies and cultures should be obtained and quick biopsy and Gram stain results should be known before proceeding to reconstruction.
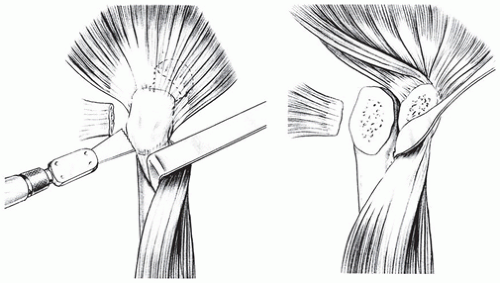
Substantial portions of the periacetabular muscles and tendons should be spared, if possible, so to be later reattached to the allograft. A sliding osteotomy of the greater trochanter is usually done because it is more stable than a transverse osteotomy and is associated with a lower risk of trochanteric migration (Fig. 12.3). The trochanteric osteotomy offers a better exposure of the hip joint, as well as a bony fragment for reattachment of the abductors to the graft. After the trochanteric osteotomy is done, the abductors and the vastus lateralis muscles are slightly displaced anteriorly, so that the anterolateral aspect of the femur is exposed to perform the femoral osteotomy. Care is taken not to strip any residual bone of its soft tissue completely, as it later is used as a vascularized autogenous graft if it is not included into the tumor mass. Before performing the resection osteotomy of the proximal femur, a Steinmann pin is inserted into the iliac crest and the distance to a reference point on the distal femur is used to determine the leg length and rotation of the host femur, as well as the length of the allograft. Then, the femur is osteotomized and excised.
There are several techniques to do a femoral osteotomy (Fig. 12.4). A transverse osteotomy (Fig. 12.4A) is the easiest to do but it does not provide adequate rotational stability. Fixation with one (anterolateral) or
usually two plates (one lateral and one anterior) is often needed for a stable construct. This results in developing many screw holes, which act as stress risers that weaken the allograft and potentially lead to allograft fracture. Telescoping the graft inside the host femoral canal or reversely the host femur into the allograft-prosthesis composite (intussuception technique)



usually two plates (one lateral and one anterior) is often needed for a stable construct. This results in developing many screw holes, which act as stress risers that weaken the allograft and potentially lead to allograft fracture. Telescoping the graft inside the host femoral canal or reversely the host femur into the allograft-prosthesis composite (intussuception technique)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree