Fig. 6.1
Patient is pointing to a point at or just caudal to the posterior superior iliac spine, the most usual site for sacroiliac joint pain (Fortin Finger Test). If a patient points to this spot, the clinician must rule out the sacroiliac joint as a potential pain generator. Copyright Borgess Health
A literature review would suggest that if the pain is below the level of the L5 vertebral body, and there are no dural tension signs (i.e., positive SLR), then the pain generator might be the SIJ [4, 20].
At this point, with strong suspicion that the pain might be coming from the SIJ, some clinicians would want to verify the diagnosis by injection before continuing with treatment knowing that the injection itself would potentially start the treatment process. The down side of doing an injection at this point is that if the SIJ is a normal joint and not the pain generator, an injection could possibly cause changes that might render the joint other than normal. More study is needed to validate this concern. Most practitioners would do some conservative treatment measures first that might work and avoid any invasion into the joint if successful. The algorithm allows for both options depending on the judgment and the training of the provider.
Treatment
Now, it is time to begin treatment. It is here that many clinicians become confused and lost about where to start, how long to do something, and what to do next. Again, the treatment process should start simple, using less-invasive measures, and cost the least. If these do not work, then it is time to move up to more complex and invasive treatments.
Types of conservative treatment:
Basic measures for low back pain prior to imaging studies
Imaging studies followed by, if appropriate, manipulation
Formal physical therapy
Injections
Conservative Treatment Prior to Imaging or Injections
Treatment begins with anti-inflammatory medications, the possible use of a brace (sacral belt), and an alteration of activities. Anti-inflammatory medications can, in some patients, produce miraculous results from the start suggesting that there is a significant inflammatory component to the SIJ pain. When anti-inflammatory medication does not work or the effects are not enough, then the addition of a sacral belt might make a significant difference in the pain. The sacral belt is worn to control symptoms as much or as little as the patient determines is necessary. There is no known negative effect on the muscles by wearing a sacral belt on a continuous basis, as the back muscles are not being unloaded by this brace. One complication from wearing a sacral belt is trochanteric bursitis due to direct pressure on this region, which, if occurs, may necessitate discontinuing the sacral belt. The main activities that patients tend to avoid to reduce symptomatology are sitting, standing long periods on the ipsilateral leg, laying on the affected side, and, in women, sexual intercourse with abducted legs. Avoiding these activities as a way to control symptoms can be challenging as many are required for activities of daily living or needed for human relationships.
Imaging Studies
If the conservative measures thus far have not significantly decreased pain, it is at this point that we would recommend obtaining imaging studies of the SIJ and surrounding areas. Keep in mind that all the necessary imaging for suspected lumbar-related pain has already been done prior to starting this algorithm. If the usual “red flags” for a trauma, infection, or tumor had surfaced before this time (e.g., rapid weight loss, night pain, recent severe trauma, etc.), X-rays would have been done at the first consultation. It is important now to rule out hip joint pathology, sacral stress fracture, tumor, infection, or other causes that might need to be treated in specific ways other than with this algorithm. This is when a diagnosis of sacroiliitis might be made and a referral to a rheumatologist recommended. The X-rays we would recommend would be an AP of the pelvis to include both hips and specific oblique X-rays of the SIJs. A CT scan or an MRI would remain optional at this time only to further clarify an abnormality or suspicion found on the plain films. It should be remembered that there is no correlation in the literature between how a SIJ looks on imaging and how it feels in the patient in the absence of a fracture, tumor, or infection [4, 5, 21, 22].
Manipulation
Manipulation is the next treatment that should be considered if the more conservative measures have not helped and nothing alarming is found on X-ray. The neuromuscular and physiological effects of thrusting maneuvers have been found, in our experience at BBSI, to be the most beneficial in the treatment of SIJ pain at this stage in the algorithm. Chiropractors, osteopaths, or physical therapists trained in these treatment modalities should be the ones providing these treatments. Manipulation can be one of the most successful conservative treatment measures for the painful dysfunctional SIJ and should be done prior to moving into more complex, expensive, and invasive treatments. If manipulation efforts, lasting no longer than 6–12 weeks, result in no lasting improvement, a formal physical therapy evaluation and treatment program is recommended [2].
Physical Therapy
Physical therapists will evaluate and treat the entire thoracolumbar, pelvic, and lower extremity anatomy. Interventions will be utilized to stretch, strengthen, and stabilize all of the musculoskeletal structures that have an effect on the SIJs. This will be done in an effort to promote structural and force symmetry through and around the SIJs. Also, the therapist can utilize modalities such as ice, heat, ultrasound, etc. to optimize outcomes. This chapter will not discuss the seemingly endless ways that these methods can be accomplished by the physical therapist. Chapter 14 covers the post-fusion rehabilitation by physical therapy.
Injections
Injections can be done at different points within this algorithm based on the experience of each individual patient and surgeon. It is placed here in the algorithm due to the fact that in a new patient being diagnosed and treated for the first time for a dysfunctional SIJ, an injection is not really needed in the treatment regimen until now. It is realized by the authors that this is a controversial statement, and in reality, our usual patient is referred to us having already had one or more diagnostic and/or therapeutic SIJ injections. It then becomes our job to be sure that all the necessary algorithm steps up to this one have been satisfied before moving on through the algorithm. If 6–12 weeks of physical therapy is not improving the patient, then more invasive and more costly measures are introduced. These start with injections if they have not already been performed. If a SIJ injection has not been done up to this point, then this injection is both diagnostic and potentially therapeutic [5, 20]. Injections should be performed using fluoroscopy with contrast dye to verify that a long-acting anesthetic agent and a steroid preparation have indeed entered the SIJ. The patient’s spine surgeon, physiatrist, anesthesiologist, interventional radiologist, or pain physician routinely performs the injections (Fig. 6.2).
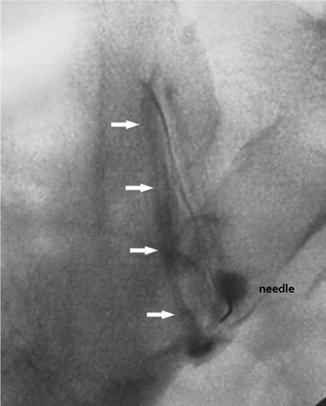
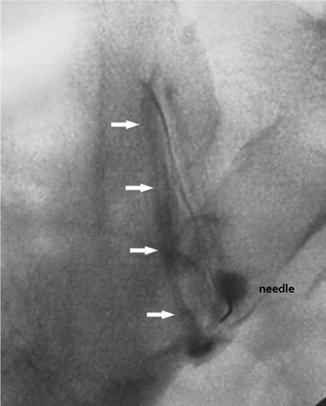
Fig. 6.2
Oblique image showing the needle at the most caudal portion of the joint with dye outlining the entire joint
A Two-Way Street
The process of performing SIJ injections requires communication between both the physician performing the injection and the patient receiving the injection. It is mandatory that the physician thoroughly understands exactly where the patient’s pain is primarily felt and where it radiates. Since the injection is the clinician’s way of making an accurate diagnosis of a dysfunctional SIJ, and it is frequently also the primary way of making a diagnosis of facet syndrome, symptomatic foraminal stenosis that might respond to decompression, and primary discogenic pain, it is paramount that the clinician has from the beginning a clear idea of where the patient’s pain might be coming from. It is only through constant dialogue with the patient before, during, and after the injection(s) that the best accurate information about the patient’s pain can be obtained. The process of “honing in” on the diagnosis through repeated injections and injections into other areas can therefore be very complex and requires a dedicated physician to ultimately make the correct diagnosis or multiple diagnoses as the case may be.
Injections and Radiating Leg Pain
One of the confusing symptoms in patients with a dysfunctional SIJ is the presence of radiating leg pain. With the advent of injecting the SIJ with dye, to confirm that the medication being injected is indeed going into the joint, the dye has been visualized “leaking” out of the joint, through tears in the joint capsule. This leaking is verification that whatever else is in the joint (e.g., synovial fluid, lysozymes, etc.) can leak out and come in contact with surrounding tissues. Many of these tissues are nerve roots or a plexus of nerves. If whatever contacting the nerve tissue is irritating the nerve, the result might be the generating of an impulse in the nerve, thus creating referred pain down the leg. It is our experience that an EMG in such a patient is usually normal as there has been no nerve compression or permanent nerve tissue injury (Fig. 6.3).
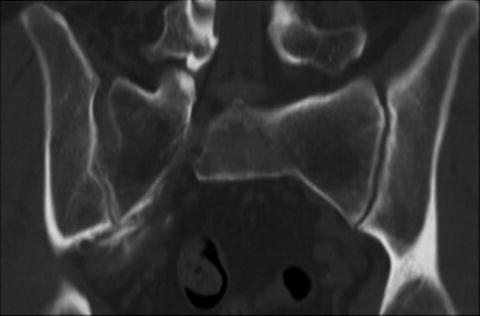
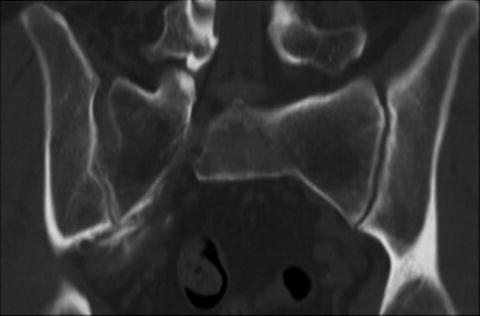
Fig. 6.3
Dye leaking out of the caudal portion of the SIJ joint capsule coming in potential contact with nerve tissue, which can result in radiating pain
The Injection Specialist
The injection specialist may or may not be the surgeon who will ultimately make the decision to operate on a SIJ. Many of us participating in the writing of this textbook did at one time do our own injections, and one or two still do. The propagation of injection specialist within the “pain management” segment of medicine now enables surgeons to send their patients to such specialists for these injections. Suffice it to say that the injection specialist has a formidable job to make an accurate diagnosis by using their injection abilities, as has been stated earlier, but it is beyond the scope of this textbook to provide teaching on the specifics of how to become an expert in the injection field.
Intra- Versus Extra-articular Injections
It should be understood that there are both intra-articular SIJ pain generators and extra-articular ones as well. The literature suggests that both intra-articular and extra-articular injections can be of benefit for both diagnosis and potential treatment in patients with painful, dysfunctional SIJs [16, 23–28]. Fluoroscopy should be used for the extra-articular injections as well. Our current institutional standard at BBSI is to perform an intra-articular injection and to consider an extra-articular injection only if the intra-articular injection was negative and the clinician has a very high suspicion that the pain is SIJ related and no lumbosacral pathology has been found.
Diagnostic Part of the Injection
Occasionally, the pain generators can be coming from both the SIJ and the lumbar spine (e.g., facet joints, foraminal stenosis), and injections become the only way to diagnose them accurately and potentially treat them. The diagnostic portion of the SIJ injection occurs by evaluating the patient’s pain level for up to 2 h postinjection while the long-acting anesthetic agent is working. If the patient has significant relief during this time, it is assumed that the SIJ is the pain generator. We feel that significant pain relief is equal to or greater than a 70 % reduction in pain. It is then hoped that the steroid that was injected with the anesthetic agent will successfully cause pain relief within 24–48 h and last for weeks to months. If an injection successfully diagnoses the SIJ as the pain generator and the pain is relieved for a long period of time, then another injection can be done if the pain returns to its previous preinjection level. If the injection was diagnostic but did not provide long-lasting relief, then there is no reason to repeat the injection unless a diagnostic block is once again required or the clinician is considering an extra-articular source of the SIJ pain and wishes to perform an extra-articular injection. At any time that the patient’s response to the injections results in questioning the SIJ as being the pain generator, the lumbar spine should be reevaluated as a possible source of the pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







