Fig. 9.1
Lateral X-ray of the elbow showing a supracondylar fracture
Fig. 9.2
Ossification centers in a skeletally immature elbow
Lateral Condyle Fractures
Lateral condyle fractures are the second most common fractures of the elbow in pediatrics [26]. They can occur with a fall on an outstretched, supinated hand, transmitting a force to the lateral condyle through the extensors of the forearm. Contrary to supracondylar fractures, displaced fractures may only present with pain and swelling. The skin and neurovascular function should be examined in each child. Traditional elbow radiographs are helpful in diagnosis, with the internal oblique view being the most accurate. Figure 9.3 demonstrates a lateral epicondyle fracture seen on X-ray. Non-displaced fractures can be treated with immobilization, while fractures displaced 2–4 mm and fractures displaced greater than 4 mm and rotated require ORIF. There is a risk for displacement in these fractures, so close follow-up with X-rays every 1–2 weeks is necessary. After bony healing and resolution of pain, the athlete can return to play.
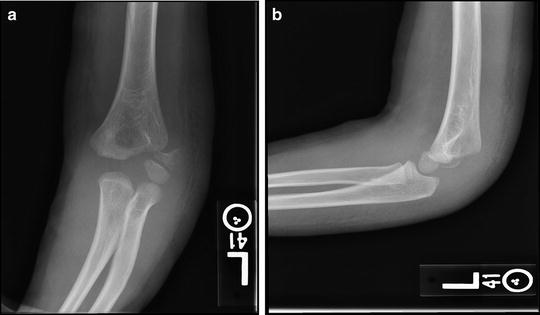
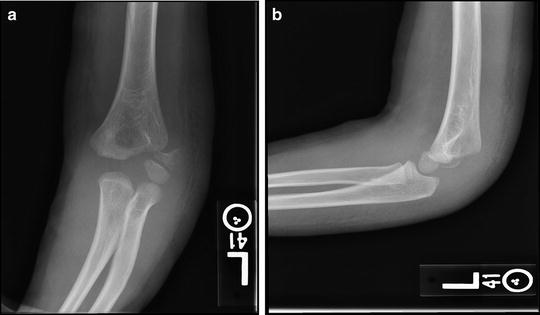
Fig. 9.3
AP (a) and lateral (b) X-rays of a lateral condyle fracture
Medial Epicondyle Fractures
Medial epicondyle fractures occur in approximately 10 % of all pediatric elbow fractures, the majority of which occur in children and adolescents aged 10–14 years. They occur more commonly in males compared to females, with a ratio of 3 to 1. These fractures can be associated with elbow dislocation [27]. The medial epicondylar apophysis can be avulsed by the attachments of the flexor-pronator mass and the medial collateral ligament (MCL). This can be seen with traumatic avulsions and in throwing athletes [29]. The mechanism is a valgus stress in combination with the contraction of the flexor mass. A fall on an outstretched hand is also a common mechanism.
On physical exam, patients have pain and swelling over the medial elbow and can have associated valgus instability. AP, lateral, and oblique X-rays of the elbow are essential for diagnosis (Fig. 9.4). Non-displaced fractures and fractures with less than 5 mm of displacement can be treated in immobilization with the elbow in flexion for 1–3 weeks. Fractures with greater than 5 mm displacement, especially in the throwing athlete, require operative intervention. Similar to other pediatric elbow injuries, athletes can return to play after fracture healing and resolution of symptoms.


Fig. 9.4
AP X-ray of medial epicondyle fracture
Forearm Fractures
Forearm fractures are very common in pediatric patients. The mechanism is typically a fall on the outstretched hand. Single-bone forearm fractures can be associated with a distal or proximal radioulnar articulation injury. These are classified as either the Monteggia or Galeazzi variants, and the different variations are shown in Fig. 9.5. The Monteggia variant fracture involves the ulnar shaft with radial head dislocation [30]. Galeazzi variant fractures occur with radial shaft fracture and associated distal radioulnar joint (DRUJ) dissociation [31]. On physical exam, these fractures are often displaced and carry an obvious deformity. AP and lateral X-rays of the forearm are necessary, as well as wrist and elbow X-rays to rule out any associated injuries as described above. Most pediatric forearm fractures can be treated nonoperatively in a cast for 6–12 weeks. Displaced fractures require surgical intervention with pins, intramedullary nails, or plate and screws. Return to activity can begin with evidence of fracture union.
Fig. 9.5
Monteggia fracture variants: (a) type I, (b) type II, (c) type III, and (d) type IV
Wrist and Hand
Distal Radius and Ulnar Fractures
The distal radius is the most common fracture of childhood, and can be associated with DRUJ disruption, although this is not common [26, 32]. Patients will present with pain and swelling of the wrist. There can be a deformity associated with displaced fracture patterns. Imaging should involve X-rays of the wrist as well as the affected elbow to rule out other associated pathology. Physeal injuries and fractures through the growth plate are common, as these areas are weaker than the surrounding bone. Salter-Harris fractures occur through the growth plates. Typically closed reduction with longitudinal traction is enough to reduce the fracture and splinting with transition to a cast over 4–6 weeks is indicated. Children younger than 10 years old can tolerate sagittal alignment less than 15° and dorsal angulation of 30°, whereas children 10 years and older can only tolerate sagittal misalignment less than 10° and dorsal angulation less than 20° [26]. Fractures exhibiting larger displacement and angulation may require closed reduction with percutaneous pinning, with pins in place for 3–4 weeks with casting and radiographic evaluation for healing [27]. Once the fracture has healed, patients can progress their activity as tolerated and return to sports.
Triangular Fibrocartilage Complex Injuries
The most common mechanism of triangular fibrocartilage complex (TFCC) injuries is a fall on an extended wrist with the forearm pronated or traction to the ulnar aspect of the wrist. This usually manifests as ulnar-sided wrist pain, and pain in the wrist with ulnar or radial wrist deviation or painful pronation and supination of the wrist [33, 34]. Patients often have pain when attempting to rise from a seated position using the wrist to push off. X-rays of the wrist should be taken to rule out any fractures. MRI is the gold standard to diagnose a tear and has largely replaced arthrography, although wrist arthroscopy is the most accurate means of diagnosis. Acute injuries to the TFCC are treated with nonsteroidal anti-inflammatories (NSAIDs), immobilization in a cast or brace, and, in some instances, steroid injections. Arthroscopic debridement can be performed in instances where initial treatment fails [27]. Direct surgical repair should be performed for more peripheral tears, and acute tears have better surgical outcomes than chronic tears. In the case of an ulnar-positive variance, an ulnar shortening osteotomy should be considered in order to address the potential cause of TFCC issues [26]. Therapy is usually started about 6 weeks postoperatively and continued for 6 weeks, after which the athlete is allowed to return to activities.
Carpal Fractures
The scaphoid is the most common carpal bone fractured in children and adolescents, and is also the most common carpal bone fractured during athletic activity. The incidence can be as high as 1 in 100 football players per year [33, 35]. The mechanism is usually a forced dorsiflexion with the wrist in ulnar deviation [26, 27]. Scaphoid fractures are characterized by degree of displacement and location, such as at the distal pole, waist, and proximal pole. Fractures at the waist are most common and displacement of over 1–2 mm can place patients at risk for nonunion [26]. Avascular necrosis (AVN) or osteonecrosis is a complication associated with scaphoid fractures secondary to frequent disruption of its blood supply at the time of injury.
The other carpal bones are injured with less frequency. Capitate fractures are less common than scaphoid fractures; however, they can also be associated with AVN. The capitate is usually fractured from a direct blow to the dorsum of the wrist or a forced dorsiflexion or volar flexion; however, they can be seen with perilunate and lunate dislocations as well [26]. The pisiform is a sesamoid carpal bone which rarely can be fractured with direct trauma to the volar and ulnar aspect of the wrist. Triquetrum fractures can result from hyperextension injuries with impingement of the distal ulna on the triquetrum, causing an avulsion from the dorsal cortex. Hamate fractures occur most commonly at the hook associated with direct force from a fall or impact with a bat, club, or racquet. Patients usually present with pain in the hypothenar eminence and occasionally will develop ulnar neuropathy as both the ulnar nerve and artery pass nearby in Guyon’s canal [25–27]. Hamate body fractures are less common but can be seen with dorsal dislocation of the ring and small finger metacarpal bones [26].
A standard wrist radiograph series is usually sufficient; however, scaphoid fractures require an additional scaphoid view, and hook of hamate fractures require a carpal tunnel view for diagnosis. Nonoperative treatment consists of cast immobilization. Operative intervention is reserved for displaced fractures. Patients are allowed to return to athletic activity when the wrist is non-tender on examination.
Metacarpal Fractures
Hand fractures are increasingly common in adolescent athletes. In some literature, upper extremity injuries accounted for over 80 % of all injuries sustained [33]. Basketball, baseball, football, and inline skating demonstrate the highest incidence of hand injuries. Some studies found that hand injuries accounted for 40 % of football and skating injuries, and that 29 % of all sport-related fractures occurred in the phalanges, while 13 % occurred in the metacarpals [6, 26, 35]. Combined, the phalangeal and metacarpal fractures account for 41.2 % of fractures [35]. Other sports also place the metacarpal bones at risk, such as skiing and snowboarding, football, rugby, and boxing [33].
Physical exam reveals swelling and tenderness over the affected digit. AP, lateral, and oblique X-rays of the hand are essential for diagnosis. The majority of fractures can be treated nonoperatively. Operative indications include open injuries, unstable fracture patterns as in the fracture pattern in Fig. 9.6, malrotation of the digits, and multiple metacarpal fractures. Early motion is initiated and the pins are usually removed at 4 weeks. Return to play is allowed with resolution of tenderness and bony union.


Fig. 9.6
AP (a) and oblique (b) X-rays of small finger metacarpal base fracture
Thumb Collateral Ligament Injuries
Acute UCL rupture of the thumb metacarpal phalangeal (MCP) joint, or skier’s thumb, is typically seen in skiers and snowboarders who fall on an outstretched hand with the thumb extended [27]. A valgus stress is placed on the thumb causing rupture to the UCL [36]. Swelling and tenderness are present on the ulnar aspect of the thumb. Valgus stress X-rays may be used to diagnose UCL ligament injury as well [36]. Occasionally, a Stener lesion can occur as the torn ligament becomes interposed between the adductor pollicis, preventing healing of the ligament. This can be seen on MRI and requires urgent surgical intervention to correct, as the ends of the torn tendon are unable to attach to one another due to the gapping with the interposed adductor muscle [27]. Surgical intervention in pediatric patients involves direct ligament repair with immobilization for 4–6 weeks in a thumb spica cast and ultimately a removable splint [25–27]. After the cast is removed, motion is begun and the athlete can return to sport at approximately 3 months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







