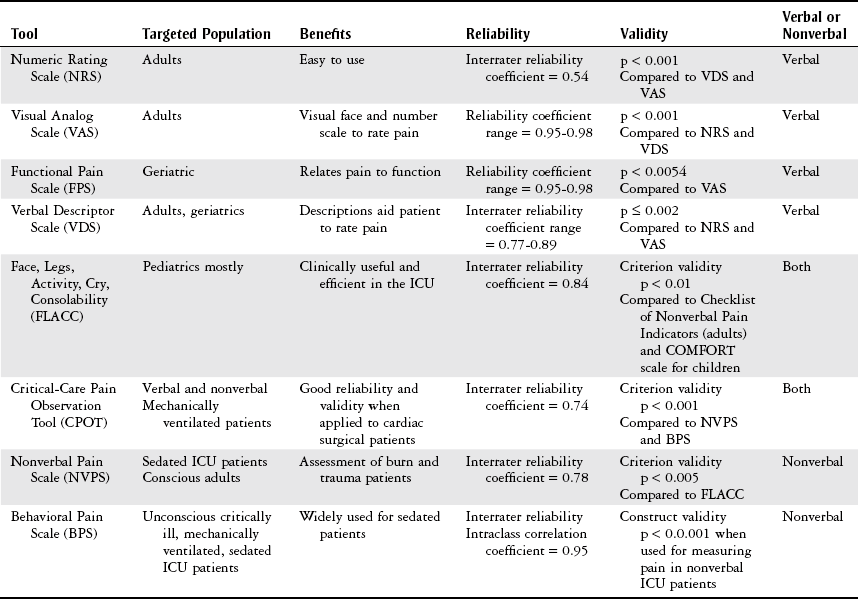
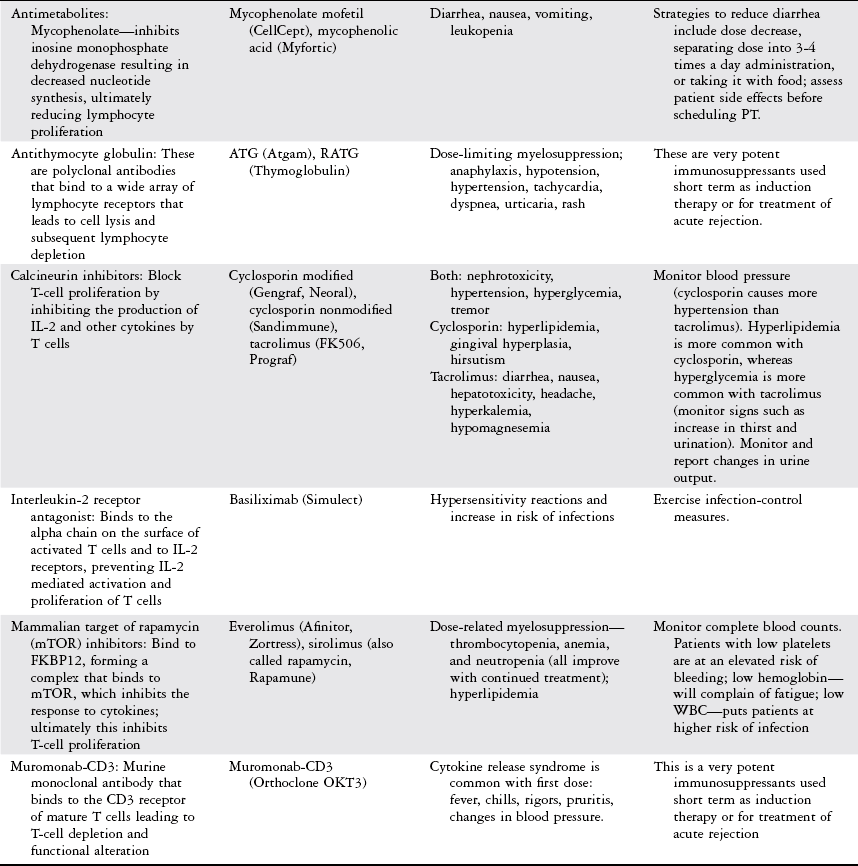
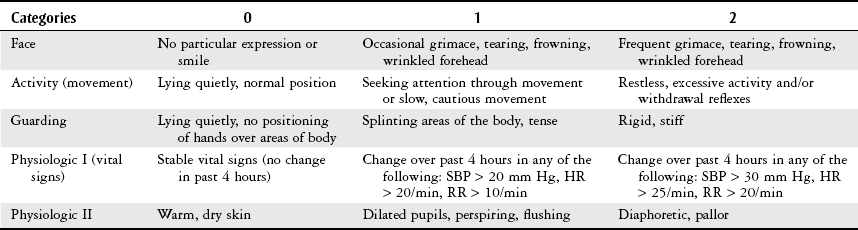
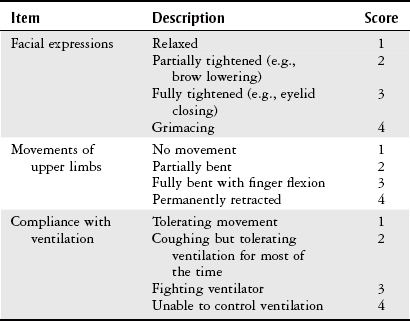
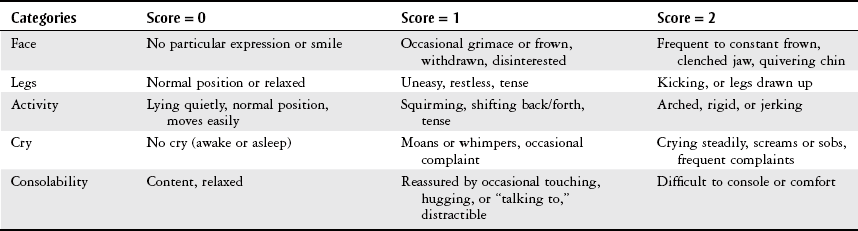
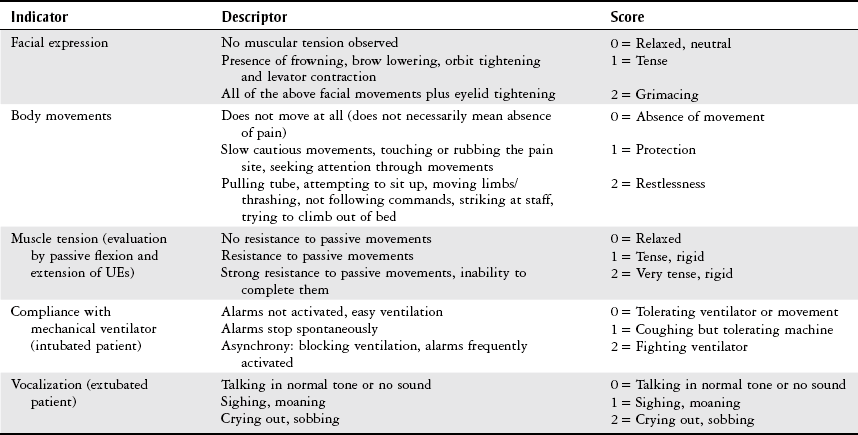
Chapter 21 The objectives of this chapter are to provide the following: 1 An overview of pain evaluation scales most applicable to the acute care setting 2 A description of physical therapy considerations when evaluating pain 3 An overview of commonly utilized management strategies for acute pain including pharmacologic agents 4 A brief description of physical therapy management strategies for acute pain Pain is multifactorial in nature and applies to many body systems. For this reason, specific practice patterns are not delineated in this chapter. Please refer to Appendix A for a complete list of the preferred practice patterns in order to best delineate the most applicable practice pattern for a given diagnosis. This chapter provides information on the evaluation and management of acute pain with the goal of facilitating patient care. The characteristics of acute pain include less than 6 months in duration, often associated with tissue damage such as surgery or traumatic injury, the cause of pain is easily recognized, pain can be treated readily, and the duration of pain is predictable.1 Acute pain in the medical patient may result from nonsurgical abdominal pain, renal or biliary stones, and phantom limb pain.2 The subjective complaint of pain is often difficult to objectify in the inpatient setting. Patients may be mechanically ventilated, pharmacologically sedated, or in too much pain to articulate their discomfort.3 Furthermore, patients who may be cognitively impaired are at higher risk for their pain to be undertreated with a resultant decreased quality of life.4–6 Despite these difficulties, an effective pain treatment plan depends on an accurate evaluation of the patient’s pain.7,8 Each evaluation requires a complete physical and diagnostic examination of the patient’s pain. The criterion standard for pain assessment is through self-report by the patient because it is the most accurate indicator of the existence or intensity of his or her pain, or both.4,5,9 The goal for evaluation should be directed toward individualization while maintaining consistency among patients. To assist with this process, various pain-rating tools have been developed to address both verbal and nonverbal (conscious or unconscious) patients. Verbal pain scales (Table 21-1) include: TABLE 21-1 Data from Kittelberger KP, LeBel AA, Borsook D: Assessment of pain. In Borsook D, LeBel AA, McPeek B, editors: The Massachusetts General Hospital handbook of pain management, Boston, 1996, Little, Brown, p 27; Carey SJ, Turpin C, Smith J et al: Improving pain management in an acute care setting: the Crawford Long Hospital of Emory University experience, Orthop Nurs 16(4):29, 1997; Wong DL, Hockenberry-Eaton M, Wilson D et al: Wong’s essentials of pediatric nursing, ed 6, St Louis, 2001, Mosby, p 1301; Puntillo K, Pasero C, Li D et al: Evaluation of pain in ICU patients, Chest 135:1069-1074, 2009; Gloth FM, Cheve AA, Stober CV et al: The functional pain scale: reliability, validity, and responsiveness in an elderly population, J Am Med Dir Assoc 2:110-114, 2001; Chanques G, Viel E, Constantin JM et al: The measurement of pain in intensive care unit: comparison of 5 self-report intensity scales, Pain 151:711-721, 2010. Nonverbal pain scales include: • Adult Nonverbal Pain Scale (Table 21-2) TABLE 21-2 HR, Heart rate; RR, respiratory rate; SBP, systolic blood pressure. From Odhner M, Wegman D, Freeland N et al: Assessing pain control in nonverbal critically ill adults, Dimens Crit Care Nurs 22:260-267, 2003. • Behavioral Pain Scale (Table 21-3) TABLE 21-3 From Payen JF, Bru O, Bosson JL et al: Assessing pain in critically ill sedated patients by using a behavioral pain scale, Crit Care Med 29(12):2258-2263, 2001. Pain scales used for both verbal and nonverbal patients include: • Face, Legs, Activity, Cry, Consolability (FLACC) scale (Table 21-4) TABLE 21-4 Indication: For nonverbal patients, particularly the pediatric population. From Merkel SI, Voepel-Lewis T, Shayevitz JR et al: The FLACC: a behavioral scale for scoring postoperative pain in young children, Pediatr Nurs 23(3):293-297, 1997. • Critical Care Pain Observational Tool (CPOT) (Table 21-5) TABLE 21-5 Critical-Care Pain Observation Tool (CPOT) Modified from Gélinas C: Nurses’ evaluations of the feasibility and the clinical utility of the Critical-Care Pain Observation Tool, Pain Manag Nurs 11(2):115-125, 2010. The validity of these scales may be improved by asking the patient about his or her current level of pain, rather than asking the patient to speculate about “usual” or “previous” levels of pain.10 The therapist should be aware that some physiologic indicators exist normally in critically ill patients. One needs to analyze the behavioral trend and differentiate pain from physiologic changes.12 The Adult Nonverbal Pain Scale is targeted toward adult patients who are intubated and sedated and is adapted from the FLACC Pain Assessment Tool.12 The Behavioral Pain Scale (BPS) is used for mechanically ventilated, sedated patients in the intensive care unit (ICU).4 Validity measured by BPS scores increase with painful stimuli.13 Good construct validity (p < 0.001) has been reported for the FLACC as evidenced by decreased pain scores after administration of analgesics and from painful to nonpainful situations. The FLACC has also demonstrated good interrater reliability when assessing pain in critically ill patients.14 This was consistent when compared among use with adults, children, and patients who are mechanically ventilated. However, there is some disagreement concerning the use of this scale with adults because of their inability to demonstrate some behaviors associated with the pediatric population. Those who disagree suggest utilizing the NVPS, as it has good interrater reliability and validity with critically ill, sedated, mechanically ventilated, and/or cognitively impaired adults.12,14,15 The CPOT was developed to assess pain in critically ill ICU patients and was mainly used with those recovering from cardiac surgery. It is reliable and valid in this population and further research is required for its use in other populations.16 The CPOT can be used with both verbal and nonverbal patients.4,16 • Observe pain-related behaviors to appropriately select an assessment tool. Use nonverbal assessment tools when self-report is unattainable.5 • Select the appropriate tool based on the clinical environment and relevance to the specific patient population.5 • Table 21-6 provides a comparison of the various pain scales to aid in selecting an appropriate tool. The VAS and NRS tend to be used commonly in the clinical setting.5,17
Acute Pain Management
Preferred Practice Patterns
Pain Evaluation
Physical Therapy Considerations for Pain Evaluation
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Acute Pain Management
Only gold members can continue reading. Log In or Register to continue