Fig. 8.1
Salter-Harris classification system
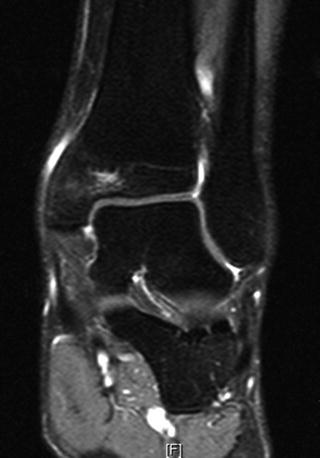
Fig. 8.2
Type V Salter-Harris lesion of the distal tibia of a 22-year-old athlete
Distal femoral fractures in adolescents result either from high-energy trauma or a sports-related injury. A careful neurovascular examination of the injured extremity is necessary. For nondisplaced Salter-Harris Type I and II physeal fractures, conservative management with a long leg cast is usually adequate. For displaced Salter-Harris Type I or II fractures with a small metaphyseal fragment, closed reduction and stabilization with percutaneous pins or Kirschner wires is indicated. Displaced Salter-Harris Type III and IV fractures warrant anatomic reduction and fixation [15]. Cannulated compression screws placed across the fracture and parallel to the physis are commonly used. Even after proper treatment, up to 50 % of distal femoral physeal fractures may result in growth disturbance [16]. A high risk of limb length discrepancy or angular deformity has been reported after Salter-Harris Type II injury [16].
Proximal tibial physeal fractures occur with valgus or hyperextension force on a fixed knee. The principles of treatment are similar to those for distal femoral physeal fractures. A CT scan is recommended for Salter-Harris Type III and IV fractures involving the tibial plateau. Neurovascular injuries and compartment syndromes are not uncommon, and they should be kept in mind.
Ankle physeal injuries account for 15–38 % of all physeal injuries. Injury patterns are a consequence of the physeal anatomy and the patient’s age [17]. The distal tibial physis appears by 1 year of age and closes by 12–14 years of age in girls and by 15–18 years of age in boys. The distal fibular physis appears by 2 years of age, and closes by 19–20 years of age. The medial malleolar ossification center appears at 1–2 years of age and closes by age 12 years [18]. The distal tibial physis closes in a circular pattern from the center to medial to lateral. During normal development, the medial and posterior tibial physeal plates close first, followed by the anterolateral areas. The fracture patterns reflect the areas of the physis that are still open.
The Tillaux fracture is a Salter-Harris Type III fracture of the anterolateral portion of the distal tibial epiphysis (Fig. 8.3). It occurs late in adolescence when the medial and posterior plates have closed and the anterior growth plate is still open. The mechanism of injury is forceful external rotation. As the ankle is stressed medially, the pull of the anterior tibiofibular ligament results in an avulsion fracture of the anterolateral aspect of the distal tibial epiphysis over the area of the physeal plate that is still not ossified. As Tillaux fracture occurs toward the conclusion of physeal closure, symptomatic growth arrest is rare [15]. A Tillaux fracture appears on anteroposterior radiographs as a vertical line through the epiphysis. It can be managed nonsurgically, with a closed reduction in internal rotation of the foot, but these fractures often require open reduction internal fixation (ORIF) to restore the joint surface and prevent articular degeneration.
Fig. 8.3
Tillaux fracture
A triplane fracture is a multiplanar Salter-Harris Type IV fracture of the ankle, which involves all three planes of the distal tibia. Patients are usually younger than those with a Tillaux fracture. A CT scan is useful to assess the fracture pattern, plan surgery, and obtain anatomical reduction of the joint surface [15, 19].
Apophyseal Avulsion Fractures of the Hip and Pelvis
Apophyseal avulsion fractures occur in growing teens involved in sports, particularly sprinters, distance runners, and soccer and tennis players. They usually result from a sudden forceful concentric or eccentric contraction of the muscle attached to the apophysis, which is an area of growth cartilage where muscles and tendons attach. Soccer and gymnastics have documented the highest number of avulsion fractures [20]. Although apophyseal avulsion fractures of the hip and pelvis usually affect adolescents, with a mean age of 13 years, they can occur in older patients, as the apophyses close at 25 years old (range 4–25 years) [21]. The most common locations were the ischial tuberosity (IT—54 %), anterior inferior iliac spine (AIIS—22 %), anterior superior iliac spine (ASIS—19 %), superior corner of pubic symphysis (PS—3 %), and iliac crest (IC—1 %) [20]. Apophyseal avulsion fractures of the greater trochanter have also been reported, and although rare, bilateral avulsion fractures can occur [22, 23].
Apophyseal injuries of the pelvis are usually acute. The young athlete feels shooting pain referred to the involved tuberosity. The clinical exam reveals pain and local tenderness during movement of the affected limb or during abdominal movements, as well as restricted range of motion and weakness. However, they can also be the result of a neglected and/or misdiagnosed injury and, if not properly diagnosed and treated, they can result in a chronic, debilitating problem. Plain radiographs are usually sufficient for diagnosis [20]. Classification is usually based on the location and amount of displacement.
Most patients can be managed conservatively. After a short period of rest, ice, and analgesics, patients can start gentle passive and active motion. Once 75 % of motion is regained, patients may progress to guided resistance exercises, usually at 3 weeks after injury. Approximately 1–2 months after injury, patients can begin stretching and strengthening exercises with an emphasis on sports-specific exercises. They should return to competitive sports no earlier than 2 months after injury. Surgical intervention is indicated for displacement of 2–3 cm, painful nonunion, inability to return to competitive sports, and exostosis formation [24]. Kautzner et al. reported faster recovery and better compliance with rehabilitation protocols in patients with fragment displacement treated surgically [25]. They concluded that the indication for surgical treatment is the grade of fragment displacement and the patient’s sporting activity.
Knee Injuries
Anterior Cruciate Ligament Injuries
In skeletally immature patients the collagen fibres of the ACL form a strong connection between the ligament, the perichondrium, and the epiphyseal cartilage. As ligaments are stronger than growth plates, knee injuries most often result in physeal injuries or tibial spine avulsion (80 % of children under 12 years old with ACL trauma) [26]. However, as the number of children and adolescents participating in competitive sports is growing, ACL tears are becoming more common, up to 90 % of cases in children older than 12 years old [26]. Recent reviews reported ACL injury in about 50–70 % of cases of knee hemarthrosis [27].
Several authors reported that young female athletes are at greater risk of sustaining ACL injuries, probably because of differences in joint laxity, hormones, anatomy (narrow notch width), neuromuscular function, and training [28, 29]. Up to 50 % of ACL ruptures in elite female athletes occurred during the menstrual phase of their cycle [30]. However, more recent research with more patients did not show any statistically significant difference in the proportion of male and female athletes who sustained an ACL tear [6].
Plain radiographic evaluation is essential to exclude bone injuries, while MRI can confirm a diagnosis based on an accurate clinical examination.
The management of ACL lesions in this age group is controversial. Conservative management with extensive rehabilitation and return to activities wearing a brace until skeletal maturity and growth plate closure followed by delayed anatomic ACL reconstruction to allow an anatomical adult-like reconstruction was the treatment traditionally preferred [31]. However, early surgical treatment is now advocated for ACL-deficient and unstable knees [32]. Longitudinal studies found that about 70 % of young athletes who suffered an ACL injury developed moderate knee osteoarthritis within 10–15 years [33]. A recent meta-analysis showed that conservative treatment can result in severe instability, high rate of meniscal tears, early degenerative osteoarthritis, and poor recovery in sports [34]. Delay of as little as 5 months between ACL injury and surgery was associated with high risk of a medial meniscal tear, which increases steadily in frequency more than 1 year after ACL injury [35]. Therefore, the importance of early surgical ACL reconstruction has recently been emphasized [36].
When ACL surgical reconstruction is performed, there is potential risk for iatrogenic injury to the physis. This could lead to growth disturbance, as the proximal tibia contributes 55 % to the growth of the leg, and the distal femoral physis contributes 70 % to the growth of the femur. Many different surgical techniques have been described to minimize risks and complications to the physis, and extra-physeal reconstruction or partial/complete transphyseal techniques are available [37]. Transphyseal repair involves a tunnel being drilled across both the tibial and femoral physis. This procedure allows ideal tunnel placement, and improves graft longevity and knee function, but the incidence of growth disturbance may increase, especially in very skeletally immature children [37]. Partial transphyseal techniques avoid the distal lateral femoral physis, providing more isometric tibial graft positioning, and provide excellent stability and return to sport. More anatomic physeal-sparing reconstruction techniques seem to be promising, but are technically demanding [2].
Conservative treatment can be considered for partial ACL tears. Good outcomes have been reported in patients younger than 14 years with a partial ACL tear and a stable knee treated conservatively [38–40]. One series reported that only 31 % of such patients required reconstruction [38].
Prevention of injuries is very important. Training programs during the preseason focused on strengthening, neuromuscular, and proprioceptive training supervised by qualified personnel seem to be effective to prevent ACL lesions [41].
Posterior Cruciate Ligament Injuries
The posterior cruciate ligament (PCL) is the primary restrain to posterior tibial translation and is a secondary restraint to external rotation. PCL injuries are less common than ACL injuries. Three mechanisms have been proposed for PCL tears: a direct blow to the anterior surface of the tibia, hyperflexion, and hyperextension. Noncontact injuries, such as forced hyperflexion, have been reported to be the most common isolated PCL injury mechanism in athletes [42]. PCL injuries can be classified according to severity (grades I–III), timing (acute versus chronic), and presence of associated injuries (isolated versus combined) [43].
Avulsion fractures are frequently associated with PCL injuries in children and adolescents, so plain radiographs are necessary. The attachment site may not yet have ossified; thus, avulsion of the PCL, especially from the femur, may not be appreciated on plain films. In the skeletally immature knee, MRI can accurately differentiate between intrasubstance and complete tears and determine associated chondral or meniscal disease. Partial ligament tears can be difficult to distinguish, even with MRI. In this case arthroscopy and examination under anesthesia remain the most accurate means of diagnosis [44].
PCL injuries are not as benign as previously thought [39]. Nonoperative treatment with the knee immobilized in a cast in full extension to reduce posterior translation was considered the first-line approach to PCL injuries in the pediatric population because of the high risk of physeal injury leading to growth arrest or angular deformity. However, treatment should consider the type of ligamentous injury (partial or complete), the site (avulsion or midsubstance), the grade (partial or complete), and the presence of any associated injuries (meniscal or chondral injuries). Soft tissue PCL avulsions from the femur or tibia should be repaired primarily with transosseous (intraepiphyseal) sutures through drill holes. Bony avulsions can be repaired with either screw or transosseous suture fixation. Isolated midsubstance PCL tears can be managed conservatively in skeletally immature patients with good results [45], particularly those with less than 8 mm of posterior displacement on stress radiographs [45]. PCL reconstruction is a viable treatment option in patients with multi-ligament injuries or those with isolated PCL injury who have failed conservative treatment, with outcomes related to the severity of the initial injury.
Medial and Lateral Collateral Ligament Injuries
Isolated medial and lateral collateral ligament (MCL, LCL) injuries are uncommon in pediatric athletes, but are more frequently associated with an ACL tear and multilayer knee instability [1]. MCL tears occur after a valgus or rotatory stress to the knee. Injuries of the MCL are well evaluated with MRI, which can show a ligament tear, lateral bone marrow edema due to the valgus stress forces, and medial bone marrow edema due to the microavulsive injury [46]. Injuries of the MCL are commonly classified according to Hughston classification as grades 1–3 [47]. Avulsion fractures of the proximal MCL are called Pellegrini-Stieda lesions [47]. Incomplete and isolated tears of the MCL are commonly treated nonoperatively with early functional rehabilitation with good results, but when ACL tear and multilateral knee instability are associated, they require surgical reconstruction [48].
Isolated LCL injury is very rare in the pediatric population, but can be associated with tears of the ACL and injuries to the posterolateral corner structures [49]. A Segond fracture is an avulsion fracture of the lateral tibial plateau and is commonly associated with ACL injury [49]. The management of isolated LCL tears is conservative. Failure to recognize and repair the posterolateral corner injuries is the reason for failure of ACL reconstruction and persistent knee instability [49].
Meniscal Tears
Meniscal injuries involve 5 % of patients younger than 15 years, particularly children and adolescents participating in football, soccer, and basketball. Isolated meniscal tears most frequently involve the medial meniscus, while the lateral meniscus is frequently injured in case of ACL injury with an unstable knee and discoid meniscus [50]. Discoid meniscus is abnormally shaped with different histological and mechanical properties from the normal meniscus. The ultrastructure of discoid meniscus is significantly different and the collagen fibrils are less in number and misaligned [51]. Discoid menisci cannot control the coordination of the tibiofemoral joint, absorb shock, or reduce mechanical pressure on articular cartilage; thus they quickly become worn and the incidence of tears is increased [52].
Young athletes may describe a “pop” heard or felt after a twisting event. Symptoms include pain, effusion, snapping, giving way, and less frequently locking. However, the diagnosis can be difficult because clinical exam is often subtle and nonspecific, leading to possible delay in diagnosis and/or misdiagnosis. Physical examination may reveal joint line tenderness and effusion. The McMurray test is considered positive when the child feels pain with provocative rotation at 30–40° of flexion. The differential diagnosis is discoid meniscus, popliteal tendinopathy, patellofemoral pain, and osteochondritis dissecans. Radiographs can exclude bone lesions or tumors. MRI can detect meniscal pathology when clinical evaluation is inconclusive.
Treatment of meniscal tears in children and adolescents is controversial. Current literature suggests surgical treatment but recent studies showed poor outcome after partial or total meniscectomy [53], with 75 % remaining symptomatic and 80 % showing radiographic signs of osteoarthritis at 5-year follow-up [54]. Therefore, meniscal repair has been suggested.
Arthroscopic meniscal repair is the treatment of choice [55, 56]. Factors shown to correlate with increased healing of meniscal injuries include younger age, peripheral tears (within 3 mm of meniscal rim), lateral meniscus tears, concomitant ACL reconstruction, surgery within 8 weeks of injury, and tear length less than 2.5 cm [57]. Partial meniscectomy is indicated for more complex meniscus injuries.
Acute Patellar Dislocations
Traumatic patellar dislocation is common in young athletes, and accounts for approximately 3 % of all knee injuries [58]. It occurs about 2/3 of the time in active patients under the age of 20 years. Girls are more likely to sustain a patellar dislocation than boys. Patellar dislocations are often the result of a direct blow or fall onto the knee, but can also occur without contact. A common example is a right-handed baseball player who rotates on his foot while swinging the bat.
The medial patellofemoral ligament (MPFL) is the primary passive restraint to lateral patellar translation at 0–30° of knee flexion [59]. The MPFL is commonly injured after acute patellar dislocation. MRI studies demonstrated an MPFL injury in up to 100 % of patients [60], and is, together with medial retinacular tears, the major cause of hemarthrosis. Osteochondral fractures are common after patellar dislocations, occurring in nearly 25 % of cases [61].
Imaging should include plain radiographs and MRI. Standard plain radiographs and Mercer-Merchant view with the patient supine and the knee flexed 45° can show an osteochondral fracture of the medial facet of the patella. MRI can evaluate osteochondral injuries of the patellofemoral joint and the location and extent of soft tissue damage to the medial patellar stabilizers, including the medial retinaculum, MPFL, and vastus medialis obliquus.
Primary patellar dislocation is usually managed nonoperatively, with acute surgical repair indicated for chondral lesions or fractures [62]. Recurrent dislocations are relatively common, with recurrence rates up to 45 % [63]. In up to 80 % of patients, recurrent instability is attributed to predisposing factors, such as immature physis and trochlear dysplasia [63]. Surgical treatment for traumatic patellar dislocation is still debated. Some studies found no statistically significant differences in the incidence of re-dislocation and functional scores between nonoperative and operative treatment [64]. Other authors reported lower functional results in case of osteochondral fracture [59, 62]. For these reasons a gold standard treatment is still not available [63]. Treatment should be individualized based on preoperatory findings and the patient’s activity level.
Ankle Injuries
Ankle injuries are the most common injuries sustained by high school athletes, accounting for 16 % of all sports-related injuries [65], and 10 % of all injuries seen in EDs [66]. Ankle sprains are the most common (88.7 % of all ankle injuries), and lateral sprains are more common than isolated medial ligament injuries, accounting for 85 % of injuries. American football accounted for most high school ankle sprains (24.1 %), followed by soccer (15–18 %), basketball (12 %), and volleyball (10 %) [67]. Even though the overall rate is comparable between the two sexes, in gender-comparable sports such as soccer, volleyball, and basketball, ankle sprain rates were higher in girls than boys [6].
Patients with acute ankle sprains usually respond to nonoperative measures, including physical therapy and functional rehabilitation. One study showed that functional rehabilitation in patients engaged in regular activity allowed earlier resumption of sports training with fewer symptoms compared to cast immobilization [68]. Most ankle sprains cause athletes to miss less than 7 days of activity (51.7 %), with 33.9 % causing 7–21 days lost, and 10.5 % causing more than 22 days lost. Injuries involving multiple ligaments resulted in more time lost. Only 0.5 % of ankle sprains were treated surgically.
Although ankle sprains are commonly treated with a high rate of success, they may result in pain and disability in the short term; recurrent sprains, chronic ankle instability, decreased sport activity, and early retirement from sports in the midterm; and secondary injuries and early osteoarthritis in the long term. Recurrent ankle sprains accounted for 15.7 % of ankle injuries. Sports with the highest proportion of recurrent ankle sprains were cheerleading (20.8 %), boys’ basketball (20.1 %), and girls’ gymnastics (20.0 %) [66]. Talar dome injuries are complications of lateral ankle sprains, and occur in up to 6.5 % of cases. They should be suspected if there is ongoing pain and persistent effusion or occurrence of intermittent swelling of the joint.
Foot Injuries
Foot fractures account for 5–13 % of pediatric fractures [18]. Metatarsal fractures are common in children and adolescents participating in sports. These usually occur indirectly as a result of torsional forces and avulsions or from direct trauma. The incidence of first metatarsal fractures is highest in children under 5 years of age. This has been called the “bunk bed fracture” because of its common mechanism [71]. The fifth metatarsal is the most common metatarsal fracture in children, occurring 45 % of the time and in 90 % of children greater than 10 years of age [66]. It occurs after an inversion-type injury, when the peroneus brevis tendon is avulsed from its attachment at the base of the fifth metatarsal. The treatment is usually conservative, with a short leg walking cast for 3–5 weeks. If displacement is greater than 2–3 mm, surgical reduction and internal fixation are needed [72]. However, only a few level I evidence-based studies are published; therefore, the treatment is often empiric and based on surgeon personal experience.
The Jones fracture is a transverse fracture at the junction of the diaphysis and the metaphysis of the fifth metatarsal without extension distal to the fourth intermetatarsal articulation. The average age of occurrence involves 15–21-year-old athletes, who usually describe a large adduction force applied to the forefoot while the ankle is plantar flexed [66]. These fractures are associated with high rates of delayed union, nonunion, and refracture because of poor blood supply. Therefore this fracture poses a difficult problem for the competitive athlete, for whom an early return to sport is important. A systematic review suggested that a nonoperative approach with non-weight-bearing immobilization resulted in a longer time to union and a higher number of delayed unions or nonunions compared with operative treatment [73]. A level I study comparing early screw fixation with casting for acute Jones fractures showed a statistically different union rate between the operative group (94 %) and the nonoperative group (67 %), and a median time to return to sports of 15 weeks in the cast group and 8 weeks in the screw group [74]. Treatment should be based on the personality of fracture and the patient. Nondisplaced Jones fracture can be treated conservatively with a non-weight-bearing cast for 6–8 weeks, while surgical reduction and internal fixation with a cannulated screw is the gold standard treatment in case of displacement. In case of nonunion, a plate fixation with autologous bone graft is indicated [66].
Lisfranc’s joint injuries are common in adolescents playing football. The keystones of Lisfranc’s joint are the first and second metatarsals articulating with the first and second cuneiforms. Stronger ligaments connect the plantar surfaces of the joint. The Lisfranc’s ligament is the stronger ligament and stabilizes the medial cuneiform with the II and III metatarsal bones; the transverse ligaments connect the plantar surfaces of the bases of the lateral four metatarsals. The most common mechanism of injury is an axial loading through the foot with the foot in forceful plantar flexion and slight rotation, which causes the proximal second metatarsal to dislocate dorsally [18]. The typical presentation involves an athlete with pain over the dorsum of the midfoot associated with swelling and an inability to bear weight, particularly on the tiptoes. Weight-bearing radiographs are needed to make the diagnosis. Lisfranc’s injuries can be treated in a cast boot for 4–5 weeks when the first and second metatarsal bones are not disrupted more than 2 mm with weight-bearing images. If there is widening of more than 4 mm surgery should be considered. A large reduction forceps is placed with the tips on the medial cuneiform and lateral second or third metatarsal base to reduce the dislocation. The dislocation is then fixed with a percutaneous screw fixation from the medial cuneiform to the second or the third metatarsal base [75]. Postoperative care is 4–6 weeks with boot immobilization and return to sports typically takes more than 4 months.
Hallux fractures occur most commonly in soccer [18] (Fig. 8.4). Closed injuries were diagnosed in 92 % of patients; 8 % of children presented with open fractures. The vast majority of children (86 %) were treated conservatively with rest and taping, while displaced fractures require reduction and percutaneous fixation with K-wire [18]. Because of the first toe’s role in weight bearing, balance, and pedal motion, deformity, decreased range of motion, and degenerative joint disease can impair a patient’s functional ability.


Fig. 8.4
Type V Salter-Harris fracture of the hallux in a young soccer player
There is an increasing incidence of “turf toe,” a sprain of the plantar capsule ligaments, in young athletes playing on synthetic surfaces and using lighter, more flexible shoes. The first metatarsal-phalangeal joint capsule is reinforced by a fibrocartilaginous plate, which is formed by the flexor hallucis, adductor hallucis, abductor hallucis tendons, and deep transverse metatarsal ligament (Fig. 8.5). The sesamoid bones are contained within the fibrocartilaginous plate. The usual mechanism of turf toe is hyperextension with the foot in slight dorsiflexion. Less common mechanisms of injury are hyperflexion, which occurs when the ball carrier is tackled from behind, and valgus stress [76]. The Lachman test of the first toe is useful to determine the stability of the plantar plate. Stress X-rays can show a proximal migration of the sesamoids, and MRI is used to confirm the plantar plate injury. For sprains of the plantar plate, with minimal or no retraction of the sesamoids, management includes planter flexion taping of the hallux and a walking boot for 2–3 weeks. Partial weight bearing is allowed at 3 weeks and full weight bearing at 4 weeks as symptoms allow. Surgical reconstruction is indicated if there is a complete tear of the plantar plate [77].