CHAPTER 128 Acute Intervention and Return to Play
INTRODUCTION
As a team physician, one has an opportunity to work with and treat athletes. Being a team physician requires a vast fund of knowledge, including familiarity with trauma protocols, musculoskeletal injuries, and medical conditions that affect the athlete. The team physician must be prepared, have an appropriate knowledge base of the sport, and be flexible enough to deal with a multitude of situations that may unexpectedly or emergently arise.1
The principal responsibility of the team physician is to provide for the athlete’s overall well-being, allowing all to maximize their potential. The team physician must take the responsibility of making medical decisions regarding the participant’s safety, and communicate effectively with coaches, athletic trainers, healthcare providers, the parents, and the athlete.1
Preparation is critical to effective and efficient management of sports-related injuries. With the appropriate equipment available, the proper personnel present, and a chain of command in place, each injury can be properly evaluated and appropriate medical decisions can be made to optimize the health and safety of the athlete. With each injury, a condition-specific medical history and physical examination, along with appropriate medical tests and consultations, help establish an accurate diagnosis to best direct treatment and ultimately make a decision regarding the athlete’s safe return to athletic participation.2,3
The purpose of this chapter is to outline how to evaluate and manage the injured athlete on the field, to highlight conditions that can occur during or as a result of active athletic participation, and to review current guidelines for decision-making regarding safe return to play for specific injuries. This information is also discussed in Chapter 127 (Epidemiology of Injuries) and in Chapter 126 (On the Field Assessment).
ON-FIELD EVALUATION
Proper preparation, which includes a chain of communication, education of medical personnel, easy access to emergency equipment and tools, and ambulance availability eases anxiety in the potentially tense situation of an athletic injury.4 Preparation enhances efficient and optimal management of the injured athlete. A comprehensive list of recommended on-site medical equipment is available in the Sideline Preparedness Consensus Statement.2 For spinal injuries, it is imperative to have a spine board with appropriate attachments, a semirigid collar, and a face mask removal tool, such as a screwdriver or bolt cutter.4,5 Other necessities besides ACLS equipment and medications include equipment for an urgent neurological evaluation, such as a flashlight, a reflex hammer, and a sharp object for sensory testing.4
On-field evaluation and management of neck or head injuries can be separated into five categories: (1) preparation for any neurological injury, (2) suspicion and recognition, (3) stabilization and safety, (4) immediate and possible secondary treatment, and (5) evaluation for return to play.6
When an injury occurs after an acceleration–deceleration impact to the head or neck, medical personnel must immediately evaluate the athlete for the possibility of a head injury, a spinal cord injury, or both.7 Indications of possible cervical spine or spinal cord injury include neck pain, numbness, or dysesthetic pain. Bilateral involvement or neurological deficits in the upper and lower extremities also suggest a possible spinal cord injury. In any case that a spinal cord injury cannot be ruled out, the athlete should have his or her neck immobilized, be positioned on a spinal board, and be transported to the nearest trauma center for further physician and radiological evaluation.8
The most important principle of injury management is to prevent further injury.9 If an athlete is downed and not moving, the athlete should be treated as though a brain injury and spinal cord injury have occurred,8 and immediate assessment of the ABCs (airway, breathing, and circulation) of trauma should ensue. Although the ABCs are of highest priority, extreme caution should be taken to avoid movement of the athlete in order to prevent further neurological injury. The head and neck of the athlete should immediately be immobilized in a neutral position.4,5,7 As standard trauma protocol management of the ABCs occurs, evaluation of the athlete’s level of consciousness should be undertaken. Neurological evaluation should consist of level of consciousness, pupil response, pain response, weakness, abnormal posturing, rigidity, or flaccidity.4,5
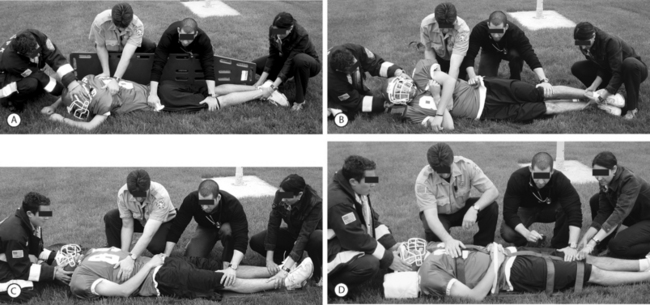
If the athlete is unconscious, the individual needs to be moved safely to a supine position to facilitate emergency management. If an athlete is face down and unconscious, he or she should be log-rolled to a face-up position while the neck is maintained in a neutral position.4,7 Ideally, the individual is log-rolled by four members of the medical team, with the leader controlling the head and neck and issuing the commands. The leader should maintain neck immobilization with slight cervical traction and employing the cross-arm technique to ease positioning throughout the roll. Each of the other three team members should control a specific region of the body, either the shoulder, hips, or the lower leg, as the athlete is rolled toward them. A fifth member can help with carrying and positioning as necessary (Fig. 128.1).4,10
If the injured athlete is wearing a helmet or shoulder pads, neither should be removed until the person has been transported to a trauma facility where appropriate clearance can be provided after a proper physician examination and radiological evaluation have been performed.4,10 When positioning a helmeted athlete on the backboard, the positioning of the head and neck must be done cautiously, as further injury can be caused if the helmet unintentionally causes flexion of the cervical spine.11 The spine should be maintained in a straight line during any movement or positioning. Once the player is on the board, straps and pads are used to secure the position.5
If the downed athlete is not breathing, the mouthpiece and face mask should be promptly removed to expedite airway access and cardiopulmonary resuscitation (CPR) management. A screwdriver, Trainer’s Angel, Face Mask Extractor, or bolt cutter should be used to remove the face mask while maintaining proper positioning of the neck. The jaw thrust maneuver is the preferred method of opening the airway in an individual with a potential cervical spine injury.4
The Inter-Association Task Force for Appropriate Care of the Spine Injured Athlete has outlined four situations in which the athletic helmet and chin strap may need to be removed on the field: (1) if the helmet and chin strap do not hold the head securely, meaning that immobilization of the helmet does not immobilize the head; (2) if because of the design of the helmet and chin strap the airway is unable to be maintained even after the removal of the face mask; (3) if the face mask cannot be removed in a reasonable time period; and (4) if the helmet prevents immobilization of the head in an appropriate position for transport.6,12,13 Emergency Medical Service (EMS) personnel may be more familiar with Advanced Trauma Life-Support (ATLS) protocols designed more specifically for motorcycle helmets, so communication among those managing an injured, helmeted athlete is critical.14
In cases in which the helmet has to be removed on the field, the athlete’s head must be supported at the occiput and the cervical spine kept in straight alignment. While the occiput is supported, the chin strap is removed and the team leader spreads the ear flaps and pulls the helmet off in a straight line with the spine.4 Efforts to maintain absolute immobilization should be continued until comprehensive evaluation at a trauma center can be completed.
INJURIES AND RETURN TO PLAY
As a physician involved in the care and treatment of athletes, one of the most challenging responsibilities is determining when an athlete is safe to return to competition. The physician needs to explain to the athlete the severity of the injury and the risk for reinjury or more severe injury. The physician must have a depth of knowledge about the sport, the nature of the injury and its course, and the potential sequelae to best counsel the athlete.1,15 Guidelines are available to help direct decision-making, but each case must be evaluated on an individual basis. Ultimately, the athlete, and when appropriate the coach and parents, must be given recommendations regarding return to play that are in the athlete’s overall best interest.3
Cervical spine injuries that are a result of athletic competition have been classified into three broad categories based on duration of symptoms or radiographic findings. The classification provides a general framework to develop an initial expectation for return to play (Table 128.1).5,15,16
Table 128.1 Classification of cervical spine injuries
| Type I | Type II | Type III |
|---|---|---|
From Warren and Bailes.11,15,16
Type I injuries are those in which the athlete acquires a permanent spinal cord injury. This class includes complete, and four variations of incomplete, spinal cord injury. The four types of incomplete spinal cord injury are Brown-Sequard, anterior spinal cord syndrome, central cord syndrome, and mixed-type of spinal cord injury. Furthermore, evidence of spinal cord pathology on radiographic studies also is classified as type I. Thus, evidence of spinal cord injury, whether clinical or radiographic, is an absolute contraindication to return to play in contact or high-velocity sports.5,16
Injuries that are classified as type II are those with neurological changes that are transient, resolving in minutes to hours, and without abnormalities on radiographic evaluation. Examples of type II injuries are transient quadriparesis and a variation of central cord syndrome known as burning hands syndrome (Fig. 128.2). Those athletes with type II injuries are not absolutely contraindicated from returning to play, but each case must be thoroughly evaluated on an individual basis. There is controversy regarding type II injuries and safe return to play. Certain criteria must be met for each specific type II injury before an athlete may return to play.5,16
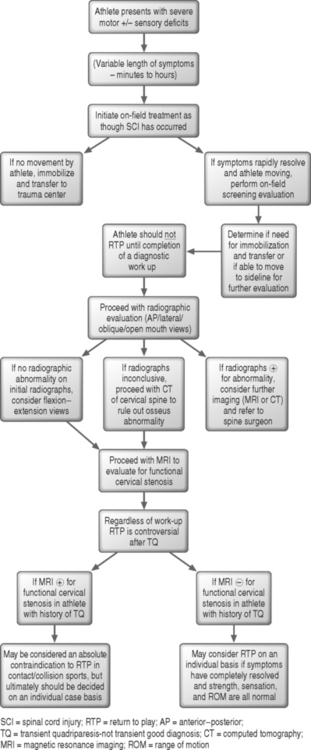
Fig. 128.2 Algorithm of transient quadriparesis. Information primarily from Wilberger11 and Allen and Kang.27
There is a condition in which spinal cord injury occurs though there is no evidence of fracture or osseous malalignment on either radiographs or computed tomography (CT). This condition has been termed ‘spinal cord injury without radiographic abnormalities’ (SCIWORA). This condition has largely been reported in the pediatric population, though it has also been described in the adult population.17 Because of the predilection for the pediatric population, SCIWORA has also been referred to in the literature as ‘pediatric syndrome of traumatic myelopathy without demonstratable vertebral injury.’18 SCIWORA has been theorized to occur more frequently in the pediatric population due to anatomical and biomechanical properties. Suggested reasons for increased incidence in the pediatric population include the following: (1) more horizontal orientation of facet joints in the pediatric population, (2) anterior wedging of the superior aspects of the vertebral bodies, and (3) more ‘elastic’ ligaments and joint capsules.17 These differences in the pediatric population, which are typically apparent until 16–18 years of age, allow for more intersegmental motion, potentially leading to neurological injury without apparent osseous or ligamentous injury. SCIWORA, which typically results from a flexion–extension-type injury, may be the result of a spinal cord infarction due to temporary occlusion of either the vertebral arteries or the anterior spinal artery.18
Fortunately, magnetic resonance imaging (MRI) now allows better evaluation of the soft tissues of the spine. Thus, even when patients presenting with a spinal cord injury have no apparent osseous abnormality, MRI can delineate extradural lesions such as disc herniations and ligamentous injuries, as well as intradural lesions such as spinal cord hematomas and edema. Furthermore, these MRI findings have been determined to correlate well with the clinical presentation and are also of prognostic significance.17
Type III injuries are based solely on radiographic abnormalities, including fractures, fracture-dislocations, herniated discs, and ligamentous and soft tissue injuries. This class encompasses a vast range of injury severity and must also be evaluated on a case-by-case basis. An important aspect of each type III injury is determining the stability of the injury in order to assess the potential for return to play.5,16 Surgical stabilization alone does not mean that the athlete can return to play. The level and type of surgical repair, as well as the sport in question, must all be considered before a decision on safe return to play can be made.9,19
CERVICAL SPINE INJURIES
Spinal cord injury
Epidemiology
Acute spinal cord injuries are relatively infrequent, but are an inherent risk of collision and high-velocity sports. With an incidence of 4 per 100 000 population per year, approximately 10 000 new spinal cord injuries occur annually in the United States.16 Between 5% and 10% of these spinal cord injuries occur during athletic activity, both organized and recreational.11
Spinal cord injuries occur most frequently in tackle football (1.87 per 100 000 players per year) among organized sports and in diving among recreational activities.5 While severe spinal cord injuries in sports are usually rare accidents, other sports with documented spinal cord injuries, in addition to American football, include gymnastics, wrestling, ice hockey, rugby, snow skiing, snowboarding, surfing, and soccer among others.4,20,21
With a conscious focus on better understanding the pathomechanics of the injuries that lead to acute sports-related spinal cord injuries, particularly in organized sports such as football, various interventions have led to a decrease in the occurrence of spinal cord injuries over the past 30 years.5,21 Changes in rules, advances in protective equipment, and adjustments in proper playing techniques have all contributed to the decrease in the incidence of spinal cord injuries in organized sports. Because so many circumstances are variable and uncontrollable in recreational activities, it has been far more difficult to impact the frequency of spinal cord injuries in those situations.5,21
Pathomechanics
According to the National Center for Sports Injury and Research, almost all of the cases of sports-related cervical spinal cord injury resulted from cervical spine fractures/dislocations, unless spinal stenosis was present.22
The mechanism of permanent spinal cord injury is thought to be from a tremendous axial load to the vertex of a player’s head that is then absorbed in the cervical spine, which is overwhelmed. This load leads to a structural failure of the spinal column and a resulting spinal cord injury. The structural failure is more likely to occur when the neck is in slight forward flexion, negating the seemingly protective natural lordosis of the cervical spine, and establishing a more uniform column which absorbs the axial load rather than dissipating it.7,23
The primary neurological injury occurs at the time of the impact. The secondary neurological injury, involving a cascade of edema and hemorrhage, occurs after the primary injury and can be minimized with the proper immediate care of the injured athlete.5
Evaluation and management
An individual with a spinal cord injury may present with no movement, complaints of pain, particularly in the neck, or with complaints of sensory changes.11 When a spinal cord or other severe acute neurological injury is thought to have occurred, the ABCs (airway, breathing, circulation) of the standard trauma protocol must be initiated immediately. It is critical that every unconscious athlete be treated as though a spinal cord injury has occurred.15 While the ABCs are the highest priority, the downed athlete should have the cervical spine stabilized as soon as possible, as previously discussed, and prepared for transport to a medical facility for further evaluation and management.
Return to play
Due to the severe nature of spinal cord injuries, athletes who sustain a spinal cord injury have an absolute contraindication to return to contact or high-velocity sports.11
Spinal cord injury variant
Burning hand syndrome is a type of spinal cord injury. A variant of central cord syndrome thought to preferentially affect the spinothalamic tracts, burning hand syndrome is classified as a type II cervical spine injury. Athletes with burning hand syndrome present with a burning sensation in the bilateral hands and fingertips, often in the absence of neck pain or limitation. Weakness may or may not be noticed and occasionally the dysesthesias are noted in the lower extremities. If an athlete is suspected of having burning hand syndrome, he or she must be removed from competition, as with any spinal cord injury, until a full physical examination and radiographic evaluation determines the nature and extent of the injury. While there may be no detectable cervical spine abnormality, at least 50% of the cases of burning hand syndrome will have evidence of a fracture or soft tissue injury.7,24,25
Transient quadriparesis and cervical stenosis
Epidemiology
Transient quadriparesis is a relatively rare cervical spine injury that, by definition, is not permanent. Thought to be a temporary dysfunction of the spinal cord, transient quadriparesis has also been referred to in the literature variably as transient neurapraxia, cervical cord neurapraxia (CCN), and spinal cord concussion (SCC).26–28 Because the pathophysiology of this temporary phenomenon is not completely understood, the more descriptive terminology of transient quadriparesis is often used.
Transient quadriparesis occurs most frequently in American football, but has also been described in athletes injured in boxing, hockey, basketball, and wrestling. The incidence of this type of injury has been estimated to be 1.3 episodes of sensorimotor deficits per 10 000 athletes and 6 episodes per 10 000 athletes in sensory disturbance alone.29 Athletes with an episode of transient quadriparesis may report a sensory change, a functional motor change, or a combined sensorimotor syndrome. Transient quadriparesis is not permanent; however, the athlete may complain of sensory changes or demonstrate motor deficits anywhere from a few minutes to several days later, though usually it is less than 48 hours.11,27 The vast majority of cases resolve in 10–15 minutes.23
Transient quadriparesis may present as a sensory change, motor weakness, or complete paralysis and can affect the bilateral arms or legs, the ipsilateral arm and leg, or all four extremities. Episodes of transient quadriparesis can be classified into three grades, based on the time frame of symptoms. Grade I injuries last less than 15 minutes. Grade II episodes last anywhere from 15 minutes to 24 hours. Grade III injuries last greater than 24 hours, but less than 48 hours. The vast majority of cases are grade I quadriparesis.28,30
Pathomechanics
Transient quadriparesis is a result of contact, typically axial loading with the neck in either flexion or extension.23 When first described, transient quadriparesis was considered a ‘concussion’ of the cervical spinal cord.26,27 Though still not completely understood, several mechanisms have been proposed, including spinal cord edema or local ischemia. However, these two mechanisms do not correlate with the immediate onset and rapid resolution of the symptoms. A mechanism of transient quadriparesis that is often described is a functional disturbance of the axonal membrane without disruption of the structural integrity.26 Though the nerve itself is not disrupted, there may be prolongation of the absolute refractory period of the long-tract axons of the spinal cord. Ultimately, the prolonged refractory period may lead to a lengthened period of time in which the axons do not respond normally to subsequent stimulation.26,27
The term neurapraxia is often used to describe the proposed phenomenon that leads to transient quadriparesis27,28 because neurological symptoms occur, but the integrity of the long-tract axons of the spinal cord is thought to be preserved. However, the term neurapraxia is classically used to refer to peripheral nerve dysfunction.31 Thus, the distinction between involvement of a spinal cord axon and a peripheral nerve axon may have different implications. The term neurapraxia may misrepresent the pathophysiology of this central nervous system lesion compared with the more common neurapraxia of the peripheral nervous system.
The current understanding of the mechanism of transient quadriparesis is consistent with the ‘pincer mechanism’ as described by Penning.28,32 A combination of axial loading and hyperextension is thought to be the primary cause. With hyperextension, the spinal canal is maximally narrowed and the cord can be compressed between the posteroinferior aspect of the superior vertebral body and the anterosuperior aspect of the spinal laminar line of the subjacent vertebral body. The degree of compression is dependent on the sagittal diameter of the canal, the degree of extension, and the amount of infolding of the soft tissues such as the ligamentum flavum and posterior longitudinal ligament.27,32
Extreme flexion with axial loading is another potential cause of transient quadriparesis. With hyperflexion, the spinal canal is also significantly reduced, potentially resulting in compression of the spinal cord. The compression occurs because the distance is reduced between the spinal laminar line of the superior vertebral body and the posterosuperior aspect of the inferior vertebral body.27,30
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree