Acute Injuries: Shoulder Fractures and Acromioclavicular and Sternoclavicular Joint Injuries
Robert Talac MD, PHD
Joel J. Smith MD
The most common cause of a proximal humerus fracture is a fall on outstretched hands from a standing position. Another mechanism of injury is excessive rotation while the arm is abducted.
Although fracture of the proximal humerus significantly limits function of the upper extremity, careful neurovas cular examination of the entire upper extremity should always be performed. There are three important nerves— axillary, suprascapular and musculocutanneous—in close proximity of the proximal humerus and nerve injury accompanies the majority of humerus fractures.
The trauma series, consisting of anteroposterior (AP) view of the scapula, a lateral, Y-view of the scapula, and axillary view, is the standard initial method of evaluation for proximal humerus fracture.
More than 80% of the proximal humerus fractures are nondisplaced and can be treated nonoperatively. The shoulder is initially immobilized in a sling at the side or in Velpaeu position. After pain has diminished and the fracture is stable (usually after 7 to 10 days), gentle pendulum exercises can be started.
Some dislocated two-part surgical neck fractures can also be treated conservatively. They may require closed reduction in conscious sedation or general anesthesia.
Multipart proximal humerus fractures or isolated fractures of the greater or lesser tuberosities that are displaced more than 5 mm should be treated with open reduction and internal fixation. Surgical modalities include plates, screws, intramedullary devices and their combinations.
Clavicle fractures account for 35% of fractures about the shoulder.
Most patients with clavicle fracture report a direct fall onto the shoulder with subsequent pain and deformity in a clavicular region.
Most middle third clavicle fractures are treated conservatively with a sling or figure-eight dressing for 3 to 6 weeks.
Similarly to other shoulder injuries, patients with the acromioclavicular joint injuries often report a fall or direct trauma to the shoulder. Physical exam reveals swelling and tenderness over distal clavicle associated with a deformity caused by a horizontal and/or vertical displacement of the clavicle.
Initial radiographic confirmation and evaluation of the clavicle fracture and acromioclavicular joint injury should include AP and 45 degree cephalic tilt (apical oblique) views with patient upright which brings the clavicular image away from the thoracic cage.
The shoulder joint mobility plays a vital role in upper extremity function. It is therefore not surprising that optimal management of acute shoulder injuries remains an important issue that confronts the orthopedic profession. Modern management of shoulder injuries has become technically sophisticated. The purpose of this chapter is to provide a succinct review of current opinions and advancements in the management of proximal humerus and clavicle fractures as well as acromio- and sternoclavicular joint injuries.
Few areas of fracture management have been the subject of as much controversy, new information, and revisionist thinking as the management of proximal humerus fractures. Proximal humerus fractures account for 2% to 4% of all upper extremity fractures (1). They occur most often in older patients and represent complex injuries often including bony fragment displacement associated with varying degree of soft tissue injury.
Anatomy and Biomechanics
The humerus is the largest bone of upper extremity. The proximal humerus is composed of the humeral head, the greater and lesser tuberosities, the anatomic and surgical necks of the humerus. The humeral head is the most proximal, ball-like region of the humerus that is retroverted (28 to 40 degrees) and articulates with the glenoid cavity of the scapula. The head of the humerus is significantly larger than the glenoid fossa. There is no bony structural stability to the joint. The motion of the glenohumeral joint completely relies on the balance of tension and compression of soft tissues attached to the proximal humerus and the scapula. After a fracture occurs, the pull of shoulder muscles becomes the deforming force dictating the pattern of the fracture. In addition, understanding a relationship between bony fragment position, soft tissue balancing and glenohumeral joint function is essential for successful outcome after proximal humerus injury. The greater and lesser tuberosities are close to the humeral head and they are insertion sites for the rotator cuff. Both tuberosities are separated by the intertubecular groove in which lies the tendon of the long head of the biceps muscle and the arcuate artery, a branch of the anterior circumflex humeral artery. The intertubercular groove is covered by the transverse humeral ligament. The humeral head and tuberosities are separated by a narrow region which represents the anatomic neck of the humerus. Distal to anatomic neck proximal humerus narrows connecting to humeral shaft. This area is called surgical neck and represents most vulnerable part of the proximal humerus. This area also contains the main arterial supply to the proximal humerus, anterior and posterior circumflex arteries that arise from axillary artery. Both circumflex arteries make numerous extra-osseous collaterals that help to supply the most proximal areas of the proximal humerus. Despite the rich blood supply, avascular necrosis (AVN) of the humeral head is still a common sequelae of the proximal humerus fractures particularly if majority of the bony and soft tissue have been detached from the humeral head. The shoulder’s innervation is derived from brachial plexus. From a clinical perspective, there are three important nerves in close proximity of the proximal humerus: These include the axillary, suprascapular, and musculocutanneous nerve.
History and Physical Findings
The most common mechanism of injury for proximal humerus fracture is a fall on outstretched hands from standing. Another mechanism of injury is excessive rotation while the arm is abducted. In this situation, the proximal humerus locks against the acromion. Even minor force can cause a fracture, especially if the bone was previously weakened by osteoporosis. Inspection of the affected area often reveals significant swelling, tenderness on palpation, and obvious deformity of affected shoulder. Crepitus may be present upon motion of the fracture fragments. Although the fracture of the proximal humerus significantly limits function of the upper extremity, careful neurovascular examination of entire upper extremity should always be performed. Recently, Sommer et al. (2) reported the nerve injury in 67% of the patients with a proximal humerus fracture. The axillary nerve was involved in 58% and suprascapular nerve in 48%. All rings should be removed from the fingers. It is important to warn the patient about transient worsening of the swelling and possible development of ecchymosis within first 24 to 48 hours after injury. Although diagnosis of the fracture is made radiographically, the circumstances resulting in the injury should be elucidated and assessment for associated injuries of the neck, the clavicle, and sternoclavicular joint should be performed.
Radiographic Evaluation
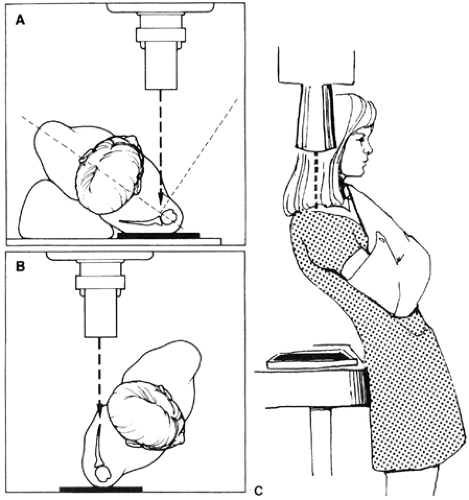
Accurate radiographic evaluation of the fracture of the proximal humerus is essential for diagnosis and treatment. The trauma series (Fig 17-1) is still the standard initial method for evaluating proximal humeral fracture. This consists of anteroposterior (AP) view of the scapula, a lateral, Y-view of the scapula, and axillary view. This series allows evaluation of the fracture pattern in three perpendicular planes. It is not uncommon for inadequate radiographs to be done. The two most common problems include the AP view of the scapula with the arm internally rotated, and not doing an axillary view. Without an axillary view, it is almost impossible to determine the relationship between the humeral head and the glenoid. To obtain a proper AP view of the scapula, the arm should be gently externally rotated about 20 degrees. This can be easily accomplished letting the patient hold onto IV pole or the edge of the table. A similar maneuver can be used to obtain abducted axillary view. Some surgeons prefer Velpau axillary view, in which arms stay in the sling, the patient leans back, and the beam is aimed down though the shoulder (1) (Fig 17-1).
The role of CT in the evaluation of proximal humerus fractures remains controversial. Some orthopedists order CT scan only if pattern of the fracture cannot be clearly determined. Others argue that standard radiographs are not sufficient to appreciate subtle changes in rotation and
positioning of the fragments and recommend CT scan as a part of standard radiographic evaluation of proximal humerus fractures. Moreover, CT images can be digitally manipulated to provide three-dimensional (3D) reconstruction of the fracture. Most recently, Edelson et al. (3) reported their experience with 3D-CT reconstruction of the proximal humerus fractures. They suggest that 3D-CT reconstruction provides precise information about anatomy of bony fragments that not only help to better understand fracture pattern, but may lead to improved or better surgical procedures. Magnetic resonance imaging (MRI) is rarely needed.
positioning of the fragments and recommend CT scan as a part of standard radiographic evaluation of proximal humerus fractures. Moreover, CT images can be digitally manipulated to provide three-dimensional (3D) reconstruction of the fracture. Most recently, Edelson et al. (3) reported their experience with 3D-CT reconstruction of the proximal humerus fractures. They suggest that 3D-CT reconstruction provides precise information about anatomy of bony fragments that not only help to better understand fracture pattern, but may lead to improved or better surgical procedures. Magnetic resonance imaging (MRI) is rarely needed.
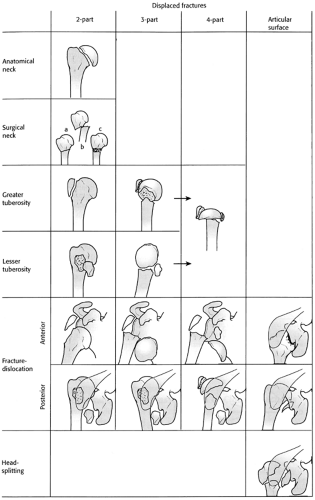
Decision Making Algorithms and Classification
Accurate analysis of radiographs and a reproducible classification system are desirable for the treatment of any fracture. Various classification systems have been proposed for the fractures of the proximal humerus in the past. Neer’s modification of Codman’s four fragments classification system (Fig 17-2) and AO/Orthopedic Trauma Association (OTA) system represent most commonly used schemes for classification of fractures of the proximal humerus. Both systems are based on the analysis of plain radiographs. In the Neer system, fractures are classified based on the number of segments and displacement of any of four principal fragments: humeral head, greater and lesser tuberosities, and humeral shaft. If fragments are displaced <1 cm from each other, or angulated <45 degrees, the fracture is considered minimally displaced or one part fracture. A two-part fracture contains two fragments, and most often the fracture line runs through the surgical neck separating the shaft from the head and both tuberosities. Three-part fractures involve either the lesser or greater tuberosity fracture in conjunction with a fracture of the surgical neck. Four-part fractures have all four key components displaced from each other. AO/OTA classification is more complex and is not widely used in the United States. There is growing recognition that existing classifications schemes are inadequate in terms of interobserver reliability as well as predicting the clinical outcome (4,5). Most recently, Edelson et al. (3) reported a 3D classification for fractures of the proximal humerus based on 3D-CT reconstructions. To address inherent difficulty with presenting a 3D object on a two-dimensional (2D) printed page, they devised a fracture wheel format in which each fracture is presented in simultaneous four-quadrant views. The injury is seen from the front, side, back, and from above in one composite picture. Using this technique, they organized proximal humerus fractures into four basic types: two part fractures; three part fractures; shield fractures with their variants; and isolated fractures of the greater tuberosity. Statistical analysis of interobserver reliability demonstrated approximately twofold improvement over previous classifications (kappa 0.69). They also suggest that the experience gained from the understanding the 3D patterns of fracture provide invaluable information guiding the restitution of anatomy during the surgery.
Many treatment methods have been described through the years. In general, the choice of the treatment for a proximal humerus fracture should be based on the type of the fracture, presence of concurrent injuries, age and activity level of the patient, the presence and nature of comorbid medical conditions, and potential outcomes of specific treatment strategy.
Over 80% of the proximal humerus fractures are non-displaced or minimally displaced and can be treated non-operatively (1,3,6). Initially, the shoulder is immobilized in a
sling at the side or in Velpaeu position. After pain is diminished and the fracture is stable (usually 7 to 10 days after injury), gentle pendulum exercises can be started. It is important to establish that the fracture is stable and moves as a unit prior to starting exercises. The exercises should be performed 3 to 4 times a day under supervision of the therapist, or at home after appropriate instruction by a physical therapist. The patient should be advised that overly aggressive exercise can lead to malunion or nonunion. Initial, immobilization and early motion have a high degree of success as documented by numerous studies (1,6).
sling at the side or in Velpaeu position. After pain is diminished and the fracture is stable (usually 7 to 10 days after injury), gentle pendulum exercises can be started. It is important to establish that the fracture is stable and moves as a unit prior to starting exercises. The exercises should be performed 3 to 4 times a day under supervision of the therapist, or at home after appropriate instruction by a physical therapist. The patient should be advised that overly aggressive exercise can lead to malunion or nonunion. Initial, immobilization and early motion have a high degree of success as documented by numerous studies (1,6).
Some dislocated two-part surgical neck fractures can also be treated conservatively. They may require closed reduction in conscious sedation or general anesthesia. In this type of injury, the shaft is usually displaced medially and anteriorly by the pull of the pectoralis major muscle, while the tuberosities remain in a neutral position. After adequate relaxation is achieved, it is possible to reduce the shaft and impact it under the head using gentle traction with flexion and adduction of the arm. Repeated and/or forceful closed reduction is not recommended. If a closed reduction is not possible, it is likely that there is an interposition of soft tissue, most commonly long head of the biceps, in the fracture site. Whenever possible, fluoroscopic C arm visualization should be employed. This allows not only visualizing the reduction, but also assessing the stability of the fracture. If the fracture is unstable, percutaneous pinning of the anterior and greater tuberosity with terminally threaded K-wires can be used to further stabilize the fracture. The greater tuberosity pins should be placed into the proximal humerus with the shoulder externally rotated and should engage the cortex at least 2 cm from most distal aspect of the humeral head. Be sure to pay close attention so that the humeral head is not penetrated (7).
Multipart proximal humerus fractures or isolated fractures of the greater or lesser tuberosities that are displaced more than 5 mm should be treated with open reduction and internal fixation. Many surgical modalities have been described in the literature. These include plates, screws, intramedullary devices, and various combinations. In general, it is important to avoid extensive exposure and soft tissue dissection because this may further compromise an already altered blood supply. As per recent literature, blade plate with interfragmentary screws or newly designed contoured proximal humerus locking compression plates seem to be most commonly used techniques for open treatment of proximal humerus fractures. The majority of orthopedists use one of the two basic surgical approaches to proximal humerus: superior deltoid approach or long deltopectoral approach. In an attempt to minimize surgical trauma to the soft tissue envelope, a new minimally invasive plating technique has been described (8). This plating technique preserves the soft tissue envelope and periosteum, maintains arterial vascularity and therefore minimizes the surgical trauma to the zone of injury. In addition, early biomechanic studies demonstrated that locking plates are less likely to fail in osteoporotic bone (9). These results are promising, but further studies are needed to demonstrate relative merit of these new techniques.
In cases of comminuted four-part fractures, humeral head splitting injuries, or humeral head defects >40% of the articular surface, open reduction and internal fixation yields unsatisfactory results (1,6,8). Due to the high incidence of AVN, post injury early humeral head hemiarthroplasty is favored. In addition, results of late arthroplasty are inferior to those treated acutely with humeral head replacement. The studies reviewing outcomes of hemiarthroplasty for proximal humerus fractures suggest that early surgical intervention within 2 weeks of injury and accurate tuberosity reconstruction are two factors that have the greatest impact on functional outcome (10).
Fracture of the proximal humerus presents a therapeutic challenge. Numerous complications have been reported. Most common complications include AVN, malunion, neurovascular injury, and adhesive capsulitis (frozen shoulder) (1,2,3,6,8,10). Hardware failure, infection, and nonunion are less common.
AVN is a common complication following three- and four-part fractures. The incidence of AVN of the humeral head ranges from 21% to 75% (1). Although the exact mechanism leading to necrosis is not known, it seems that disruption of the anterior humeral circumflex artery and its branches during the injury play a critical role in development of this complication. The treatment of choice for symptomatic AVN is a humeral head arthroplasty.
Malunion is a complication occurring after inadequately closed reduction or failed open treatment. The treatment is often challenging because of excessive scarring and retraction of the fragments. Angulation or rotational malunions are treated with osteotomy and internal fixation. If malunion is associated with AVN or post-traumatic degeneration, humeral head arthroplasty or total shoulder replacement may be considered.
Neurovascular injuries occur as an associated injury during proximal humerus fracture or as a complication of surgical treatment particularly percutaneous pinning. The main trunk of the axillary nerve and posterior humeral circumflex artery is at risk during placement of the greater tuberosity pins (7). The anterior branch of the axillary nerve can be damaged during placement of the proximal lateral pin, and musculocutaneous nerve, cephalic vein, and biceps tendon can be injured during the anterior pin placement (7).
Rehabilitation is an essential part of the therapeutic plan for a proximal humerus fracture. Early range of motion exercises help prevent adhesive capsulitis (frozen shoulder) that impede adequate motion necessary for optimal function. Initial management consists of an early, staged exercise program. Patients with a frozen shoulder unresponsive to
conservative treatment may be considered for arthroscopic debridement of glenohumeral joint and subacromional space and selective capsular release combined with manipulation under general anesthesia. Manipulation under general anesthesia as a stand-alone procedure has also been described and has demonstrated improvement in range of motion (11,12). Although manipulation under anesthesia was effective in terms of joint mobilization, the method can cause iatrogenic intra-articular damage such as iatrogenic superior labrum anterior-posterior lesions, partial tears of the subscapularis tendon, anterior labral detachments with a small osteochondral defect, or tears of the middle glenohumeral ligament (12).
conservative treatment may be considered for arthroscopic debridement of glenohumeral joint and subacromional space and selective capsular release combined with manipulation under general anesthesia. Manipulation under general anesthesia as a stand-alone procedure has also been described and has demonstrated improvement in range of motion (11,12). Although manipulation under anesthesia was effective in terms of joint mobilization, the method can cause iatrogenic intra-articular damage such as iatrogenic superior labrum anterior-posterior lesions, partial tears of the subscapularis tendon, anterior labral detachments with a small osteochondral defect, or tears of the middle glenohumeral ligament (12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree