Acromioclavicular Joint: Difficult Problems and Revision Surgery
Young W. Kwon
Joseph P. Iannotti
Y. W. Kwon: Assistant Professor, Department of Orthopedic Surgery, NYU-Hospital for Joint Disease, New York, New York.
J. P. Iannotti: Professor and Chairman, Department of Orthopedic Surgery, The Cleveland Clinic Foundation, Cleveland, Ohio.
INTRODUCTION
The acromioclavicular (AC) joint is one of the most commonly injured structures in the human body. Because of its subcutaneous location, the AC joint is highly susceptible to injury after direct trauma to the shoulder girdle. In addition, because of the repetitive nature of shoulder motion and the large amount of force that must transmit across a relatively small surface area, this structure is also prone to various degenerative conditions. The majority of AC joint pathology can be successfully treated without a surgical intervention. If, however, a surgical intervention is warranted, there are numerous procedures, both historic and contemporary, that can be used to treat pathologic conditions about the AC joint.
For patients with a difficult problem or condition that requires a revision surgery, understanding the nuances of a single pathology or a single procedure is of limited benefit. Rather, identifying the underlying pathology and restoring the physiologic biomechanical properties of the joint will be of greater value in successfully treating these patients. As such, instead of providing a detailed description of any single procedure, this chapter will focus on providing a general guideline in evaluating and treating patients with a complex AC joint pathology.
ANATOMY AND BIOMECHANICS
The AC joint is located between the lateral end of the clavicle and the medial aspect of the anterior acromion. Its articular surface is initially composed of hyaline cartilage, which subsequently changes to fibrocartilage during early adulthood.88 The joint space is filled with fibrocartilaginous disks. These disks may be complete or meniscoid (i.e., partial). Overall size and dimensions of the meniscus can be quite variable.30 Similar to the knee, this meniscus is generally believed to possess both a stabilizing and a protective role for the joint. However, for unknown reasons, the meniscus degenerates rapidly during early adulthood to become a nondistinct structure by the fourth decade.30,70,73 As such, its exact role remains largely speculative.
Stability of the AC joint is provided by both dynamic and static restraints. Dynamic stabilization arises from
various superficial muscles about the shoulder girdle. For example, the anterior deltoid muscle originates in part from the lateral end of the clavicle and inserts onto the deltoid tuberosity on the humerus. Thus, during its contraction, the generated force will tend to depress the clavicle against the acromion and provide a stabilizing effect on the AC joint. Similar stabilizing force is also generated from contractions of the middle deltoid and trapezius muscles.
various superficial muscles about the shoulder girdle. For example, the anterior deltoid muscle originates in part from the lateral end of the clavicle and inserts onto the deltoid tuberosity on the humerus. Thus, during its contraction, the generated force will tend to depress the clavicle against the acromion and provide a stabilizing effect on the AC joint. Similar stabilizing force is also generated from contractions of the middle deltoid and trapezius muscles.
Static stabilizers of the joint include the AC ligaments and coracoclavicular ligaments. The AC ligaments are confluent thickenings within the joint capsule and are named according to their location. These ligaments are thought to be the primary stabilizers along the anterior-posterior direction.29,36,50 As such, significant amounts of translation may be observed in the anteroposterior direction even after isolated damage to the AC ligaments.29 For small displacements, these ligaments can also provide significant stability in the superoinferior direction. For larger displacements in the superoinferior direction, however, the majority of the stability is provided by the coracoclavicular ligaments.36 The coracoclavicular ligaments are composed of two primary structures. They are the conoid (medial) and trapezoid (lateral) ligaments, named after their approximate geometric shape. These ligaments arise from the coracoid process and attach onto the undersurface of the distal clavicle just medial to the joint. They span the coracoclavicular distance of approximately 13 mm.11,18 Although the AC and coracoclavicular ligaments each possess a role as a primary stabilizer along a particular direction, in the absence of one, the other can compensate to act as the primary stabilizer for all directions.36
Both the scapulothoracic and the glenohumeral motion contribute to the overall movement of the upper extremity. Relative contributions of each can vary depending on the total arc of arm motion.59 Primary motion of the clavicle during arm elevation is rotation around its long axis. Although overall rotation may reach up to 45 degrees, the majority of this motion appears to take place at the sternoclavicular joint rather than at the AC joint.45 Physiologically, the clavicle and scapula move as a single unit. As such, rotation at the AC joint is typically limited to only 5 to 8 degrees.26 Thus, full range of arm motion should be possible with minimal to no motion across the AC joint.25,48,72
PATHOLOGY
Acute Injuries of the Acromioclavicular Joint
Most acute injuries to the AC joint occur as a result of direct trauma. Because of the intrinsic stability of the sternoclavicular joint, most of the energy generated by an impact appears to be absorbed by the AC joint.12 A common cause of AC joint injury is a fall onto the shoulder with the arm in an adducted position, because this force will displace the acromion inferiorly. In addition, because of its subcutaneous location, the AC joint is often a primary target of an external blow. As expected, the magnitude and location of the impact will determine the severity of the injury. Initially, the resulting force is absorbed by the AC ligaments. With additional force, the AC ligaments rupture and the coracoclavicular ligaments are damaged. If the force is severe enough, the deltotrapezial fascia and the coracoclavicular ligaments can also be ruptured. In such cases, the upper extremity will have lost its suspensory support from the clavicle and therefore sag inferiorly relative to the clavicle.
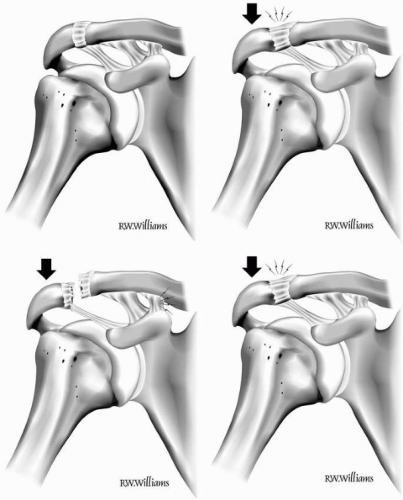
This sequence of injury progression has been summarized in an AC joint dislocation classification system. Originally proposed by Allman and Tossy et al., and subsequently modified by Rockwood et al., this system categorizes the severity of the injury on the basis of the damaged anatomic stabilizers and degree of overall joint displacement.4,72,86 Type I injury describes a sprain of the AC ligaments with other intact stabilizers. Type II injury describes a rupture of the AC ligaments with a sprain of the coracoclavicular ligaments and intact deltotrapezial fascia. Type III injury signifies a rupture of both the AC and the coracoclavicular ligaments with an additional injury to the deltotrapezial fascia. As such, there is a complete dislocation of the AC joint with an inferior displacement of the acromion relative to the clavicle. In types IV, V, and VI injuries, all of the stabilizing structures about the AC joint are disrupted and there is a gross dislocation of the joint. Type IV injury is associated with a severe posterior displacement of the clavicle, often piercing into or through the trapezius muscle. In type V injury, there is a gross (i.e., more than 100% compared with the normal shoulder) inferior displacement of the acromion relative to the clavicle. In type VI injury, the clavicle is actually displaced inferiorly relative to the acromion and often locked under coracoid process. The overall classification system is summarized in Figure 20-1.
Degenerative Conditions of the Acromioclavicular Joint
Because of its small dimensions, the relative amount of force transmitted across the AC joint is quite large. As the intra-articular meniscus tends to become nondistinct by the fourth decade of life, its ability to provide protection for the articular surface is limited.30,70,73 Thus, the AC joint is quite susceptible to degenerative changes. Systemic inflammatory diseases (e.g., rheumatoid arthritis, gout, or pseudogout), trauma, and previous operative procedures can also increase the likelihood of symptomatic AC joint degeneration. Although the true incidence of AC joint arthritis is unknown, it is generally believed to be the most common cause of AC joint pain.43 According to
one study, radiographic evidence of AC joint arthritis can be found in up to 57% of elderly patients, with 42% to 45% of these patients having associated joint tenderness.44 In addition, up to 70% of patients with documented arthritis in other joints may also have tenderness in one or both AC joints.92
one study, radiographic evidence of AC joint arthritis can be found in up to 57% of elderly patients, with 42% to 45% of these patients having associated joint tenderness.44 In addition, up to 70% of patients with documented arthritis in other joints may also have tenderness in one or both AC joints.92
It is important to distinguish radiographic evidence of arthritis from the clinical symptomatic entity, because many patients with significant radiographic AC joint changes may be asymptomatic.63,77 In one study, for example, up to 93% of patients with no shoulder symptoms had magnetic resonance imaging (MRI) findings consistent
with AC joint osteoarthritis.77 In addition, other pathologic changes about the shoulder girdle may coexist with symptomatic AC joint arthritis. In one series of patients, for example, more than 97% of patients with symptomatic AC joint degeneration had other coexisting shoulder pathology.24
with AC joint osteoarthritis.77 In addition, other pathologic changes about the shoulder girdle may coexist with symptomatic AC joint arthritis. In one series of patients, for example, more than 97% of patients with symptomatic AC joint degeneration had other coexisting shoulder pathology.24
An infrequent, but increasingly recognized, degenerative clinical entity of the AC joint is distal clavicle osteolysis. This condition is believed to be increasing in frequency because of the increasing emphasis by professional and recreational athletes on weight training. Histologic features of the condition include subchondral cysts, demineralization, and microscopic fractures.62 These observations have led to the hypothesis that distal clavicle osteolysis is a result of repetitive microtrauma to the AC joint leading to fatigue failure and bone resorption.23,24,62
EVALUATION—GENERAL GUIDELINES
Clinical Evaluation
Acromioclavicular joint symptoms may present as an isolated pathology or in conjunction with other conditions about the shoulder girdle. Therefore, a thorough history and examination are necessary to identify the exact cause(s) of symptoms. For acute injuries, the history may be clear and simple to elucidate. For chronic cases or degenerative conditions, the history may be more subtle. In these patients, the duration and nature of the symptoms should be addressed. Notable activities that can initiate or exacerbate the symptoms as well as any recent change in the level or type of activities should be elicited. Prior trauma and prior treatments, including surgical interventions, should also be discussed, and the appropriate documents must be reviewed.
A careful evaluation of the cervical spine should accompany the physical examination, because radicular symptoms may mimic vague AC joint pathology.38 Inspection may demonstrate prominence, and palpation may elicit crepitus or tenderness. Reproduction of the patient’s usual symptoms with AC joint palpation is the most important finding on physical examination. Isolated pathology of the AC joint should not typically inhibit shoulder motion. Therefore, a restricted motion in a setting other than recent trauma may suggest other pathology about the shoulder girdle. Provocative maneuvers such as cross-body adduction with the arm elevated at 90 degrees or internal rotation of the arm reaching to the lumbar spine may elicit significant pain in the AC joint. The specificity of these maneuvers for AC joint pathology has not been validated in the literature. Thus, positive findings on these maneuvers suggest, but do not confirm AC joint pathology. Instability of the AC joint is difficult to elicit. Manual manipulation can be performed to translate the distal clavicle away from the acromion. A positive finding would reproduce the abnormal translation, in either superoinferior or anteroposterior direction, with characteristic pain. Unfortunately, correlation of this maneuver to the actual pathology has not been validated in the literature.
For patients with an unclear source of pathology, a diagnostic injection with a short-acting anesthetic agent can be very useful. Elimination of symptoms with an accurately placed injection can confirm the source of pain.15,34 In addition to its diagnostic utility, an injection can also provide information regarding the potential benefit of a surgical intervention. For example, in patients with a degenerative joint, pain relief after an injection is typically considered to be the best prognostic factor for success after a distal clavicle excision.99 For an injection to be informative, however, a patient must be able to consistently reproduce the symptoms. Furthermore, the injection must be placed accurately within the joint. According to a cadaveric study, AC joint injection by an orthopedic surgeon was successful in only 67% of the cases.68 Inaccurate placement of the anesthetic agent into the subacromial space can actually lead to a false-positive diagnosis.
Radiographic Studies
Routine radiographs of the shoulder are inadequate for the examination of the AC joint. Because of its small size, these radiographs will typically “overpenetrate” the AC joint and fail to reveal any details. For most patients, approximately 50% of the voltage used for shoulder radiographs should be used when examining the AC joint. In addition, routine shoulder radiographs show an overlap of the AC joint against the scapula, which can prohibit detailed examination of the joint. For an acceptable evaluation, approximately 10 to 15 degrees of cephalic tilt should be used to project the x-ray beam.100 This tilt will allow isolated visualization of the AC joint without a bony background. To evaluate subtle changes, a similar tilt can be used to project an x-ray beam across both AC joints onto a single wide cassette.72 This view can allow comparison of the affected joint against the contralateral AC joint. In addition to these anteroposterior views, a lateral view of the AC joint should also be obtained and evaluated.91
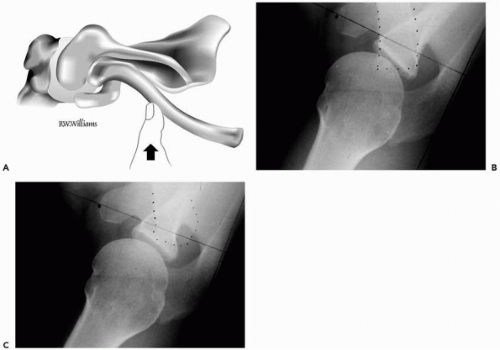
Stress views of the AC joint can be helpful for a certain population of patients whose history and examination suggest instability. Routine use of stress views, however, is not recommended.17 For examination of instability in the superior inferior direction, an anteroposterior radiograph with a cephalic tilted beam is obtained with approximately 10 to 15 pounds of weight that is either held by or tied to the wrist of the patient.78 When examining instability in the anteroposterior direction, an axillary lateral view can be obtained with either a posteriorly directed force to the
clavicle or an anteriorly directed force on the acromion.16 This view is illustrated in Figure 20-2. An alternative is a scapula lateral view with the patient voluntarily protracting the affected shoulder forward, as this maneuver may displace the scapula anteriorly relative to the clavicle.1,2,98 Typically, stress views are also obtained on the contralateral shoulder for comparison.
clavicle or an anteriorly directed force on the acromion.16 This view is illustrated in Figure 20-2. An alternative is a scapula lateral view with the patient voluntarily protracting the affected shoulder forward, as this maneuver may displace the scapula anteriorly relative to the clavicle.1,2,98 Typically, stress views are also obtained on the contralateral shoulder for comparison.
Other Studies
Routine use of other modalities for the evaluation of the AC joint is usually not necessary. In certain select cases, however, other studies can provide significant additional information. Computed tomography images can reveal a more detailed anatomy of the joint and exhibit subtle changes in the bony architecture. MRI can provide information regarding the soft tissues about the joint. Interpretation of the MRI should be performed with caution, however, because 75% to 93% of asymptomatic patients can exhibit signal changes consistent with arthritis.63,77 For symptomatic patients whose radiographs are unremarkable, a technetium bone scan can reveal changes in the AC joint.23 This can be especially useful in cases where distal clavicle osteolysis is suspected in its early phase but the radiographs are inconclusive. Finally, various authors have shown the utility of ultrasonography in the evaluation of AC joint instability.23,74,79 The dynamic nature of this study provides a unique perspective in assessing instability. However, because of its inherent limitations, such as user dependency, a routine use of ultrasonography to assess the AC joint has not gained wide popularity.
CONTROVERSIAL ACROMIOCLAVICULAR JOINT TREATMENT ISSUES
Surgical Versus Nonsurgical Treatment for Acute Dislocations
A general consensus seems to exist among orthopedic surgeons in treating acute type I and II AC joint dislocations. Typically, nonsurgical treatment is favored for acute cases, while surgical intervention is reserved for chronic, symptomatic patients.4,28,72,90 General consensus also exists for the treatment of acute AC joint dislocation types
IV, V, and VI. For these patients, elective surgical treatments are typically recommended.28,37,42,65,69,72 Open reduction and stabilization of the joint, with the repair of deltotrapezial fascia as needed, are associated with an improved clinical outcome for such cases.
IV, V, and VI. For these patients, elective surgical treatments are typically recommended.28,37,42,65,69,72 Open reduction and stabilization of the joint, with the repair of deltotrapezial fascia as needed, are associated with an improved clinical outcome for such cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree