Acquired Shoulder Stiffness: Posttraumatic and Postsurgical
Thomas F. Holovacs
Jon J. P. Warner
T. F. Holovacs: The Harvard Shoulder Service, Massachusetts General Hospital, Boston, Massachusetts.
J. J. P. Warner: The Harvard Shoulder Service, Massachusetts General Hospital, Boston, Massachusetts.
WHAT IS THE PROBLEM?
Definition and Classification
In contrast to primary adhesive capsulitis, acquired shoulder stiffness is a condition in which limitation of active and passive range of motion occurs after a well-defined traumatic event or a surgical procedure, and it is often associated with prolonged immobilization of the shoulder.30,34,37,51,52,59,70,80,87,91,97 It can follow a number of posttraumatic and postsurgical scenarios. These include trauma with or without fracture and distortion of the articular surfaces and tuberosities, stiffness occurring after anatomical instability procedures (i.e., Bankart procedure and capsular shift), stiffness after rotator cuff repair, stiffness after nonanatomic instability shoulder stabilization procedures (i.e., Bristow, Putti-Platt, Magnuson-Stack), and stiffness after any shoulder procedure, open or arthroscopic.
Approach to management of acquired shoulder stiffness requires an appreciation of the pathology and likely natural history in each clinical scenario. Although treatment of idiopathic adhesive capsulitis is usually conservative, many experts agree that nonsurgical approaches to acquired shoulder stiffness are not only less likely to be successful, but they may also result in eventual arthrosis in some cases.
Normal and Abnormal Anatomy/Mechanics of the Shoulder
The glenohumeral joint is inherently lax to allow for the wide range of multiplanar motion necessary for work, daily living, and sports participation. The glenohumeral ligaments act largely as passive restraints to excessive ranges of rotation and translation. So the relative capsular laxity in the midranges of motion is a feature of normal shoulder motion. In fact, joint compression created by muscle contraction is the major stabilizing force through much of the midrange rotations for the glenohumeral joint.
Although many cases of acquired shoulder stiffness result from global capsular contracture, scarring or shortening of specific regions of the capsule has been shown to lead to specific patterns of motion limitation.26,33,43,85 When the shoulder is in an adducted position, the rotator interval, which is composed of the coracohumeral and superior glenohumeral ligaments, becomes involved and typically limits flexion, extension, and external rotation. The anteroinferior capsuloligamentous complex is a restraint for external rotation in abduction, whereas the posteroinferior capsule limits internal rotation and forward flexion. These patterns are important to recognize when considering the regions of the capsule that may require surgical release to recover motion.
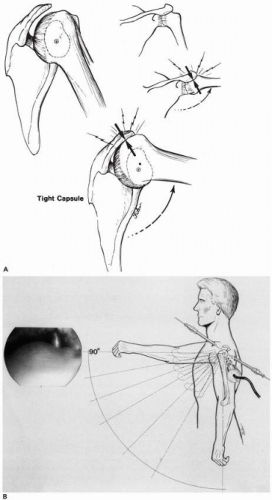
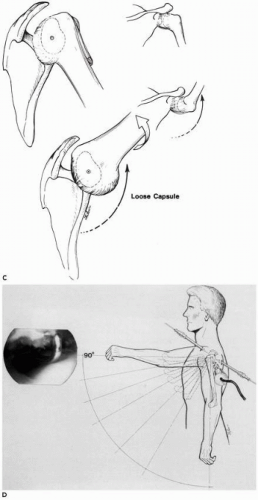
Of great clinical relevance are experimental observations,32,34 when the shoulder is rotated, of soft-tissue contractures that cause increased translation of the humeral head on the glenoid socket in a direction opposite to the location of the capsular contracture. For example, a Putti-Platt procedure shortens the anterior soft-tissues and causes the humeral head to translate posteriorly when external rotation is attempted. The consequence of this can be an increased joint-reactive load on the posterior glenoid and eventual development of articular erosion and arthritis.4,32,34 This has been termed capsulorrhaphy arthropathy32 (Fig. 11-1).
Anterior or posterior capsular contractures can also cause increased superior humeral head translation when a patient attempts to bring the shoulder into forward flexion32,82 (Fig. 11-2). These altered mechanics compress the rotator cuff against the acromial surface as the humeral head is pushed superiorly by the contracture. This has been termed “nonoutlet”-type impingement, and it explains why many patients feel impingement-like symptoms when they have a stiff shoulder.31,32,90 Arthroscopic release89 and experimental capsular sectioning33 have been shown to restore normal glenohumeral kinematics (Fig. 11-2).
Scapulothoracic pain can also be a confounding initial presentation in these patients. Because the shoulder complex is an intercalated series of joints, loss of glenohumeral motion usually causes a compensatory increase in scapulothoracic motion. Many patients present with secondary scapular winging, and some will complain of pain in the periscapular region.87
Finally, in osteoarthritis, global thickening and scarring are typical features of the joint capsule and may be the consequence of dysfunctional synoviocytes.75 Moreover, it is our opinion that, in long-standing cases of motion loss, there may be adaptations in the muscle architecture of the rotator cuff through fatty replacement and fibrous infiltration that reduce muscle compliance and further add to motion loss.
Pathogenesis
Acquired Capsular Contracture/Shortening
Idiopathic adhesive capsulitis is characterized by inflammation and subsequent scarring of the joint capsule, as well as by decreases in intra-articular volume and capsular compliance limiting motion in all planes.87 Inflammation of the joint capsule and subsequent scarring may also occur as an acquired entity, that is, after trauma or surgery. It is not clear whether the cause of posttraumatic or postsurgical capsulitis is different from that of idiopathic adhesive capsulitis or whether some patients simply develop adhesive capsulitis in the context of trauma or surgery. Age, length of immobilization, and endocrine, neurologic and psychologic disorders, all recognized as important in the pathogenesis of idiopathic adhesive capsulitis, also seem to play a role in the development of shoulder stiffness after trauma or surgical treatment.35
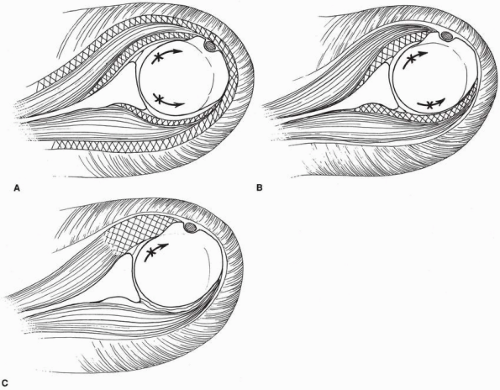
Three different basic forms of acquired shoulder stiffness can be defined (Fig. 11-3):
Capsular contracture (posttraumatic or postsurgical): stiffness after arthroscopic capsular shift, open Bankart repair, or open rotator cuff repair.
Extra-articular adhesions between tissue planes: stiffness after Bristow, Putti-Platt, or Magnuson-Stack procedures.
Skeletal or articular incongruity: proximal humeral malunion with displaced tuberosities,or stiffness associated with posttraumatic arthritis.
Although features of these three general categories can overlap in the same patient, this classification system is useful for developing a logical therapeutic approach.
Some specific examples include:
Calcific tendinitis: Stiffness after surgical excision of calcific tendinitis of the rotator cuff reportedly affects 6-20% of patients. The pathologic mechanism is unknown but the clinical symptoms are similar to those of adhesive capsulitis.54 In many cases, a conservative approach similar to that utilized for idiopathic frozen shoulder is successful.
Post-thermal capsulorrhaphy: Reports on thermal capsulorrhaphy suggest that stiffness is a common complication of this procedure.22 Patients who have undergone this procedure often present with the same symptoms as patients with idiopathic adhesive capsulitis, although the etiology is different. This procedure creates thermal injury to capsular tissue through an internal burn, which then results in a degree of inflammation; scarring also occurs as an obligatory repair mechanism. Why some patients develop this complication and others do not is unclear. Miniaci58 has proposed that it is related to transient axillary nerve neuritis in some way.
Post-rotator cuff repair: A recent meta-analysis91 of greater than 500 surgical cases reported in literature concluded a 4% incidence of measurable symptomatic loss of motion in patients undergoing rotator cuff surgery; however, it seems that this underreports the actual incidence of this complication. Even so, the need for surgical management of stiffness after rotator cuff repair seems to be rare.
Stiffness after anatomical instability repair: There is no documented reported incidence of stiffness after capsular shift repair or arthroscopic or open Bankart repair for traumatic or atraumatic shoulder instability. Several articles have postulated that these patients were analyzed as a cohort of all patients presenting with refractory stiffness17; however, virtually none of these series inferred anything but extremely rare incidences of symptomatic loss of motion after instability surgery. This most certainly represents underreporting, because many individuals may note loss of rotation after instability surgery but
may either not be symptomatic initially or only become symptomatic if postsurgical capsulorrhaphy arthropathy eventually recurs.
Stiffness after nonanatomical instability repairs: Stiffness may occur from extra-articular procedures that shorten tendons around the shoulder or asymmetrically shorten the anterior capsule. For example, a Putti-Platt procedure shortens both the anterior capsule and the subscapularis. A Magnuson-Stack procedure reduces external rotation by attaching the subscapularis insertion lateral to the bicipital groove with the arm in external rotation, which is the procedure’s aim. A Bristow or Latarjet procedure can shorten the subscapularis, especially if there is prolonged immobilization, because the subscapularis is scarred to the transferred conjoined tendon and coracoid process. All of these procedures can result in asymmetric motion loss, which has been shown to place the glenohumeral joint at risk for early osteoarthritis. Furthermore, loss of external rotation can actually coexist with untreated instability because inferior capsular laxity may remain untreated with these operations. This creates the paradoxical situation of a patient who complains of loss of motion but still has a sense of apprehension about instability episodes.
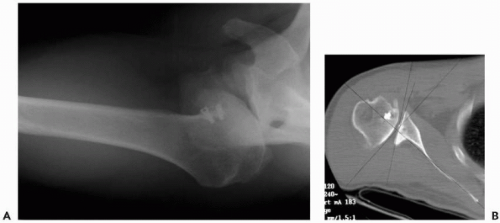
Extra-articular adhesions between tissue planes (scarring of gliding surfaces): Another requirement for normal shoulder mobility is free gliding between tissue planes. In the normal shoulder, the rotator cuff glides underneath the coracoacromial arch and the deltoid muscle. Trauma and prolonged immobilization or surgical procedures can lead to scarring between the deltoid and the proximal humerus, the rotator cuff and the acromion, and the rotator cuff and the joint capsule. Furthermore, prominent implants used to stabilize proximal humeral fractures may lead to scarring of the subdeltoid bursa (Fig. 11-4).
Skeletal or articular incongruity: Smooth, normally shaped articular surfaces, properly oriented to each other, represent the osteoarticular requirement for normal glenohumeral range of motion. Skeletal deformity is always associated with soft-tissue scarring.
Displaced fractures of the proximal humerus treated conservatively or in which anatomic reduction could not be achieved or maintained can be associated with stiffness resulting from not only soft-tissue contracture but also skeletal deformity. Intra-articular fractures with loss of the normal relationship between the humeral head and tuberosities are usually associated with poor function, partly because of stiffness but also because of malpositioning of the tuberosity. Extra-articular deformities are usually better tolerated.
Stiffness resulting from articular incongruity (and capsular contracture) is one of the leading features of osteoarthritis. Except for selected cases in the early stage of the degenerative process in which only the soft-tissue contracture needs to be addressed, correction of the articular deformity, through corrective osteotomy or replacement arthroplasty, is required in the majority of the cases. In the case of replacement arthroplasty, stiffness can be the result of nonanatomic reconstruction, such as oversizing and improper orientation of the components, and tuberosity-related problems, such as nonunion or malunion.
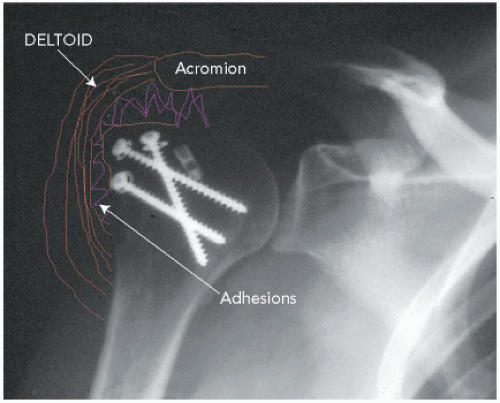 Figure 11-4 Adhesions between deltoid and rotator cuff after fracture repair and prolonged immobilization in a sling. |
The muscular imbalance seen in patients with brachial plexus birth palsy has been shown to lead to an age-related articular deformity if the condition is not addressed early. Once humeral head flattening and glenoid dysplasia have developed, soft-tissue release alone, either arthroscopically or as an open procedure, cannot increase mobility.93
Bony block procedures to treat instability, such as the Bristow, Latarjet, and Trillat procedures, are techniques that distort the skeletal and soft-tissue anatomy. Subscapularis entrapment or impingement and articular incongruity may lead to limitation of motion after these procedures.91
Clinical Evaluation
An accurate history and physical examination are prerequisites to proper treatment of the refractory stiff shoulder. Patients with adhesive capsulitis frequently report no inciting traumatic event whatsoever. These patients describe the insidious and unremitting onset of shoulder pain, which predates stiffness and is unresponsive to physical therapy. Acquired shoulder stiffness, on the other hand, occurs as a result of a well-defined event, such as prolonged immobilization following trauma and anatomic (capsular shift) or nonanatomic (Putti-Platt) surgical overtightening for glenohumeral instability.34,70,82,87 Prior surgery or trauma must be clarified. For example, if a patient had a fracture and then developed stiffness after prolonged immobilization, this might indicate that there are adhesions between
tissue planes as well as a capsular contracture. Radiographic imaging would then determine whether there is bony incongruity around the joint.
tissue planes as well as a capsular contracture. Radiographic imaging would then determine whether there is bony incongruity around the joint.
Medical conditions, such as diabetes, must also be considered.66,87 Patients who develop a stiff shoulder without trauma or even after trauma or surgery may have this as a confounding variable. Finally, a patient who develops a stiff shoulder after rotator cuff surgery may also have a rerupture of the rotator cuff, which may affect decision making because both stiffness and rotator cuff insufficiency must be addressed.
Symptoms
As described in the preceding text, symptoms may vary among patients. Some patients complain not only of motion loss but also of impingement-type pain with pain radiating into the deltoid area. The mechanism, as described previously, is one of nonoutlet impingement. Others may also have periscapular pain due to transfer overload onto the scapulothoracic articulation as a compensation for glenohumeral motion loss. Still others with very severe motion loss may have minimal complaints of pain and be willing to tolerate their motion loss. These individuals are particularly challenging because, if the severe loss of external rotation is left untreated, they may be the most at risk for eventual capsulorrhaphy arthropathy. Indeed, this is one of the few groups of patients in whom we often advise surgical contracture release prior to developing symptoms of pain. If the patient waits many years for pain to develop, irreversible articular damage will have already occurred due to the mechanical overload of the posterior joint (Fig. 11-1).
Physical Examination
Begin the physical examination of the shoulder by inspecting the ipsilateral and contralateral shoulders for signs of prior trauma/surgery, atrophy, and deformity. The patient should always be examined while viewing the exposed shoulder and torso from the front and back. Active motion of the shoulder girdle is assessed using a goniometer with the patient seated. Document active flexion, elevation in the scapular plane, and abduction, as well as internal/external rotation, both at the side and in abduction. Assess passive mobility in the same planes of motion, first with the patient seated and, then, supine (to stabilize the scapula and minimize scapulothoracic substitution). It should be noted that scapulothoracic substitution might give the appearance of good shoulder motion when glenohumeral motion is actually quite restricted. Patients with shoulder stiffness have active and passive motion loss that is equal. If there is active motion loss but passive motion is preserved, one should think of rotator cuff insufficiency. Weakness associated with passive motion loss may also indicate a rotator cuff tear or nerve injury.
Patterns of motion loss are very important to recognize. Primary adhesive capsulitis tends to present with global motion restriction, whereas postsurgical or posttraumatic stiffness may present with a more discrete or isolated motion loss.26,87 For example, a patient may have good flexion but marked loss of external rotation after a Putti-Platt or Bristow procedure, which has selectively shortened the anterior capsule and subscapularis. Another example, diminished external rotation in adduction, indicates contracture of the anterosuperior capsule and the rotator interval, while limited external rotation in abduction is associated with scarring in the anteroinferior capsule. Furthermore, limitation of internal rotation in either adduction or abduction may be associated with posterior capsular scarring. These preoperative observations are important because they indicate which portions of the capsule may need to be addressed, if a surgical release is required.
In addition to passive limitation of motion, many patients will complain of symptoms that suggest rotator cuff impingement. Although these patients may have pain with flexion, the impingement symptoms that seem to suggest rotator cuff disease are actually secondary due to alterations in joint mechanics as a result of the capsular contracture. This is “nonoutlet” impingement, which occurs without altering the architecture of the coracoacromial arch and, instead, is due to a tight capsule that pushes the humeral head in a superior direction when flexion is attempted31,32,90 (Fig. 11-2). Periscapular pain may also develop due to the scapulothoracic muscles stretching to compensate for the limited glenohumeral joint motion.
Imaging Studies
Plain radiographs are always essential to rule out arthrosis, associated fracture malunion, and loose or misplaced metal implants and hardware.
Arthrography has been advocated by many to confirm a decreased joint capacity.66 However, it has been shown that there is no direct correlation between arthrographic findings and motion loss.40 Therefore, its use is often limited to an adjunctive role, such as ruling out a concomitant rotator cuff tear.
Magnetic resonance imaging (MRI) and contrast-enhanced computed tomography (CT) are limited in use, aiding in the diagnosis of additional shoulder pathology, such as locating a rotator cuff tear or the exact position of hardware that may be impinging on the articular surface.
Acquired Capsular Contracture/Shortening
Acquired capsulitis means the development of shoulder stiffness after a traumatic incident, surgical treatment without tissue or bone repair, i.e., decompressing calcifying tendinitis, or after arthroscopic or open surgery. Examples of this last category might include arthroscopic thermal
capsulorrhaphy, Bankart and capsular shift procedures, Bristow procedure, Putti-Platt procedure, rotator cuff repair, and other shoulder reconstructions.
capsulorrhaphy, Bankart and capsular shift procedures, Bristow procedure, Putti-Platt procedure, rotator cuff repair, and other shoulder reconstructions.
After trauma or surgery of the shoulder, some patients develop severe pain that cannot be explained by the underlying condition. This type of shoulder stiffness seems similar to the idiopathic form of the disease. Some patients may have the diabetes risk factor. The symptoms usually do not occur immediately after trauma or surgery, but 2 to 6 weeks. The patient’s pain is constant and is especially severe at night. Attempts at regaining motion rapidly with physical therapy may lead to exacerbating the chronic discomfort. Regular pain medication prescribed after the traumatic event or operation, or subacromial infiltration with a local anesthetic, does not help to control the pain. On physical examination, any manipulation of the shoulder is extremely painful to the patient. At this stage, loss of passive range of motion may be discrete, but passive rotation amplitude, especially in abduction, is already decreased and is very painful. Active range of motion is limited by pain as well as by soft-tissue shortening.
Acquired capsular contracture, with or without concomitant scarring between tissue planes, is usually seen after fractures or surgery. The prolonged immobilization often required for healing injured or repaired structures plays an important role in developing this type of stiffness. Scarring between the tissue plains of the gliding surfaces can cause global motion restriction and pain. Global motion restriction is a common feature of fractures of the proximal humerus. If open reduction is indicated to achieve anatomic reduction, subdeltoid scarring can be very important, especially if postoperative immobilization is required. Prominent humeral prosthetic implants impair gliding in the subdeltoid space.
Unlike in patients in the acute inflammatory stage, pain is usually present, especially in the end-range of motion, but motion limitation is the main complaint. Pain mimics the symptoms of subacromial impingement, limits active range of motion, and is localized on the lateral side of the arm. Depending on the underlying problem, specific patterns of motion restriction are observed.
Persistent motion loss after rotator cuff repair may be the result of inadequate operative technique or inadequate postoperative rehabilitation, and it is more likely to happen in patients demonstrating preoperative stiffness.20,21,91 It is very important to ensure that the patient who has a rotator cuff repair has a supple shoulder. This can be established through physical therapy prior to surgery, closed manipulation, operative release of adhesions during surgery.
Incorrect operative technique includes poor release, especially of the coracohumeral ligament, or tight closure of the rotator interval in internal rotation, leading to loss of external rotation and flexion.33,43 Repair by excessively advancing the musculotendinous unit is characterized by loss of internal rotation, if the posterosuperior rotator cuff is at issue, or by a decrease in external rotation, as seen after subscapularis repair.92 Indeed, some loss of external rotation is mandatory when repairing a chronic subscapularis tendon tear, because the motion loss means the repair is intact.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree