ACL Reconstruction in Skeletally Immature Patients
J. Lee Pace
Mininder S. Kocher
INDICATIONS/CONTRAINDICATIONS
Anterior cruciate ligament (ACL) reconstruction is indicated for patients with an ACL tear who desire to get back to cutting and pivoting sports and/or have persistent instability despite rehabilitation efforts. In skeletally immature patients, the risks of possible growth disturbance from operative intervention (1, 2, 3, 4, 5) must be weighed against the benefits of restoring stability to the knee. While conservative treatment of ACL injuries in skeletally immature patients has been a historical norm, poor outcomes have been documented repeatedly with high rates of new meniscal tears, chondral defects, early radiographic signs of osteoarthritis, and decreased levels of activity and patient-related outcome scores (6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19). As such, there have been several procedures described in the literature aimed at recreating a functional ACL for these patients while minimizing the risk of growth disturbance. Techniques described can be broadly grouped into physeal-sparing reconstruction (20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31), partial physeal reconstruction (32, 33, 34, 35, 36), and transphyseal reconstruction (5, 11, 28, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50). These techniques have had variable outcomes ranging from poor to excellent. While techniques are variable
and controversy still remains, the literature tends to support early stabilization of ACL injuries in pediatric and adolescent patients (14, 16, 17, 18, 51, 52).
and controversy still remains, the literature tends to support early stabilization of ACL injuries in pediatric and adolescent patients (14, 16, 17, 18, 51, 52).
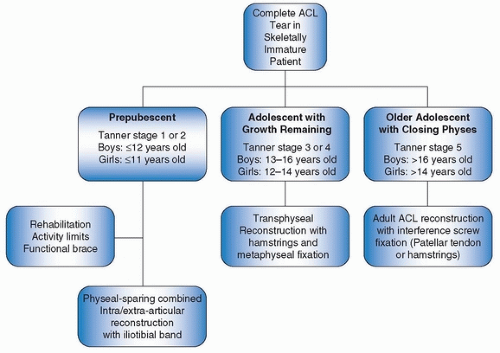 FIGURE 29-1 Algorithm to determine treatment for pediatric and adolescent patients with an ACL tear. |
The senior author has developed an algorithm (Fig. 29-1) that guides treatment based on future growth remaining (53). Prepubescent patients are recommended for a physeal-sparing ACL reconstruction utilizing autologous iliotibial (IT) band in a combined extra- and intra-articular fashion (31). While this procedure is noted to recreate a nonanatomic ACL, research has shown it to recreate native ACL knee kinematics better than other leading pediatric ACL reconstruction options (54). Pubescent patients with growth remaining are indicated for a transphyseal ACL reconstruction using autologous hamstring tendons with metaphyseal fixation (45). Adolescent patients who are at or near skeletal maturity are deemed appropriate for adult-style ACL reconstruction with the option of utilizing grafts with bone plugs and interference screw fixation at the discretion of the surgeon and patient. Prepubescent is defined as patients who are Tanner stage 1 or 2, males with a bone age of ≤12, and females with a bone age of ≤11 (55, 56). Pubescent patients are Tanner stage 3 or 4 and/or have a bone age of 13 to 16 in males or 12 to 14 in females. Patients at or near skeletal maturity are considered Tanner stage 5 with a bone age greater than 16 in male and greater than 14 in females (Fig. 29-1).
Contraindications for ACL reconstruction in skeletally immature patients are generally the same as for older individuals and include advanced osteoarthritis, chronic infection, uncontrolled inflammatory conditions in the knee, preexisting angular knee deformity, or patient noncompliance.
PREOPERATIVE PREPARATION
Preparation for this procedure begins in clinic with a thorough history and physical exam. Focused exam of the knee includes a Lachman exam, anterior drawer test, and possibly a pivot shift exam, if the patient tolerates it, to determine clinical ACL insufficiency. Concomitant injuries should be assessed such as meniscal tears, chondral injuries, and other ligamentous injuries, and appropriate exam maneuvers should be performed to determine if these exist. If there is clinical suspicion of an ACL tear, appropriate imaging should be ordered. X-rays are ordered to rule out fracture and also to get an idea of the patient’s physeal status in the knee. Magnetic resonance imaging (MRI) is the gold standard imaging tool to diagnose an ACL tear and can identify concomitant injuries such as meniscal tear, articular cartilage injury, and multiligamentous injury. Once the tear is confirmed on imaging, an assessment of the patient’s physical maturity is performed. An AP x-ray of the left hand (“bone age” x-ray) is ordered, and the Greulich and Pyle (55) manual is used to determine bone age. Tanner staging (56) typically involves asking questions regarding recent maturational milestones such as onset of menses, presence of pubic hair, etc. A focused exam of these areas is not routinely performed in clinic but can be confirmed under general anesthesia in the operating room. If the exam
is borderline regarding physiologic status, it is the authors’ practice to err on the younger side when recommending treatment.
is borderline regarding physiologic status, it is the authors’ practice to err on the younger side when recommending treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








