A1 Pulley Release for Trigger Finger with and without Flexor Digitorum Superficialis Ulnar Slip Excision
David H. MacDonald
Alexander M. Marcus
DEFINITION
Trigger finger is an entrapment of the digital flexor tendon(s) by the flexor tendon sheath.
Trigger finger progressively causes inflammation, pain, catching, locking, and reduced range of motion (ROM).
ANATOMY
The flexor digitorum profundus and superficialis (flexor pollicis longus in the thumb) pass under (dorsal to) the flexor sheath, which consists of annular and cruciate pulleys.
PATHOGENESIS
High angular loads at the A1 pulley and often other causes of local inflammation result in a flexor tendon sheath whose inner diameter is too narrow to accommodate the flexor tendon(s).
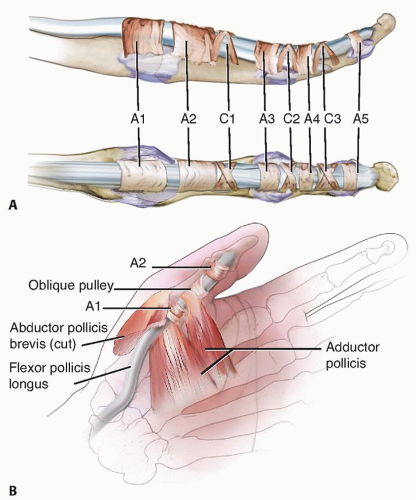
FIG 1 • To understand trigger finger and its release, an appreciation of the flexor tendon pulley system of the finger (A) and thumb (B) is required.
This size mismatch causes hypertrophy (thickening) of the A1 pulley and tendinous swelling.
These changes exacerbate the size discrepancy, setting up a cycle in which entrapment causes hypertrophy and hypertrophy causes entrapment.
NATURAL HISTORY
Trigger digits may develop spontaneously or may occur after swelling, from either trauma or a period of heavy use.
Trigger digits may:
Resolve spontaneously (especially in mild cases)
Persist with the same level of symptoms
Advance to passively correctable locking
Become indefinitely locked in either flexion or extension
PATIENT HISTORY AND PHYSICAL FINDINGS
The history may include any of the following:
Pain in the distal palm, often radiating proximally along the path of the flexor tendon(s)
Pain occurring with use and difficulty grasping objects or flexing the digit
Clicking or locking with digital flexion and extension, which is often perceived by the patient to be at the proximal interphalangeal (PIP) joint
The finger being stuck in flexion, often in the morning, requiring the other hand to straighten it
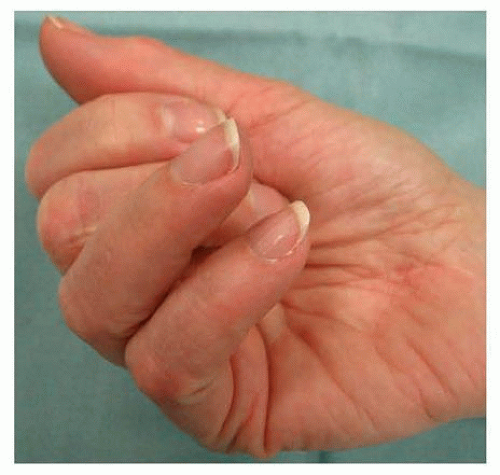
Being unable to flex or extend the digit fully or at all (FIG 2)
The history should elicit the following information:
Whether the patient has had a trigger finger before, in either the currently involved or any other digit
Previous treatments for trigger finger and the extent and duration of the result
Whether the condition began after a particular incident or period of increased hand use
The patient’s medical history should be evaluated for conditions that may cause trigger fingers and alter treatment as well as commonly associated conditions, including the following:
Diabetes
Rheumatoid arthritis and other inflammatory arthropathies
Amyloidosis, most commonly secondary to renal disease requiring dialysis
Lysosomal storage diseases
Carpal tunnel syndrome (often seen in patients with trigger finger but not causally related)
The history and physical examination should exclude other conditions that cause overlapping symptoms, including the following:
Nerve compression
Muscle weakness
Tendon interruption from laceration (partial or complete) or rupture
Pulley rupture and bowstringing
Joint or soft tissue contracture or swelling or both
Extensor tendon laceration or subluxation, especially at the MCP joint
Joint dislocation
MCP joint collateral ligament injury
The physical examination should include the following:
ROM test, which is the most objective measure of severity. If the patient has absolutely no active motion at the PIP (or thumb interphalangeal [IP]), consider tendon interruption.
Palpation of the palm. If the A1 pulley is not tender, strongly consider other diagnoses. Examine for other causes of the patient’s symptoms, including Dupuytren contracture, tendon sheath ganglion, PIP joint injury, and A3 pulley triggering.
Examination of the extensor apparatus. Rule out extensor mechanism abnormalities and stress test the collateral ligaments of the MCP joint (radially and ulnarly) to rule out conditions that may cause overlapping signs or symptoms, including a popping sensation with ROM.
Examination of the collateral ligaments at the MCP joint. Stress the collateral ligaments radially and ulnarly.
Perform a neurovascular examination. Carpal tunnel syndrome often is associated with trigger finger. Muscle weakness may cause similar findings. Any neurovascular deficit should be documented before treatment.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs can exclude some unusual causes of trigger finger symptoms and can assess for arthritis but are not required to make the diagnosis of trigger finger.
Ultrasound/dynamic ultrasound has been increasingly useful in confirmation of diagnosis and in guiding corticosteroid therapy for trigger finger.9
If other pathology is suspected, magnetic resonance imaging (MRI) can be useful.
Nerve conduction studies can evaluate for anterior interosseous nerve (AIN) compression, which may mimic a trigger thumb or concomitant carpal tunnel syndrome.
DIFFERENTIAL DIAGNOSIS
Extensor tendon subluxation at the MCP joint
Joint contracture or injury, including MCP locking due to collateral ligaments and a swollen PIP joint
Soft tissue swelling or contracture, including Dupuytren contracture
Partial tendon laceration
Triggering at the A3 pulley (rare)
Muscle weakness, including flexor pollicis longus weakness secondary to AIN palsy
Masses (especially tendon sheath ganglions), which may cause A1 pulley tenderness
NONOPERATIVE MANAGEMENT
Observation and splinting
Mild, early cases often resolve spontaneously or do not bother the patient significantly.
Use of a night extension splint may help minimize morning locking.
Unless the PIP joint remains locked, in either flexion or extension, for several weeks, delayed treatment usually does not significantly change either the options available or their results.
Injection
Long-term relief in most affected digits with one to three injections2
Injection technique (FIG 3)
One milliliter of 2% plain (no epinephrine) lidocaine and 1 mL of a soluble corticosteroid solution (eg, betamethasone or dexamethasone) in a single syringe with a 25-gauge needle is given.
The A1 pulley area is prepped with an antiseptic solution such as alcohol or Betadine.
A topical spray may be used to reduce discomfort.
One to 2 mL is injected in the sheath or subcutaneously around the A1 pulley.13 Avoid injecting into the tendon itself; if increased resistance is encountered, this may be the cause.
Ultrasound guidance may provide increased accuracy and avoid possible complications especially in the thumb.9
SURGICAL MANAGEMENT
Indications for surgical treatment include the following:
Symptoms that persist despite conservative management
Inability to flex or extend the finger even passively: This is an indication for earlier release to prevent secondary joint contracture.
Open A1 pulley release is indicated for any routine trigger finger.
Percutaneous trigger finger release:
Requires an actively triggering digit so the patient can flex to confirm needle placement and pulley release
Is used primarily for the middle and ring fingers. Use in the other digits may place digital nerves in jeopardy.15
In patients with very extensive synovitis, such as that seen in rheumatoid arthritis, lysosomal storage diseases, or amyloidosis associated with end-stage renal disease, releasing the A1 pulley percutaneously or through a routine, small
incision is often not sufficient. A more extensive tenosynovectomy and sometimes ulnar slip of the flexor digitorum superficialis resection (USSR) is often required.
Preoperative Planning
Clinical notes and any studies obtained preoperatively should be reviewed.
If procedures beyond an A1 pulley release are considered likely to be necessary (eg, possible resection of the ulnar slip of the flexor digitorum superficialis [FDS]), they should be discussed with the patient preoperatively.