Multiple systems for classifying osteochondritis dissecans (OCD) of the knee have been reported. These existing classification systems have some similar characteristics, such as stable lesion/intact articular cartilage and presence of a loose body. However, variations are found in the number of stages and specific lesion characteristics assessed. Currently, no system has been universally accepted. A future classification system should be developed that reconciles the discrepancies among the current systems and provides a clear, consistent, and reliable method for classifying OCD lesions of the knee during arthroscopy.
Key points
- •
Multiple systems have been described for classifying osteochondritis dissecans (OCD) lesions of the knee during arthroscopy, with varying levels of overlap among the existing classification systems.
- •
The identified classification systems associate intact articular cartilage with lesion stability, whereas instability is associated with a disruption of the articular cartilage.
- •
None of the studies included in this review rigorously assessed the inter-rater and intra-rater reliability of an arthroscopic grading system for OCD lesions of the knee.
- •
Future research is needed to establish a classification system for OCD of the knee during arthroscopy that demonstrates high inter-rater and intra-rater reliability.
Introduction
Osteochondritis dissecans (OCD) is a focal, idiopathic alteration of subchondral bone with potential for instability and disruption of adjacent articular cartilage that may result in premature osteoarthritis. Several risk factors have been linked to OCD of the knee, including male sex, age (with 10–20 years being at highest risk), sports participation, and African-American ethnicity. Three primary methods have been used to assess the stability, severity, and potential for healing of the OCD lesion: radiographs, magnetic resonance imaging (MRI), and arthroscopy. Although many methods have been developed to classify the various stages of OCD lesions, none has been rigorously validated for accuracy, ease of use, or prognostic predictive ability.
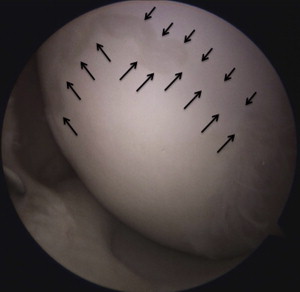
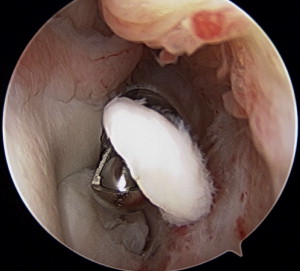
The main principle underlying the classification of OCD lesions focuses on the stability of the lesion. The term stability , in regard to OCD lesions, has been used to describe the mechanical integrity and stability of the subchondral OCD lesion. Furthermore, characteristics of a stable lesion ( Figs. 1 and 2 ) include those that have stable articular cartilage, whereas a disruption in the articular cartilage ( Fig. 3 ) is present in lesions that are usually loose or unstable ( Fig. 4 ). Some lesions may be stable but do include a breech in the articular cartilage.


Multiple grading systems exist for classifying OCD of the knee during arthroscopic surgery. However, variation among these classifications and the lack of a standardized method for grading OCD lesions prevents comparison among the published literature on arthroscopy of OCD of the knee. This article reviews the English-written literature for existing systems for classifying OCD lesions of the knee during arthroscopic surgery.
Introduction
Osteochondritis dissecans (OCD) is a focal, idiopathic alteration of subchondral bone with potential for instability and disruption of adjacent articular cartilage that may result in premature osteoarthritis. Several risk factors have been linked to OCD of the knee, including male sex, age (with 10–20 years being at highest risk), sports participation, and African-American ethnicity. Three primary methods have been used to assess the stability, severity, and potential for healing of the OCD lesion: radiographs, magnetic resonance imaging (MRI), and arthroscopy. Although many methods have been developed to classify the various stages of OCD lesions, none has been rigorously validated for accuracy, ease of use, or prognostic predictive ability.
The main principle underlying the classification of OCD lesions focuses on the stability of the lesion. The term stability , in regard to OCD lesions, has been used to describe the mechanical integrity and stability of the subchondral OCD lesion. Furthermore, characteristics of a stable lesion ( Figs. 1 and 2 ) include those that have stable articular cartilage, whereas a disruption in the articular cartilage ( Fig. 3 ) is present in lesions that are usually loose or unstable ( Fig. 4 ). Some lesions may be stable but do include a breech in the articular cartilage.
Multiple grading systems exist for classifying OCD of the knee during arthroscopic surgery. However, variation among these classifications and the lack of a standardized method for grading OCD lesions prevents comparison among the published literature on arthroscopy of OCD of the knee. This article reviews the English-written literature for existing systems for classifying OCD lesions of the knee during arthroscopic surgery.
Review of the literature
Radiographic and MRI Classifications
Berndt and Harty described one of the first classification systems in 1959. They classified talar OCD lesions on radiographic images, with stages ranging from a small area of compression of the subchondral bone to a completely detached fragment or loose body. Rodegerdts and Gleissner described an early classification system for OCD of the knee in 1981. They classified lesions on radiographic images, with 5 stages ranging from a potentially depressed osteochondral fracture to a displaced fragment or loose body. Subsequent authors have described additional radiographic methods of classification, all with various ranges of modifications and reclassifications.
Several authors have also described classification systems for OCD of the knee for MRI. These classifications do share some similarities. Many of the existing classification systems describe intact articular cartilage for stable or low-graded lesions. Similarly, multiple authors also agree that high-signal intensity between the parent bone and progeny fragment indicates lesion instability, although in some cases this higher signal may indicate healing or fibrous tissue at the interface. However, arthroscopic visualization remains the reference standard for determining the stability of an OCD lesion of the knee.
Arthroscopic Classification Systems for OCD of the Knee
In 1979, Guhl published a report on the arthroscopic treatment of OCD. This report began with a statement that arthroscopy should first begin with classification of the lesion. Guhl described 4 variations of lesions: intact lesions, early separation, partial detachment, and craters and loose bodies ( Table 1 ). Although Guhl’s classification was simple, it provided a foundation on which others have built more comprehensive systems classifying OCD of the knee. This classification also identified an important aspect of OCD lesions: delineating between stable (intact lesions) or unstable (separation and eventual loose body formation). This distinction between stable and unstable is present in many of the subsequent classification systems.







