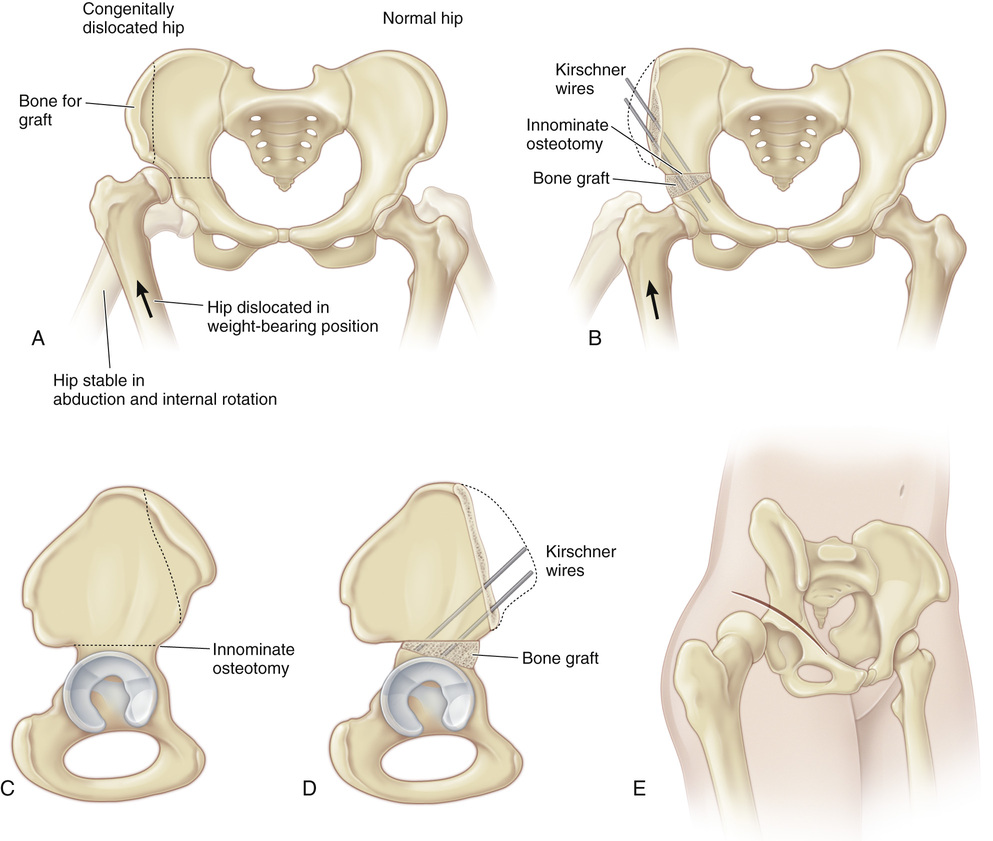
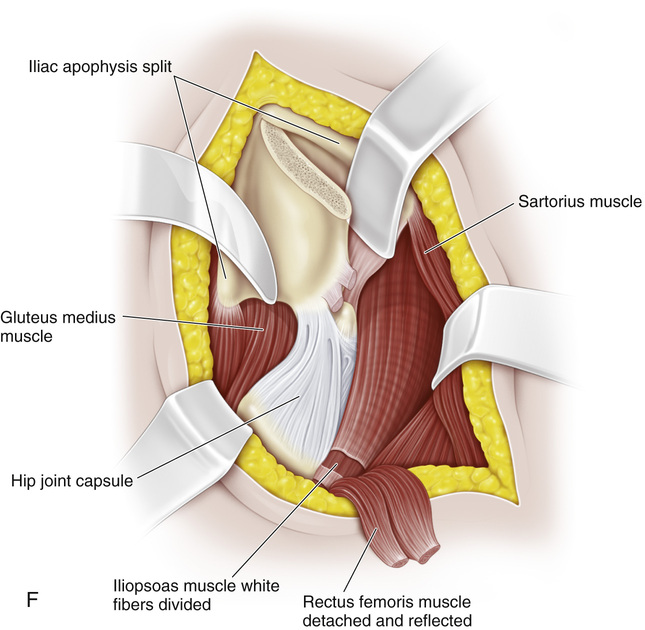
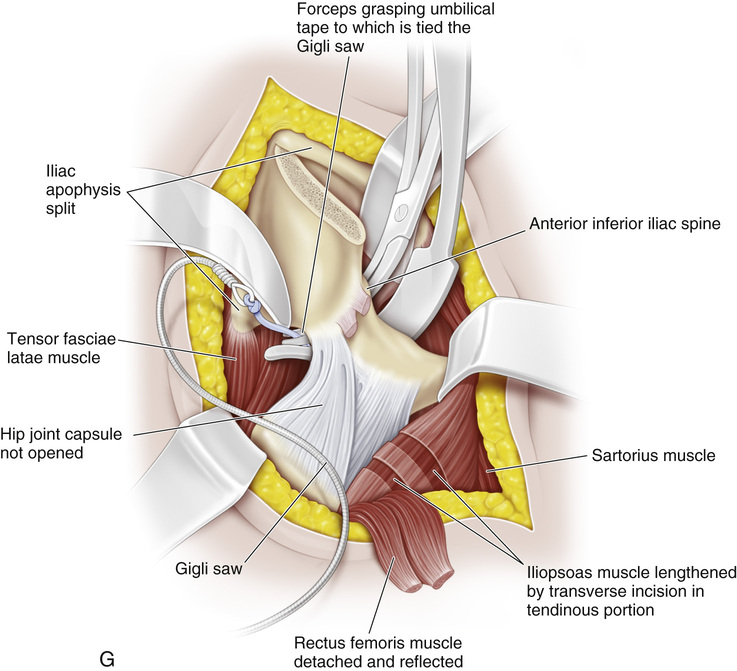
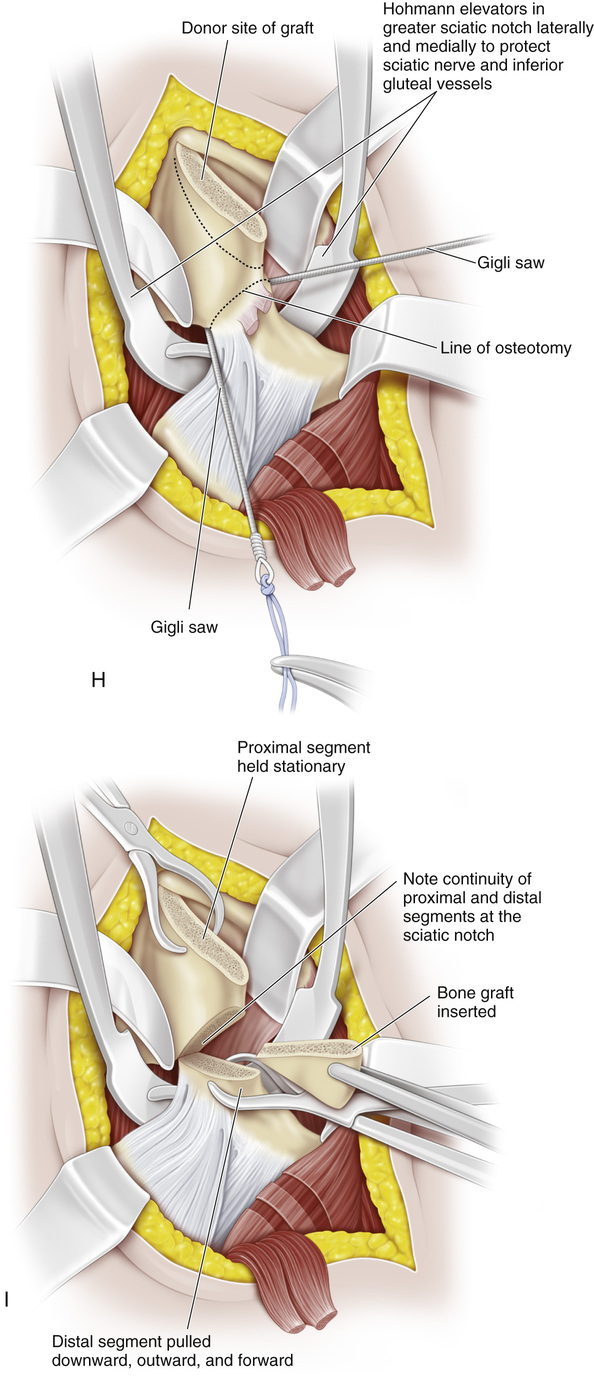
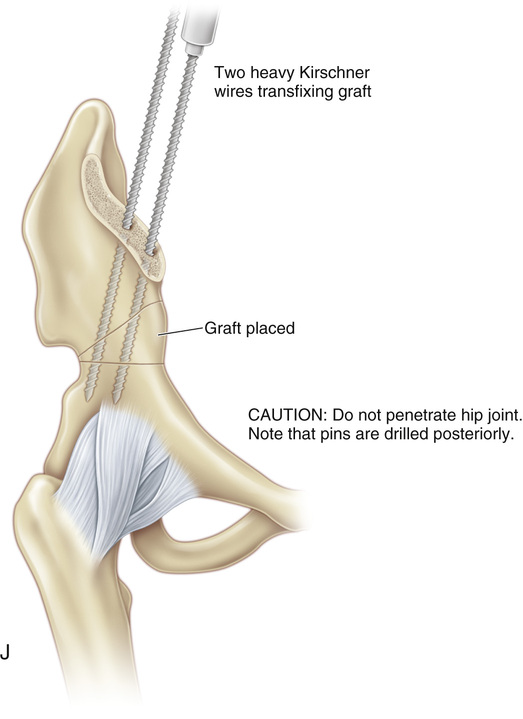
(see Video 5) A to D, The Salter innominate osteotomy is based on the redirection of the acetabulum as a unit by hinging and rotation through the symphysis pubis, which is mobile in children. It is performed by making a transverse linear cut above the acetabulum at the level of the greater sciatic notch and the anterior inferior iliac spine. The whole acetabulum with the distal fragment of the innominate bone is tilted downward and laterally by rotating it. The new position of the distal fragment is maintained by a triangular bone graft that is taken from the proximal portion of the ilium and inserted into the open-wedge osteotomy site. Internal fixation is provided by two threaded Kirschner wires. Through the rotation and redirection of the acetabulum, the femoral head is covered adequately with the hip in a normal weight-bearing position. In other words, the reduced dislocation or subluxation that was previously stable in the position of flexion and abduction is now stable in the extended and neutral position of weight bearing. E, The skin is prepared with the patient in the side-lying position so that the abdomen, the lower part of the chest, and the affected half of the pelvis can be draped to the midline anteriorly and posteriorly; the entire lower limb is also prepared and draped to allow for the free motion of the hip during the operation. The patient is placed supine with a roll beneath the buttock. The skin incision is an oblique bikini incision. The incision that was formerly used over the iliac crest produces an unsightly scar, whereas the bikini incision results in excellent exposure and cosmesis. The anterior inferior iliac spine is palpated and marked. The incision begins approximately two thirds of the distance from the greater trochanter to the iliac crest and extends across the inferior spine and 1 or 2 cm beyond the inferior spine. The incision is then retracted over the iliac crest, and the dissection is carried down to the apophysis of the crest. Anteriorly, the tensor–sartorius interval is bluntly dissected, beginning distally and working proximally. The lateral femoral cutaneous nerve appears just medial to this interval and just distal to the inferior iliac spine, and it should be protected. F, With a scalpel, the cartilaginous iliac apophysis is split in the middle down to the bone from the junction of its posterior and middle thirds to the anterior superior iliac spine. With the use of blunt dissection, the groove between the tensor fasciae latae and the sartorius and rectus femoris muscles is opened and developed. With a broad and long-handled periosteal elevator, the surgeon strips the lateral part of the iliac apophysis and the tensor fasciae latae and gluteus medius and minimus muscles subperiosteally and the greater sciatic notch posteromedially. G, Next, the periosteum is elevated from the medial and lateral walls of the ilium all the way posteriorly to the sciatic notch. It is vital to stay within the periosteum to prevent injury to the superior gluteal vessels and the sciatic nerve. A common pitfall is the inadequate surgical exposure of the sciatic notch, which makes it difficult to pass the Gigli saw behind the notch. The space on the lateral wall of the ilium is packed with sponge to dilate the interval and to control the oozing of blood. The periosteum is then elevated from the inner wall of the ilium in a continuous sheet to expose the sciatic notch medially. Again, it is important to stay in the subperiosteal plane to avoid injury to the vessels and nerves. The medial space is packed with sponge. The sartorius muscle can usually be reflected medially with the medial half of the cartilaginous iliac apophysis. If it is difficult to do so or if more distal exposure is desired, the origin of the sartorius muscle is detached from the anterior superior iliac spine, its free end is marked with whip sutures for later reattachment, and the muscle is reflected distally and medially. The two heads of origin of the rectus femoris—the direct one from the anterior inferior iliac spine and the reflected one from the superior margin of the acetabulum— Next, on the deep surface of the iliopsoas muscle, the psoas tendon is exposed at the level of the pelvic rim. The iliopsoas muscle is rolled over so that its tendinous portion can be separated from the muscular portion. If identification is in doubt, a nerve stimulator is used to distinguish the psoas tendon from the femoral nerve. A Freer elevator is passed between the tendinous and muscular portions of the iliopsoas muscle, and the psoas tendon is sectioned at one or two levels. The divided edges of the tendinous portion retract, and the muscle fibers separate, thus releasing the contractures of the iliopsoas without disturbing the continuity of the muscle. Two medium-sized Hohmann elevator retractors—one introduced from the lateral side and the other from the medial side of the ilium—are placed subperiosteally in the sciatic notch. This step is crucial: in addition to keeping the neurovascular structures out of harm’s way, the Hohmann retractors maintain the continuity of the proximal and distal innominate segments at the sciatic notch. A right-angle forceps is passed subperiosteally from the medial side of the ilium and guided through the sciatic notch to the outer side with the index finger of the surgeon’s opposite hand. The Gigli saw is most easily passed by first passing an umbilical tape through the notch. The end of the tape is tied to the Gigli saw. The tape is grasped with the right-angle clamp and pulled through the notch; it in turn pulls the saw through the notch. H, The osteotomy line extends from the sciatic notch to the anterior inferior iliac spine, and it is perpendicular to the sides of the ilium. It is vital to begin the osteotomy well inferiorly in the sciatic notch; the tendency is to start too high. The handles of the Gigli saw are kept widely separated and in continuous tension to keep the saw from binding in the soft cancellous bone. The osteotomy, which emerges anteriorly immediately above the anterior inferior iliac spine, is completed with the Gigli saw. The use of an osteotome may subject the superior gluteal artery and the sciatic nerve to iatrogenic damage. I, The Hohmann retractors are kept constantly at the sciatic notch by an assistant to prevent the posterior or medial displacement of the distal segment and the loss of bony continuity posteriorly. A triangular full-thickness bone graft is removed from the anterior part of the iliac crest with a large, straight, double-action bone cutter. The length of the base of the triangular wedge represents the distance between the anterior superior iliac spine and the anterior inferior iliac spine. The portion of bone to be removed as a bone graft is held firmly with a Kocher forceps; the operator must be sure that this portion does not fall on the floor or get contaminated. The proximal fragment of the innominate bone is held steady with a large towel-clip forceps, and the distal fragment is grasped with a second stout towel forceps. The affected hip is placed in 90 degrees of flexion, maximal abduction, and 90 degrees of lateral rotation; a second assistant applies distal and lateral traction to the thigh. With the second towel clip placed well posteriorly on the distal fragment, the surgeon rotates the distal fragment downward, outward, and forward, thereby opening the osteotomy site anteriorly. The site must be kept closed posteriorly. Leaving it open posteriorly displaces the hip joint distally without adequate rotation and redirection of the acetabulum at the symphysis pubis; furthermore, it will lengthen the lower limb unnecessarily. Another technical error to avoid is opening the osteotomy site with a mechanical spreader (e.g., a laminectomy spreader, a self-retaining retractor) because that may move the proximal fragment upward and the distal fragment downward without rotating the distal fragment through the symphysis pubis. The acetabular maldirection will not be corrected unless such rotation of the distal fragment takes place. The posterior and medial displacement of the distal fragment should be avoided. When the periosteum on the median wall of the ilium is taut, the cartilaginous apophysis of the ilium is divided at two or three levels; this will help with the rotation of the acetabulum. J, Next, the bone graft is shaped with bone cutters to the appropriate size to fit the open osteotomy site. The graft is usually about the correct size for the size of the patient because the base of the triangular graft represents the distance between the anterior superior iliac spine and the anterior inferior iliac spine. The surgeon should avoid using a large graft and hammering it in to fit snugly into the osteotomy site because this will open the site posteriorly. With the osteotomy site open anteriorly and the distal segment rotated, the bone graft is inserted into the opened-up osteotomy. The distal fragment of the innominate bone should be kept slightly anterior to the proximal fragment. When traction is released, the graft is firmly locked by the two segments of the bone. A stout threaded Kirschner wire is drilled from the proximal segment across the osteotomy site, through the graft, and into the distal segment posterior to the acetabulum, thereby preventing any future displacement of the graft or the distal segment. The first wire should be directed posterior to the acetabulum. Radiographs are obtained to check the adequacy of correction of the acetabular maldirection and the position of the Kirschner wire. A second Kirschner wire is then drilled parallel to the first to further stabilize the internal fixation of the osteotomy. In the older child, we use a third threaded Kirschner wire or two cancellous positional screws to ensure the security of internal fixation. The inadequate penetration of the wires into the distal fragment will result in the loss of alignment of the osteotomy. The wires may bend or break, or, if they are excessively heavy, they may fracture the graft or the innominate bone; the importance of choosing the correct diameter of wire or cancellous screw cannot be overemphasized. The penetration of the wires into the hip joint may cause chondrolysis of the hip, or it may cause the wire to break at the joint level. An anteroposterior radiograph of the hips is obtained to check the depth of the Kirschner wires and the degree of correction that has been obtained. The two halves of the cartilaginous iliac apophysis are sutured together over the iliac crest. The rectus femoris and sartorius muscles are reattached to their origins, and the wound is closed in a routine manner. Skin closure should be with continuous subcuticular 00 nylon suture. The Kirschner wires are cut so that their ends are in the subcutaneous fat and easily palpable. A one-and-one-half-hip spica cast is applied with the hip in a stable weight-bearing position. Immobilization in a forced or extreme position should be avoided because it will cause the excessive and continuous compression of articular cartilage, osteonecrosis, permanent joint stiffness, and eventual degenerative arthritis. In the cast, the knee is bent to control the position of hip rotation. When there is excessive femoral antetorsion, the hip is immobilized in slight medial rotation. A common pitfall is immobilization in marked medial rotation; this mistake will result in posterior subluxation or dislocation of the femoral head. With femoral retrotorsion, the hip should be immobilized in slight lateral rotation. A radiograph of the hips through the cast is obtained before the child is discharged from the hospital. Another set of radiographs is obtained 2 to 3 weeks after surgery to ensure that the graft has not collapsed, that the pins have not migrated, and that there is no medial displacement of the distal segments. In the older cooperative patient, when cancellous screws are used for internal fixation, a hip spica cast is not necessary.
Salter Innominate Osteotomy
Operative Technique
![]()
 are divided at their origin, marked with whip sutures, and reflected distally.
are divided at their origin, marked with whip sutures, and reflected distally.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








