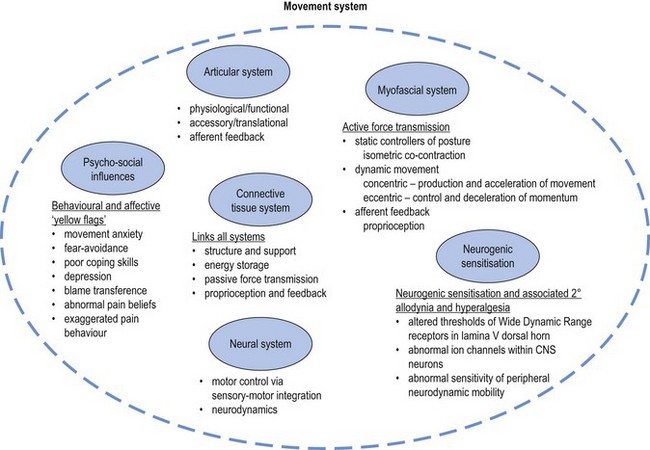
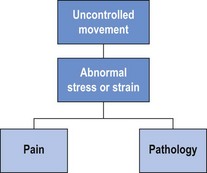
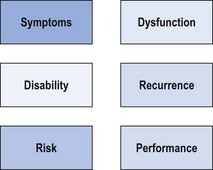
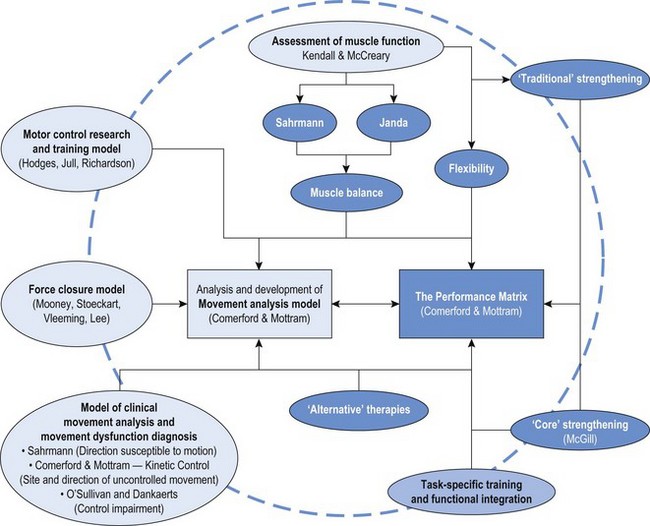
Chapter 1 The movement system comprises the coordinated interaction of the articular, the myofascial, the neural and the connective tissue systems of the body along with a variety of central nervous system, physiological and psycho-social influences (Figure 1.1). It is essential to assess and correct specific dysfunction in all components of the movement system and to assess the mechanical inter-relationships between the articular, myofascial, neural and connective tissue systems. This chapter will describe a systematic approach to evaluation of the movement system and identification of the relative contributions of individual components to movement dysfunction. Identifying and classifying movement faults is fast becoming the cornerstone of contemporary rehabilitative neuromusculoskeletal practice (Comerford & Mottram 2011; Fersum et al 2010; Sahrmann 2002). In recent years clinicians and researchers have described movement faults and used many terms to describe these aberrant patterns. These terms include substitution strategies (Richardson et al 2004; Jull et al 2008), compensatory movements (Comerford & Mottram 2001a), muscle imbalance (Comerford & Mottram 2001a; Sahrmann 2002), faulty movement (Sahrmann 2002), abnormal dominance of the mobiliser synergists (Richardson et al 2004; Jull et al 2008), co-contraction rigidity (Comerford & Mottram 2001a), movement impairments (Sahrmann 2002; O’Sullivan et al 2005) and control impairments (O’Sullivan et al 2005; Dankaerts et al 2009). All of these terms describe aspects of movement dysfunction, many of which are linked to UCM. The focus of this text is to describe UCM and explore the relationship of UCM to dysfunction in the movement system (Comerford & Mottram 2011). Movement dysfunction represents multifaceted problems in the movement system and the therapist needs the tools to relate UCM and faults in the movement system to symptoms, recurrence of symptoms and disability. Skills are required to analyse movement, make a clinical diagnosis of movement faults and apply a patient-specific retraining program and management plan to deal with pain, disability, recurrence of pain and dysfunction. Sahrmann (2002) has promoted the concept that faulty movement can induce pathology, not just be the result of it; that musculoskeletal pain syndromes are seldom caused by isolated events; and that habitual movements and sustained postures play a major role in the development of movement dysfunction. These statements have been fundamental in the development of the movement dysfunction model. Clinical situations which have a major component of movement dysfunction contributing to pain include: postural pain; pain of insidious onset; static loading or holding pain; overuse pathology (low force repetitive strain or high force and/or impact repetitive strain); recurrent pain patterns; and chronic pain. It is important to identify UCM in the functional movement system. It is our hypothesis that the uncontrolled segment is the most likely source of pathology and symptoms of mechanical origin. There is a growing body of evidence to support the relationship between UCM and symptoms (Dankaerts 2006a, 2006b; Luomajoki et al 2008; van Dillen et al 2009). The direction of UCM relates to the direction of tissue stress or strain and pain producing movements. Therefore it is important in the assessment to identify the site and the direction of UCM and relate it to the symptoms and pathology. The UCM identifies the site and the direction of dynamic stability dysfunction and is related to the direction of symptom-producing movement. For example, UCM into lumbar flexion under a flexion load may place abnormal stress or strain on various tissues and result in lumbar flexion-related symptoms. Likewise, uncontrolled lumbar extension under extension load produces extension-related symptoms, while uncontrolled lumbar rotation or side-bend and/or side-shift under unilateral load produces unilateral symptoms. Figure 1.2 illustrates the link between UCM and pain. Abnormal stress or strain that exceeds tissue tolerance can contribute to pain and pathology. The relationship between UCM and pain/pathology will be explored further in Chapter 3. In this text the identification and classification of movement faults are described in terms of site and direction of UCM. These movement faults will be discussed in Chapter 2 in relation to changes in motor recruitment and strength (Comerford & Mottram 2001b, 2011). Scientific literature and current clinical practice are linking the site and direction of UCM in relation to symptoms, disability, dysfunction, recurrence, risk and performance (Figure 1.3). Pain is frequently one of the main symptoms that the patient presents with to the therapist and is inherently linked to movement dysfunction. Contemporary research clearly demonstrates that individuals with pain present with aberrant movement patterns (Dankaerts et al 2006a, 2009; Falla et al 2004; Ludewig & Cook 2000; Luomajoki et al 2008; O’Sullivan et al 1997b, 1998). Research has demonstrated a consistent finding: in the presence of pain, a change occurs in recruitment patterns and the coordination of synergistic muscles. Individuals with pain demonstrate patterns of movements that would normally be used only in the performance of high load or fatiguing tasks (e.g. pushing, pulling, lifting weights) to perform low load non-fatiguing functional tasks (e.g. postural control and non-fatiguing normal movements). Clearly UCM is a feature of many musculoskeletal pain presentations and identifying and classifying these movement faults is essential if therapists are to effectively manage symptoms by controlling movement faults. Disability is the experienced difficulty doing activities in any domain of life (typical for one’s age and sex group, e.g. job, household management, personal care, hobbies, active recreation) due to a health or physical problem (Verbrugge & Jette 1994). Movement faults are related to disability. For example, Lin et al (2006) demonstrated that changes in scapular movement patterns (in particular a loss of posterior tilt and upward rotation) correlated significantly with self-report and performance-based functional measures indicating disability. The relationship between disability and movement faults has been identified in many other fields of physical therapy (e.g. neurological and amputee rehabilitation). Indeed, in relation to gait dysfunction, management and retraining of UCM is a key factor in rehabilitation of people with lower limb amputations using a prosthesis (Hirons et al 2007). Reduction of disability is the primary long-term goal of therapy or rehabilitation. Disability is individual and what one person considers disability another person might consider exceptional function. For example, an elite athlete’s disability may be a function that most people do not have the ability to do, do not want to do or need to do. Movement dysfunction, however, can affect a person’s ability to function independently and therefore decrease quality of life. The disablement process model in disease as well as in rehabilitation is gaining recognition (Escalante & del Rincon 2002; Verbrugge & Jette 1994) and retraining movement faults has been shown to improve function (O’Sullivan et al 1997a; Stuge et al 2004). The process of identifying and measuring UCM, and linking UCM to musculoskeletal pain, and to changes in muscle function, is a developing area of active research in the field of pain and movement dysfunction (Gombatto et al 2007; Luomajoki et al 2007, 2008; Mottram et al 2009; Morrissey et al 2008; Scholtes et al 2009; Roussel et al 2009a; van Dillen et al 2009). Muscle dysfunction is most clearly apparent in people with pain (Falla & Farina 2008; Hodges & Richardson 1996; Hungerford et al 2003; Lin et al 2005). The changes in muscle function underlying pain can present in two ways: 1) as altered control strategies (van Dillen et al 2009; O’Sullivan 2000); and 2) as physiological peripheral muscle changes (Falla & Farina 2008). Physiological changes associated with muscle dysfunction are discussed further in Chapter 2, and altered control strategies are discussed further in Chapter 3. The correction or rehabilitation of dysfunction has been shown to decrease the incidence of pain recurrence (Hides et al 1996; Jull et al 2002; O’Sullivan et al 1997a). This reinforces the need for therapy to be aimed at correcting dysfunction in the management of musculoskeletal disorders and not just relieving symptoms. Evidence suggests history of injury is a predictive factor for re-injury and therefore outcome measures that are defined in terms of normal range of joint motion and muscle strength are inadequate to prevent recurrence (Mottram & Comerford 2008). Making the link between UCM and pain is not new, but the concept of linking it to injury prevention is. Some recent research has highlighted the potential for linking UCM to risk of injury. A recent study on dancers identified two movement control tests that may be useful for the identification of dancers at risk of developing musculoskeletal injuries in the lower extremities (Roussel et al 2009a). Athletes with decreased neuromusculoskeletal control of the body’s core (core stability) are at an increased risk of knee injury (Zazulak et al 2007). Indeed, there is now growing evidence that motor control and physical fitness training prevent musculoskeletal injuries (Roussel et al 2009b), highlighting the importance for therapists to be more knowledgeable about movement control and function. Figure 1.4 illustrates the development of the movement analysis model. The movement analysis model identifies UCM in terms of the site (joint), direction (plane of motion) and recruitment threshold (low or high) and further establishes links to pain, disability, dysfunction, recurrence, risk of injury and performance. This model has been developed through the analysis and synthesis of historical and contemporary research from many sources; however, it is not intended to be a comprehensive summary of the current level of knowledge surrounding movement analysis. Kendall and colleagues (2005) described muscle function in detail. Their now classic text has been the foundation for assessment of muscle function, especially with reference to the graded testing of muscle strength and analysing the interrelationship of strength and function. Janda (1986) had previously developed the concept of muscle imbalance and patterns of dysfunction by analysing the pattern of movement sequencing. His primary intervention was to increase extensibility of short muscles. Sahrmann (2002) and co-workers further developed the concept of muscle imbalance, again analysing patterns of movement, and have developed a diagnostic framework for movement impairments (direction susceptible to motion). The 1990s saw a huge advancement in the identification of motor control dysfunction (Jull et al 2008; Richardson et al 2004). Hodges (Hodges & Cholewicki 2007) has developed a large body of evidence linking motor control of deep muscles to spinal stability. O’Sullivan and co-workers have provided objective measurements to support the links between altered muscle recruitment and direction-related musculoskeletal pain (Dankaerts et al 2006a). From this research a classification system based on diagnostic subgroups has been proposed (Vibe Fersum et al 2009). Vleeming et al (2007) and Lee (2004) have developed the model of form and force closure and have linked this to anatomical fascial slings. McGill’s (2002) research has emphasised the importance of training more superficial muscles to stabilise the core during loaded and sporting function and is often referred to as core strengthening. All these clinicians and researchers have contributed important aspects to a comprehensive and integrated model of movement analysis. In the search to identify the defining characteristics of therapeutic exercise, a brief review and analysis of many different approaches and concepts including alternative therapies is appropriate. Some of these approaches are supported by clinical evidence (Emery et al 2010; Rydeard et al 2006). Box 1.1 lists some useful approaches to pain management and/or movement dysfunction to explore. Many exercise approaches have either stood the test of time or their popularity suggests that people who practise them feel or function better. Whilst the various exercise concepts feature distinctive elements that characterise their approach, there are features that are common to all approaches (Box 1.2). These common features may contribute to good function and warrant closer inspection and further investigation. Breathing control is a key feature in many of these therapies. The link between respiratory disorders and increased risk of development of back pain has recently been established (Smith et al 2009) and altered breathing patterns have been noted during lumbopelvic motor control tests (Roussel et al 2009c). Effective intervention requires the therapist to have a thorough understanding of the mechanisms of aberrant movement patterns, an ability to confidently diagnose and classify the movement faults and to manage these dysfunctions. Guidelines for a comprehensive analysis of movement dysfunction have been described with factors the therapist needs to consider in Box 1.3 (Comerford & Mottram 2011). An understanding of the inter-relationship of the elements of the movement is needed alongside an understanding of factors relating to normal movement, function and dysfunction (Chapter 2). A sound clinical reasoning process underpins this process to optimise the assessment and retraining strategy. This process is described in the following section. The efficient and effective management of UCM in relation to symptoms, disability, dysfunction, recurrence, risk of injury and performance is dependent on a comprehensive assessment. This should lead to a specific action plan for the individual patient. Exercise protocols do have a place in the management of musculoskeletal disorders. However, because of differences in presentation and diagnostic subgroups, effective management is dependent on assessment analysis and management planning. Exercise protocols can be effective when dysfunction can be clearly defined into diagnostic subgroups rather than based on pathology. The key to identifying these diagnostic subgroups lies in making the link between movement dysfunction and symptoms (Comerford & Mottram 2001b; Sahrmann 2002; Vibe Fersum 2009). A clinical reasoning framework can be used to develop an understanding of the relationships between movement, symptoms, dysfunction, and other factors that influence the clinical reasoning process (Comerford & Mottram 2011). Box 1.4 presents 10 key steps to understanding movement and pain. The first five steps relate specifically to the site and direction of UCM. The last five steps relate to other factors necessary to develop a full understanding of the dysfunction, as well as a management plan.
Uncontrolled movement
Understanding movement and function
Movement faults
Identification and classification of UCM
Symptoms
Disability
Dysfunction
Recurrence
Risk of injury
A model for the assessment and retraining of movement faults
Alternative therapies
The assessment and management of UCM
The clinical reasoning process
The 10 point analysis and clinical reasoning framework for UCM
Uncontrolled movement