Chapter 5 Flexion (posterior pelvic tilt) control T2 4 point: backward push test T3 Crook: double bent leg lift test T6 Sitting: double knee extension test Extension (anterior pelvic tilt/pelvic sway) control T8 Standing: thoracic extension (SWAY) test T9 Standing: thoracic extension (TILT) test T10 Sitting: chest lift (TILT) test T11 Sitting: forward lean test T12 4 point: forward rocking test T13 Crook: double bent leg lower test T14 Prone: double knee bend test T15 Prone: hip extension lift test Rotation/side-bend (open chain) control T17 Supine: single heel slide test T18 Supine: bent knee fall out test T19 Side-lying: top leg turn out test T20 Prone: single hip rotation test T21 Prone: single knee flexion test T22 Prone: hip extension lift test Rotation/side-bend (closed chain) control There is rapidly growing acceptance among clinicians and researchers that the development of movement-based diagnostic frameworks is the way forwards in managing chronic and recurrent low back pain (LBP). The systems most supported by evidence are those that examine inter-relationships between altered patterns of muscle recruitment and motor control strategies and establish a direction-based mechanism of provocation or relief of symptoms (Sahrmann 2002; Dankaerts et al 2006; Luomajoki et al 2008; Van Dillen et al 2009; Vibe Fersum et al 2009). In the lumbar spine, this approach is now well established. In the management of non-specific low back pain, the subgrouping and classification of patients’ symptoms based on the assessment of movement and motor control has become more important than trying to identify a pathology-based diagnosis (Sahrmann 2002; Fritz et al 2007; Gombatto et al 2007). The influence of movement faults on pain has been illustrated (Van Dillen et al 2009) and a link between the direction of uncontrolled motion in low threshold motor control testing and pain provocative movements identified (Sahrmann 2002; O’Sullivan 2005; Dankaerts et al 2006; Luomajoki et al 2008; Vibe Fersum et al 2009). Research to date highlights the poor to moderate treatment effects with current intervention strategies for chronic specific low back pain, highlighting the need for further research and clinical developments (Airaksinen et al 2006). Different postural positions have been shown to alter trunk muscle activation (O’Sullivan et al 2002a; O’Sullivan et al 2006). In particular a lumbopelvic upright posture (with a maintained lumbar lordosis and some anterior pelvic tilt) recruits more of the internal oblique and superficial multifidus muscles than does an upright posture of thoracic extension, where there is less lumbar extension and anterior pelvic tilt, less superficial multifidus and internal oblique recruitment and more erector spinae activation. Similarly, sway standing postures and slump sitting postures decrease activity in the internal oblique and multifidus muscles and sway standing increases the activity in rectus abdominis. These changes in muscle recruitment patterns have been linked to the presence of lumbopelvic pain (Sahrmann, 2002; O’Sullivan 2005; Dankaerts et al 2006; O’Sullivan et al 2002b, 2003, 2006). Changes in the alignment of the lumbar spine have been noted in subjects with flexion-related lumbar pain (O’Sullivan et al 2006). These people sit with their lumbar spines closer towards the end of flexion range and with more posterior pelvic tilt than healthy pain-free controls. Interestingly they also had reduced back muscle endurance compared to the controls, suggesting a link between changes in muscle function and changes in postural position. Differences in sitting postures and control of the lumbar neutral position have been identified in patients with back pain (Trudelle-Jackson et al 2008). Segmental dysfunction has been identified in low back pain subjects with uncontrolled segmental movement noted around the neutral zone, as described by Panjabi (1992), during lumbar flexion (Teyhen et al 2007). The dysfunctional movement occurs during the early part of movement when the motion should be under neuromuscular control and not at end of range where the passive osteoligamentous system contributes to stability. These changes illustrate alterations in control of segmental motion. Gombatto et al (2007) have identified different patterns of lumbar region movement during trunk lateral bending in two subgroups in people with LBP. In people with patterns of uncontrolled extension and rotation, the lumbar region demonstrated asymmetry in movement and contributed more to trunk lateral bend particularly in the early stages of lateral bending on one side. They suggest that this lumbar region movement will unilaterally load one or more lumbar segments and repeated stress on the tissues during functional movements which involve side-bend, will cause cumulative stress of the lumbar region and eventually result in pain. Van Dillen et al (2009) demonstrated that movement tests can provoke symptoms in people with LBP. These researchers explored the effect of modifying, or ‘correcting’, symptomatic alignment or movement in people with LBP. This was done by correcting the spinal alignment or movement that occurred when symptoms were provoked. The modifications involved: i) restricting movement of the lumbar spine while encouraging movement elsewhere (e.g. thoracic spine or hip); and ii) positioning and maintaining the lumbar spine in a neutral position during movement similar to the principles discussed in Chapters 3 and 4. The modifications resulted in a decrease in symptoms in the majority of patients. This illustrates a classification system of subjects with LBP based on the direction(s) of alignment and movement consistently associated with a change in symptoms. Luomajoki et al (2008) demonstrated significant differences between healthy people without back pain and back pain subjects in their ability to control movement in the lumbar spine using a battery of six movement control tests (Luomajoki et al 2008). These six tests (all of which are described later in this chapter), are based on cognitively controlling lumbar flexion, lumbar extension and lumbopelvic rotation. The back pain subjects failed a significantly greater proportion of these tests than the healthy people. The ability to perform these six movement control tests can reveal differences between subjects with chronic low back pain and subjects with acute or subacute pain (Luomajoki et al 2008). The reliability of therapist observation to identify UCM and to make consistent clinical judgements based on movement observation has significant support. Van Dillen et al (2009), Dankaerts et al (2006), Luomajoki et al (2007), Vibe Fersum et al (2009) and Roussel et al (2009) have all demonstrated good intra-tester and inter-tester reliability for observational assessment of a patient’s ability to perform cognitively learned movement patterns or motor control tests of movement control. Van Dillen et al (2009) and Morrissey et al (2008) have further demonstrated that therapist observation correlates closely with 3D motion analysis. The efficacy of retraining the activation of muscles that contribute to lumbopelvic stability is well supported (Hides et al 2001; Hodges 2003; O’Sullivan 2005; Tsao & Hodges 2008; Luomajoki et al 2010). More recently there is evidence from randomised clinical trials (RCTs) that retraining programs which focus on motor control are beneficial (Macedo et al 2009). Stabilising exercises have been shown to have an effect on pain and disability (O’Sullivan et al 1997; Moseley 2002; Stuge et al 2004) and can effectively reduce recurrence of back pain at long term follow-up (Hides et al 2001). Specific recruitment of these deep stability muscles seems to be an important part of retraining (Hall et al 2007). Motor control impairment during functional movement tasks can change following a motor learning intervention (Dankaerts et al 2007; O’Sullivan & Beales 2007a). Once the site and direction of UCM have been identified specific muscle retraining can be used to retrain control of the dysfunction. For example, ‘drawing in’ the abdominal wall, to activate the deep abdominal muscles, has been shown to decrease erector spinae activity and increase gluteus maximus activity in prone hip extension lift test (Oh et al 2007). In subjects with spondylosis and spondylo-listhesis, lumbopelvic stability training has resulted in decreased pain intensity and pain descriptor scores and improvements in functional disability levels (O’Sullivan et al 1997). Exercise interventions have been described based on the evaluation of spinal alignment with postures and during active movements of both the spine and the extremities (Maluf et al 2000; Van Dillen et al 2009). Their treatment approach is to teach the patient specific strategies to reduce the symptoms associated with movements to enable them to perform activities they would otherwise avoid. Aberrant motor control strategies have also been identified in people with sacroiliac joint (SIJ) and pelvic girdle pain. O’Sullivan et al (2002b) observed abnormal kinematics of the diaphragm and pelvic floor during an active straight leg raise test in subjects with SIJ pain, and noted that these aberrant motor control strategies could be eliminated with manual compression during the test. In addition these people demonstrated bracing strategies in the abdominal wall not seen in the non-pain group. Transversus abdominis recruitment has been shown to increase sacroiliac joint stiffness to a significantly greater degree than the general abdominal exercise pattern illustrating the stability role that this muscle has on the SIJ (Richardson et al 2002). The diagnosis of the site and direction of UCM in the lumbar spine can be identified in terms of the site (being lumbar) and the direction of flexion, extension and rotation/side-bend (asymmetry) (Table 5.1). As with all UCM, the motor control deficit can present as uncontrolled translational movement (e.g. spondylolisthesis at L5–S1) or uncontrolled range of functional movement (e.g. lumbar flexion) (Sahrmann 2002; O’Sullivan 2005). The site and direction of UCM at the lumbar spine can be linked with different clinical presentations, postures and activities aggravating symptoms. The typical assessment findings in the lumbar spine are identified in Table 5.2. The key principles for assessment and classification of UCM have previously been described in Chapter 3. All dissociation tests are performed with the lumbar spine in the neutral training region. 1. Place a short piece of adhesive strapping tape across the primary hinging segment. The skin is tensioned from the adjacent segment below to the adjacent segment above. If the subject cannot prevent flexion across this segment, the tape pulls off the skin when uncontrolled flexion is produced. 2. Place one finger tip on the spinous process of the primary hinging segment and another finger tip on the spinous process of each adjacent segment (above and below). If the subject is unable to prevent flexion at this segment the therapist palpates uncontrolled opening (spinous processes moving apart). 1. Place one finger tip on the spinous process of the primary hinging segment. During normal extension the spinous process can be palpated moving slightly forwards (as the articular surfaces close and compress), then the spinous process is palpated moving backwards and down as the articular surface of the upper segment glides backwards on the lower segment. If the subject is unable to prevent extension or translation shear at this segment the therapist palpates uncontrolled and excessive forward displacement of the spinous process during active extension (spinous process moving forwards too far) and a lack of sufficient backward glide. 2. Place one finger tip on the spinous process of the primary hinging segment and another finger tip on the spinous process of each adjacent segment (above and below). If the subject is unable to prevent extension at this segment the therapist palpates uncontrolled closing (spinous processes moving together) during lumbar spine extension. A multisegmental hyperflexion can be identified in motion testing in the following ways: 1. Observe or palpate the multisegmental group of spinal segments (e.g. whole lumbar lordosis L1–S1). The therapist relies on visual observation or manual palpation to identify if the subject cannot maintain a neutral lordosis and prevent flexion during the test movement. The subject demonstrates a decrease in the depth or flattening or reversal of the lordosis curve when instructed to prevent flexion. 2. Place a long piece of adhesive strapping tape across the entire group of spinal segments (e.g. whole lumbar lordosis L1–S1). The skin is tensioned from the lowermost segment (below) to the uppermost segment. If the subject cannot prevent flexion across this multisegmental group, the tape pulls off the skin when uncontrolled flexion motion is produced. A multisegmental hyperextension can be identified in motion testing in the following ways: 1. Observe or palpate the multisegmental group of spinal segments (e.g. whole lumbar lordosis L1–S1). The therapist relies on visual observation or manual palpation to identify if the subject cannot maintain a neutral lordosis and prevent extension during the test movement. The subject demonstrates an increase in the depth or exaggeration of the lordosis curve when instructed to prevent extension. 2. Place a long piece of adhesive strapping tape across the anterior abdomen (e.g. from the ASIS (anterior superior iliac spine) to the lower anterolateral ribcage or along the rectus abdominis muscle). The skin is tensioned from the lowermost attachment (below) to the uppermost attachment. If the subject cannot prevent spinal extension or anterior pelvic tilt across this multisegmental group, the tape pulls off the skin when uncontrolled extension motion is produced. Occasionally, both single segment and multisegmental dysfunctions can present together. • segmental extension hinge – uncontrolled segmental extension and translational shear at a pivot point (primarily at L5–S1, but potentially also at L3–4–5) • multisegmental hyperextension – uncontrolled lumbar hyperextension and exaggerated anterior tilt. The relationship between SIJ or pelvic girdle pain and insufficiencies in the stability of the lumbopelvic region is currently an active area of research (Hungerford et al 2003; Stuge et al 2004; O’Sullivan & Beales 2007b). The classification of UCM in terms of site and direction at the SIJ and pelvis is gaining recognition and reports of labelling movement and positional faults can be seen in the literature (Cibulka 2002). The range of motion that is available to the SIJ is very small in terms of translation and rotation between the sacrum and the innominates. Reports vary, but it is generally accepted that there are approximately 2–6° of rotation and 2 mm of translation (Sturesson et al 1989; Bogduk 1997; Lee 2004). These small ranges of motion are only able to be measured with specialised radiographic techniques (Sturesson et al 1989). Consequently, it is not possible to visually measure this range of motion and therefore not reliable to evaluate the site and direction of sacroiliac motion visually. Aberrant motor control strategies have been identified in people with SIJ and pelvic pain. O’Sullivan et al (2002b) observed abnormal kinematics of the diaphragm and pelvic floor during an active straight leg raise test in subjects with SIJ pain, and noted that these aberrant motor control strategies could be eliminated with manual compression during the test. In addition, these people demonstrated bracing strategies in the abdominal wall not seen in the non-pain group. Transversus abdominis recruitment has been shown to increase SIJ stiffness to a significantly greater degree than the general abdominal exercise pattern, illustrating the stability role that this muscle has on the SIJ (Richardson et al 2002). Evaluation of the presence of SIJ dysfunction has historically been difficult to evaluate (Riddle & Freburger 2002). Laslett et al (2005) have demonstrated that composites of provocation tests are of value in clinical diagnosis of the symptomatic SIJ but do not evaluate movement faults or guide diagnosis. Some authors have reconsidered the influence on force closure but not detailed specific assessment of movement faults (Pool-Goudzwaard 1998). O’Sullivan & Beales (2007a) have recognised that movement faults can be a part of SIJ dysfunction but do not detail the site and direction of UCM. Altered motor control strategies and alteration of respiratory function have been identified in subjects with sacroiliac pain (O’Sullivan & Beales 2007a). Hungerford et al (2003) have indentified delayed onset of internal oblique, multifidus and gluteus maximus on the supporting leg during hip flexion in subjects with SIJ changes, which they consider evidence of altered lumbopelvic control. Muscle recruitment dysfunction has been shown to be reversible: an individualised specific exercise training program has been shown to be more effective than physical therapy for women with pelvic girdle pain after pregnancy (Stuge et al 2004). Although research has demonstrated the presence of movement faults in subjects with SIJ or pelvic girdle pain (Mens et al 2002; Hungerford et al 2004) reliability and validity of clinical tests are lacking. However, Hungerford et al (2007) have shown that physical therapists can reliably palpate and recognise altered patterns of intra-pelvic motion with a weight shift from bilateral stance to unilateral hip flexion. The osteopathic process of positional diagnosis, as advocated by Mitchell et al (1979) and Greenman (2003), uses manual palpation of the pelvis during functional movement testing to determine motion restriction of the SIJ. There is a lack of consensus among the clinicians who use this approach as to which motion tests identify restriction in function and as to precisely where to palpate the pelvis to interpret the positional change of adaptation. Once the restriction is determined as being related to abnormal motion of the sacrum, the right innominate or the left innominate, palpation of pelvic landmarks is then used to determine the position of adaptive change. This process of positional diagnosis attempts to identify and label the site and direction of adaptive compensatory motion of the pelvis. The site and direction of adaptive compensatory motion appears to be related to the site and direction of UCM. The process of positional diagnosis currently labels three separate sites of pelvic girdle adaptation: i) the sacrum; ii) the innominate; and iii) the pubis. These three sites also demonstrate specific directions of adaptive compensation or UCM (Table 5.3). Table 5.3 Potential site and direction of UCM in the pelvic girdle The subject is instructed to stand with the feet in a natural stance and bend forwards in a normal relaxed pattern. Ideally, there should be even flexion throughout the lumbar and thoracic regions with the hips flexing to approximately 70°. The spinal flexion and hip flexion should occur concurrently. The finger tips should reach the floor without the need to bend the knees (Figure 5.1). There should be good symmetry of movement without any lateral deviation, tilt or rotation of the trunk or pelvis. The pelvis and hips should lead the return to standing with the spine unrolling on the way back to the upright posture. • Hamstrings restriction of hip flexion – the hips lack 70° of normal range in standing forward bending. The lumbar spine frequently increases flexion to compensate for the lack of hip mobility. Hamstring extensibility can be tested passively and dynamically with manual muscle extensibility examination. • Thoracic restriction of flexion – mid and upper thoracic flexion restriction may also contribute to compensatory increases in lumbar flexion range. This is confirmed with manual segmental assessment (e.g. Maitland passive physiological intervertebral movements or passive accessory intervertebral movements) (Maitland et al 2005). • Lumbar flexion – the lumbar spine may initiate the movement into flexion and contribute more to producing forward bending while the hips and thoracic contributions start later and contribute less. At the limit of forward bending, excessive or hypermobile range of lumbar flexion may be observed. During the return to neutral the lumbar flexion and posterior pelvic tilt persists and unrolls late. • Segmental flexion hinge. If only one spinous process is observed as prominent and protruding ‘out of line’ compared to the other vertebrae then the UCM is interpreted as a segmental flexion hinge. The specific hinging segment should be noted and recorded. This commonly occurs at the L5–S1 segment. Ideally, when lumbar flexion control is assessed, the positional alignment between the low lumbar spine and the pelvis should be maintained during hip flexion or thoracic flexion challenges. If lumbopelvic stability and control is inadequate, L5 alignment with the sacrum cannot be maintained and during flexion control tests the L5 and S1 segments appear to ‘open’ (the spinous processes move apart) as the pelvis posteriorly tilts instead of moving forwards with the spinal position. The upper lumbar lordosis can be maintained well and the failure of control is demonstrated only at the lumbopelvic junction. • Multisegmental hyperflexion. If, on the other hand, excessive or hypermobile lumbar flexion is observed, but no one particular spinous process is prominent from the adjacent vertebrae then the UCM is interpreted as a multisegmental hyperflexion. This is commonly observed as excessive reversal of the lumbar lordosis and hypermobile flexion of the whole lumbar region. Instead of maintaining positional control of the lumbar lordosis and the pelvis during hip flexion or thoracic flexion challenges, uncontrolled lumbar flexion and posterior pelvic tilt are observed. The person should have the ability to actively lean forwards by flexing at the hips while controlling the lumbar spine and pelvis. The person stands tall with legs straight and the lumbar spine and pelvis positioned in neutral (Figure 5.2). Lumbopelvic motion is monitored by the therapist. The therapist monitors the lumbosacral neutral position by palpating the spinous process of L2, L5, and S2 with their finger tips (Figure 5.3). During testing, if the palpating fingers do not move, the lumbosacral region is able to maintain neutral (Figure 5.4). If the palpating fingers move further apart, uncontrolled segmental lumbar flexion is identified. The person is instructed to stand tall and to ‘bow’ or lean the trunk forwards from the hips, keeping the back straight (neutral spine). Ideally, the subject should have the ability to dissociate the lumbar spine from hip flexion as evidenced by 50° forward lean while preventing lumbar flexion or posterior pelvic tilt (Figure 5.5). This test should be performed without any feedback (self-palpation, vision, tape, etc.) or cueing for correction. The person stands tall with legs straight and the lumbar spine and pelvis positioned in the neutral. They monitor the lumbosacral neutral position by palpating the spinous process of L2, L5, and S2 with their fingers (Figure 5.6). The person is instructed to stand tall and to ‘bow’ or lean the trunk forwards from the hips, keeping the back straight (neutral spine). If the palpating fingers do not move further apart, lumbar flexion is being controlled (Figure 5.7). The person should self-monitor the lumbopelvic alignment and control with a variety of feedback options (T1.3). In some cases it may be useful to tension a strip of adhesive sports strapping tape to the skin across the uncontrolled segments. This will provide sensory feedback and some degree of mechanical support to the control of flexion. Visual feedback (e.g. observation in a mirror) is also a useful retraining tool. Ideally, the subject should have the ability to dissociate the lumbar spine from hip flexion as evidenced by 50° forward lean while preventing lumbar flexion or posterior pelvic tilt. There should be no provocation of any symptoms under flexion load, within the range that the flexion UCM can be controlled. T1.3 Feedback tools to monitor retraining If control is poor, the pattern of forward leaning with a straight back and independent hip flexion should be performed only as far as lumbar flexion and posterior pelvic tilt can be actively controlled or prevented. Also, the upper body and trunk weight can be supported by weight bearing through the arms to decrease the load that must be controlled by the local and global stabiliser muscles (Figure 5.8). As the ability to control the UCM gets easier and the pattern of dissociation feels less unnatural, the exercise can be progressed to the unsupported position. This exercise can also be performed with the knees bent to decrease the influence of the hamstrings and to encourage the gluteal muscles to eccentrically control the hip. Once the pattern of dissociation is efficient and feels familiar it should be integrated into various functional postures and positions. The person should have the ability to actively push the body away with the hands while leaning forwards by flexing at the hips and controlling the lumbar spine and pelvis. The person positions themselves in 4 point kneeling (hands and knees) with the lumbar spine and pelvis in neutral alignment (Figure 5.9). Lumbopelvic motion is monitored by the therapist. The therapist monitors the lumbosacral neutral position by palpating the spinous process of L2, L5, and S2 with their fingertips (Figure 5.10). Ideally, the person should have the ability to dissociate the lumbar spine and pelvis from hip flexion as evidenced by 120° of hip flexion during the backward push while preventing lumbar flexion or posterior pelvic tilt (Figure 5.11). After 120° hip flexion the pelvis should start to tilt posteriorly and the spine should start to flex as the pelvis moves towards the heels. The lumbar spine and pelvis should return to a neutral position as the subject rocks forwards, back to the starting position. The pelvis should have good symmetry. That is, no lateral tilt or rotation. This test should be performed without any feedback (self-palpation, vision, tape, etc.) or cueing for correction. The person positions themselves in 4 point kneeling (hands and knees) with the lumbar spine and pelvis in neutral alignment. The person rocks backwards from the pelvis towards their heels by pushing with the hands. The goal is to push the pelvis backwards with independent hip flexion, but only as far as the neutral lumbopelvic position can be maintained. Ideally, the person should have the ability to dissociate the lumbopelvic region from hip flexion as evidenced by 120° of hip flexion as the pelvis moves backwards (half way back towards the heels) (Figure 5.12) while preventing lumbar flexion or posterior pelvic tilt. The person should self-monitor the lumbopelvic alignment and control with a variety of feedback options (T2.3). It is very useful to tension a strip of adhesive sports strapping tape to the skin across the uncontrolled segments. This will provide sensory feedback and some degree of mechanical support to the control of flexion. Visual feedback (e.g. observation in a mirror) is also a useful retraining tool. T2.3 Feedback tools to monitor retraining The person should have the ability to lift both feet off the floor (in crook lying) by flexing at the hips and controlling the lumbar spine and pelvis. The person lies on the back in crook lying (hips and knees bent and feet resting on the floor) with the lumbar spine and pelvis relaxed in neutral alignment (Figure 5.13). Lumbopelvic motion is monitored by the placement of a Pressure Biofeedback Unit (PBU) (Stabilizer – Chattanooga) under the back, centred at L3 in the middle of the lumbar lordosis (Figures 5.14 and 5.15). During limb load tests and exercises the PBU can objectively monitor the functional stability of the trunk (Richardson et al 1992, Jull et al 1993). In crook lying the PBU is inflated to a base pressure of 40 mmHg (Figure 5.16). This pressure is used to position and support the lumbar spine in neutral alignment. Under functional limb load or movement, no pressure change = no loss of neutral position = good control. If the lumbar spine flexes beyond the neutral starting position an increase in pressure is registered by the PBU. If the lumbar spine extends beyond the neutral starting position a decrease in pressure is registered by the PBU. The person is instructed to slowly lift both feet off the floor (both at the same time) until both hips are flexed to 90°. They are instructed to keep the knees bent and the lumbar spine neutral (no pressure change) while they flex the hips to 90° by lifting the feet from the floor. They are required to hold this position (Figure 5.17) and keep the back stable (no pressure change) for at least 5 seconds. Ideally, the person should have the ability to dissociate the lumbar spine and pelvis from hip flexion as evidenced by 90° of bilateral hip flexion during the double leg lift while preventing lumbar flexion or posterior pelvic tilt.
The lumbopelvic region
Introduction
Changes in movement and postural control in the lumbopelvic region
Reliability of movement observation
Efficacy of treatment to retrain control of lumbopelvic UCM
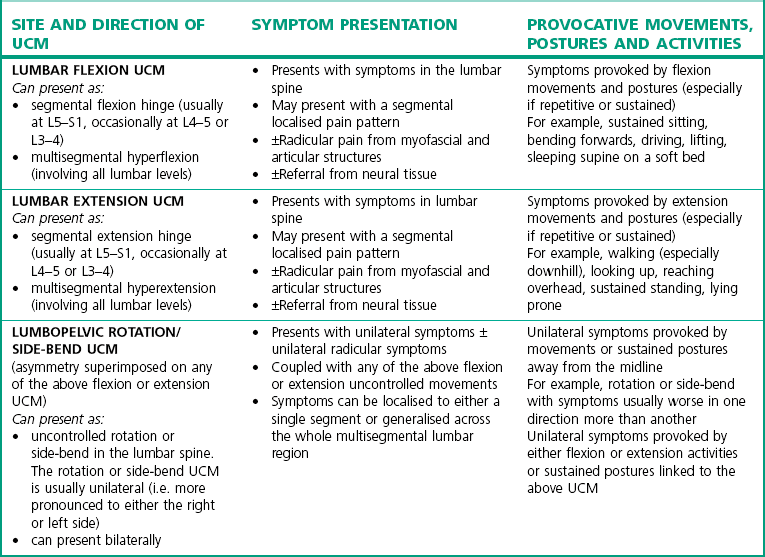
Diagnosis of the site and direction of UCM in the lumbar spine
Identifying site and direction of UCM at the lumbar spine
Segmental and multi-segmental uncontrolled motion in the sagittal plane
Segmental UCM
Multisegmental UCM
Clinical examples
Lumbar extension UCM
Movement and postural control at the sacroiliac joint (SIJ) and pelvis
Identifying UCM at the SIJ and pelvis
SITE
DIRECTION
Forward torsion
Sacrum
Backward torsion
Nutated and side-bent (unilateral flexion)
Counternutated and side-bent (unilateral extension)
Anterior rotation
Innominate
Posterior rotation
Superior shear (upslip)
Inferior shear (downslip)
Inflare
Outflare
Superior shear
Pubis
Inferior shear
Anterior shear
Posterior shear
Lumbar flexion control
Observation and analysis of lumbar flexion and forward bending
Description of ideal pattern
Movement faults associated with lumbar flexion
Relative stiffness (restrictions)
Relative flexibility (potential UCM)
Tests of lumbar flexion control
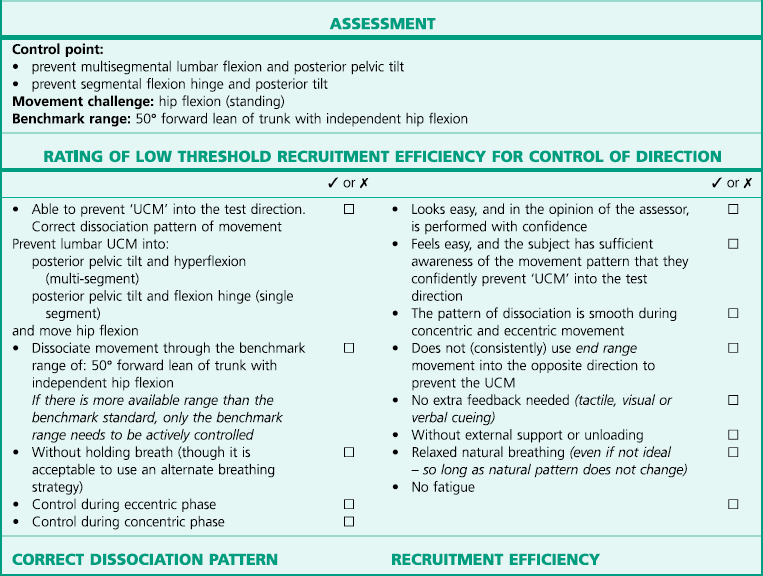
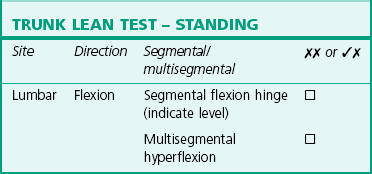
T1 Standing: trunk lean test(tests for lumbar flexion UCM)
Test procedure
Rating and diagnosis of lumbar flexion UCM
Correction
FEEDBACK TOOL
PROCESS
Self-palpation
Palpation monitoring of joint position
Visual observation
Observe in a mirror or directly watch the movement
Adhesive tape
Skin tension for tactile feedback
Cueing and verbal correction
Listen to feedback from another observer
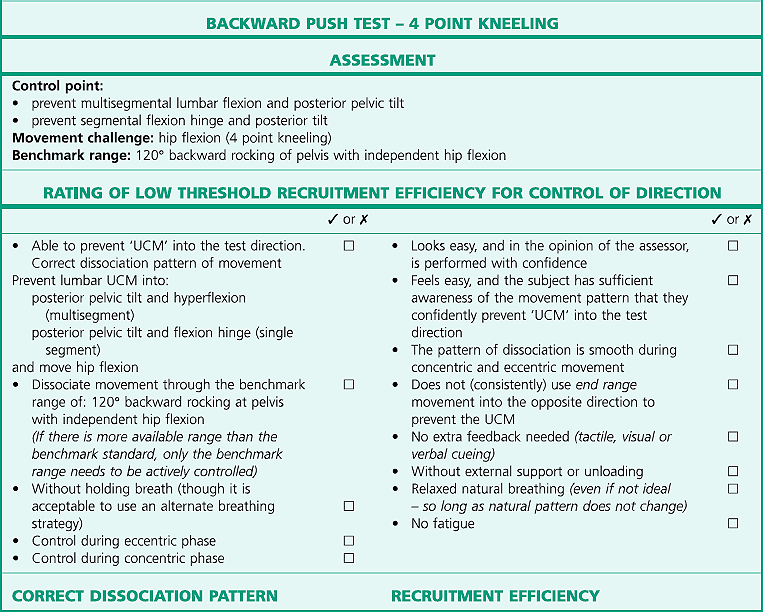
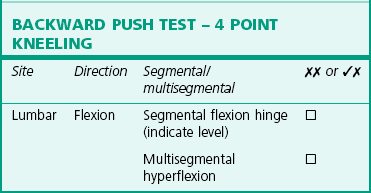
T2 4 point: backward push test(tests for lumbar flexion UCM)
Test procedure
Rating and diagnosis of lumbar flexion UCM
Correction
FEEDBACK TOOL
PROCESS
Self-palpation
Palpation monitoring of joint position
Visual observation
Observe in a mirror or directly watch the movement
Adhesive tape
Skin tension for tactile feedback
Cueing and verbal correction
Listen to feedback from another observer
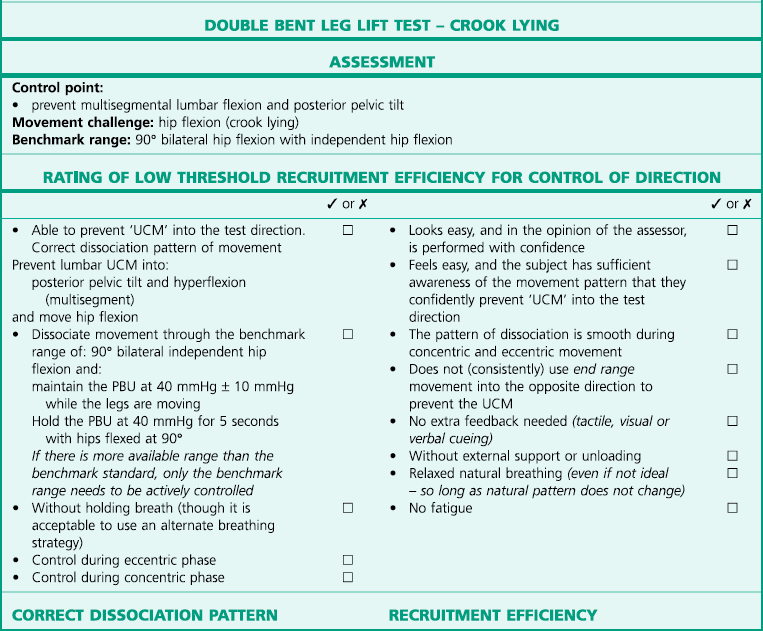
T3 Crook: double bent leg lift test(tests for lumbar flexion UCM)
Test procedure



 (good control of site and direction)
(good control of site and direction)
 (inefficient control of site and direction)
(inefficient control of site and direction)
 (uncontrolled site and direction).
(uncontrolled site and direction).
 rating, the person must demonstrate good control to the benchmark standard and the test movement must look and feel easy and does not require any specific movement retraining. An assessment rating of
rating, the person must demonstrate good control to the benchmark standard and the test movement must look and feel easy and does not require any specific movement retraining. An assessment rating of 
 or
or 
 for any particular test identifies the presence of UCM. The UCM is always qualified by a diagnostic label of its site and direction.
for any particular test identifies the presence of UCM. The UCM is always qualified by a diagnostic label of its site and direction.
 rating for the test. For example, if during a test of control of lumbar flexion control, the lumbar spine moves into extension, there is a possibility of a problem with lumbar extension control. The ability to control this potential UCM should be specifically assessed with extension related tests. However, if there was no UCM into flexion, then flexion is not the direction of UCM and the flexion control test should be rated as
rating for the test. For example, if during a test of control of lumbar flexion control, the lumbar spine moves into extension, there is a possibility of a problem with lumbar extension control. The ability to control this potential UCM should be specifically assessed with extension related tests. However, if there was no UCM into flexion, then flexion is not the direction of UCM and the flexion control test should be rated as 
 .
.
 .
.
 rating or
rating or 
 rating labels or diagnoses the stability dysfunction. The diagnosis should label both the SITE and the DIRECTION of give that is uncontrolled.
rating labels or diagnoses the stability dysfunction. The diagnosis should label both the SITE and the DIRECTION of give that is uncontrolled.