The Knee 
The knee is a pivotal hinge joint, which connects the bones of the upper and lower leg, and allows flexion and extension, as well as limited medial and lateral rotation. It is stabilized by a complex arrangement of ligaments, tendons and muscles.
The knee is arbitrarily divided into medial and lateral compartments, in which the medial and the lateral femoral condyles articulate with the respective articular surfaces of the tibial plateau, and patellofemoral compartment, in which the patella articulates with the femoral trochlea. The three compartments share a common joint capsule, composed of a strong outer fibrous layer, with local thickenings, which form ligaments, and a thin inner synovial membrane. Superiorly, the capsule attaches to the femur, immediately proximal to the articular margins of the condyles, and inferiorly on the tibia, distal to the cartilage. Anteriorly, the synovial membrane is separated from the capsule, which attaches to the patella and lines the posterior surface of infrapatellar fat pad. The synovial membrane extends posteriorly through the joint space and surrounds the two cruciate ligaments, rendering them extrasynovial. Posteriorly, the capsule attaches at the cartilaginous margins of the femoral condyles. The capsule is deficient on the lateral condyle, allowing the popliteus tendon to exit the joint.
Figures 1 to 6 show the normal MR appearance of important knee joint structures. A systematic image analysis and structured reporting is prudent for optimal diagnostic assessment of the knee structures. This chapter discusses the imaging evaluation approach and describes how to fill in the structured checklist (Box 1). Conceptual details of related MR physics and imaging protocol are discussed in the chapter on MR protocol optimization.
 IMAGE EVALUATION
IMAGE EVALUATION
The below-outlined stepwise interpretation approach is only a practical guide, and all structures of the knee should be evaluated in multiple planes for optimal assessment. This will also help readers perceive which structures are best depicted/evaluated in which particular plane.
1. Line up the similar-plane fat-saturated (fs) and non-fs images and synchronize them for tandem evaluation.
2. Start with the sagittal and axial images to look for possible knee effusion or Baker cyst. Check on sagittal and coronal images for marrow abnormalities, such as red marrow reconversion, fracture, contusion, or mass lesion. Subsequently, check for cartilaginous or osteochondral bodies and assess the bony alignment.
3. For the internal structures, use coronal and sagittal images. Coronal images are useful for assessing free edge abnormalities of the meniscal bodies, evaluating the anterior and posterior meniscal roots, and detecting displaced flap or bucket-handle components of meniscal tears. The anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) are also best seen on coronal images and different bundles can be outlined. Anterior-most coronal images show patellofemoral cartilage erosion-related marrow abnormalities, whereas posterior most images are good for detecting Baker cyst rupture-related fluid leakage and the popliteal neurovascular bundle. Mid-coronal images are useful for the evaluation of the medial collateral ligament (MCL) complex and lateral collateral ligament (LCL) complex.
4. Sagittal images are useful for secondary look at the meniscal horns and roots. The normal ACL should parallel the roof of the intercondylar notch (Blumensaat line) on these images. All fat pads are well evaluated on sagittal images and secondarily on axial images, including Hoffa’s, quadriceps, and prefemoral fat pads. Synovial thickening, debris, bodies, and abnormality of plicae are also well seen on these images. The posterior joint capsule, patellar tendon, quadriceps tendon, and semimembranosus (especially the pars distalis) tears are nicely seen on sagittal images. Finally, sagittal images are essential for establishing patella alta and abnormal tibial translation.
5. Axial images are useful for the evaluation of patellofemoral malalignments (tilt and subluxation). While coronal and sagittal images are ideal for tibiofemoral articuar cartilage (coronal and sagittal both) and trochlear cartilage (sagittal images), axial images are ideal for evaluation of the cartilage of patella and apex of the trochlear sulcus. Capsular thickenings of anterior and posterior knee (including the medial and lateral retinaculae, medial and LCLs, posterior oblique ligament, oblique popliteal ligament, and arcuate ligament) are best seen on the axial images. Finally, the axial images are optimal for assessing the gastrocnemius, popliteus, pesanserinus and semimembranosus tendons, muscles, 2nd look at the collateral and cruciate ligaments, regional mass lesions and evaluation of the neurovascular bundles.
 BOX 1: The Structured Report: Knee
BOX 1: The Structured Report: Knee
The checklist for structured reporting of MR imaging of the knee. For each field, Normal is considered default in the dictation whereas the rest of the elements describe various pathologies that could be encountered during imaging evaluation. See Appendices 1 and 2 at the end of the chapter for a sample completed reports of normal and abnormal examination results.
EXAMINATION: MRI OF THE [RIGHT/LEFT] KNEE [WITH/WITHOUT] CONTRAST
FINDINGS:
Fluid: [<Normal> <Small effusion> <Moderate effusion> <Large effusion> <Baker cyst (present / partially ruptured)> <Synovial hypertrophy> <Cartilaginous or osteochondral bodies>]
Medial compartment:
Medial meniscus: [<Normal> <Degenerative free edge fraying> <Incomplete or complete radial tear/Oblique tear/Horizontal tear/Longitudinal tear/Flap tear/Displaced bucket-handle tear>]
Medial collateral ligament: [<Normal> <Thickened> <Acute sprain>]
Medial femoral condyle cartilage: [<Normal>]
Medial tibial plateau cartilage: [<Normal>]
Posteromedial corner:
Semimembranosus tendon: [<Normal> <Tendinosis> <Tear>]
Posterior oblique ligament: [<Intact> <Acute Sprain>]
Lateral compartment:
Lateral meniscus: [<Normal> <Degenerative free edge fraying> <Incomplete or complete radial tear/Oblique tear/Horizontal tear/Longitudinal tear/Flap tear/Displaced bucket-handle tear>]
Lateral collateral ligament: [<Normal> <Thickened> <Acute sprain>]
Lateral femoral condyle cartilage: [<Normal>]
Lateral tibial plateau cartilage: [<Normal>]
Posterolateral corner:
Popliteus tendon: [<Normal> <Tendinosis> <Partial tear>]
Popliteofibular ligament: [<Intact> <Acute sprain>]
Arcuate ligament: [<Intact> <Acute sprain>]
Proximal tibiofibular joint: [<Normal> <Osteoarthrosis> <Effusion>]
Anterior compartment:
Alignment: [<Normal> <Patella alta/Patella infera> <Patellar tilt> <Lateral/Medial patellar subluxation>]
Quadriceps tendon: [<Normal> <Tendinosis> <Tear> <Enthesopathy> <Quadriceps fat pad edema/Prefemoral fat pad edema>]
Patellar tendon: [<Normal> <Tendinosis> <Tear> <Enthesopathy>]
Patellar cartilage: [<Normal>]
Trochlear groove: [<Normal> <Shallow> <Prominent lateral ridge>]
Trochlear cartilage: [<Normal>]
Plica: [<Normal / Thickened> <Sprained ligamentum mucosum>]
Hoffa fat pad: [<Normal> <Superolateral edema> <Shearing injury>]
TT–TG distance: [__] cm
Intercondylar compartment:
Anterior cruciate ligament: [<Normal> <Mucoid degeneration> <Sprain>]
Posterior cruciate ligament: [<Normal> <Mucoid degeneration> <Sprain>]
Bones: [<Otherwise normal>]
Muscles: [<Normal>]
Vessels: [<Normal>]
Nerves: [<Normal>]
Other:
IMPRESSION:

Fig. 1: Normal knee MR anatomy. Anterior coronal images (A, B) demonstrate the iliotibial band (arrowheads), 1st layer of the medial collateral ligament (short arrows), superficial (medium arrows) and deep (long arrows) medial collateral ligament, as well as the anteromedial (dashed arrows) and posterolateral (dotted arrows) bundles of the anterior cruciate ligament.
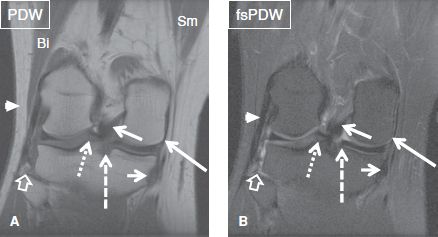
Fig. 2: Normal knee MR anatomy. Posterior coronal images (A, B) show the lateral collateral ligament (arrowheads), popliteofibular ligament (open arrows), posterior oblique ligament (long arrows), posterior cruciate ligament (medium arrows), posterior root of the medial (dashed arrows) and lateral (dotted arrows) meniscus, semimembranosus muscle (Sm), semimembranosus tendon (short arrows) and biceps femoris muscle (Bi).
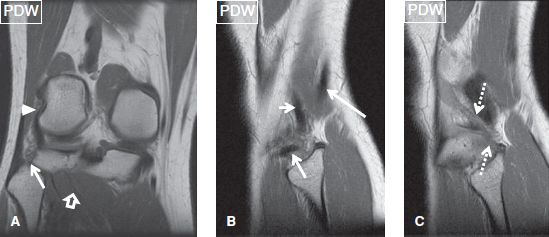
Fig. 3: Normal knee MR anatomy. Posterior coronal (A) and sagittal (B, C) images show the popliteus tendon (arrowhead) and myotendinous junction (open arrow), biceps femoris tendon (long arrow), popliteofibular ligament (medium arrows), lateral collateral ligament (short arrow), and arcuate ligament (dotted arrows) arising from the tip of styloid process.
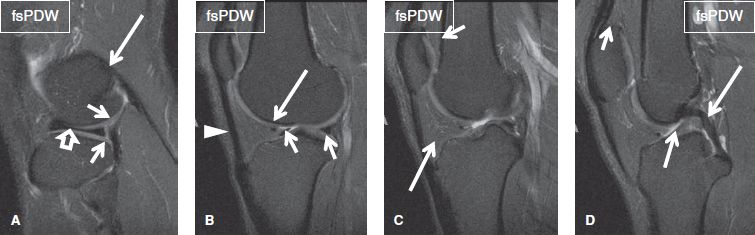
Fig. 4: Normal MR knee anatomy. Sequential lateral sagittal images. A: Open arrow, body of the lateral meniscus; short arrows, superior and inferior popliteomeniscal fasciculi; long arrow, origin of the lateral head of the gastrocnemius muscle. B: Short arrows, anterior and posterior horns of the lateral meniscus; long arrow, transverse meniscal ligament; arrowhead, patellar tendon. C: Long arrow, Hoffa’s fat pad; short arrow, prefemoral fat pad. D: Short arrow, quadriceps fat pad; medium arrow, anterior cruciate ligament; long arrow, posterior cruciate ligament.
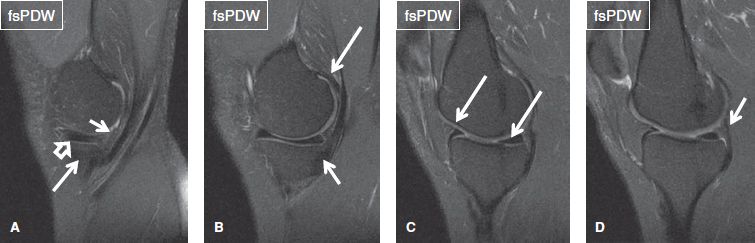
Fig. 5: Normal knee MR anatomy. Sequential medial to sagittal images. A: Open arrow, body of the MM; short arrow, meniscocapsular junction; long arrow, pars reflexa of the semimembranosus tendon. B: Short arrow, pars distalis of the semimembranosus tendon; long arrow, medial head of the gastrocnemius muscle. C: Arrows, anterior and posterior horns of the MM. D: Arrow, posterior oblique ligament and capsular reflection of the semimembranosus tendon.
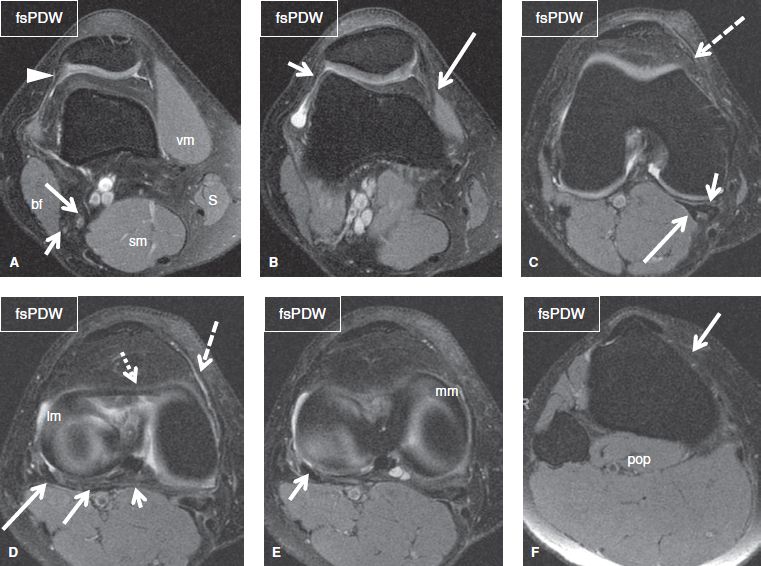
Fig. 6: Normal knee MR anatomy. Sequential axial images. A: Arrowhead, vastus lateralis obliquus; short arrow, common peroneal nerve; long arrow, tibial nerve; vm, vastus medialis muscle; S, sartorius muscle; sm, semimembranosus muscles; bf, biceps femoris muscle. B: Short arrow, lateral patellofemoral ligament; long arrow, medial retinaculum. C: Dashed arrow, medial patellofemoral ligament; short arrow, semimembranosus tendon; long arrow, medial head of the gastrocnemius tendon. D: Dashed arrow, medial patellomeniscal ligament; dotted arrow, transverse meniscal ligament; lm, lateral meniscus; short arrow, oblique popliteal ligament; medium arrow, medial bundle of the arcuate ligament; long arrow, lateral bundle of the arcuate ligament. E: Arrow, popliteus tendon underneath the lateral bundle of the arcuate ligament; mm, medial meniscus. F: Arrow, medial patellotibial ligament; pop, popliteus muscle.
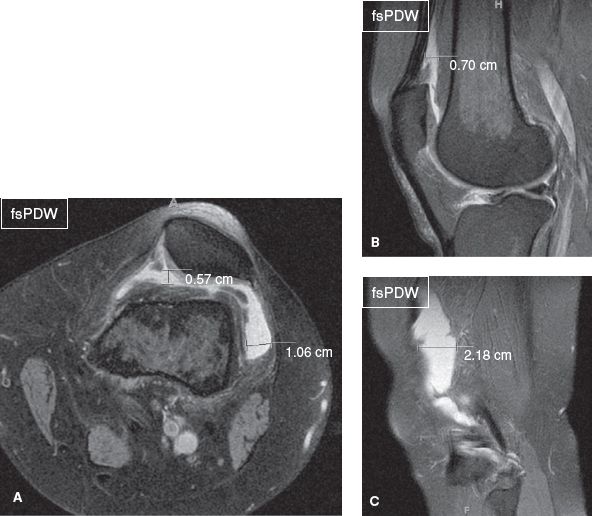
Fig. 7: Small joint effusion. On axial (A) and midsagittal (B) images, the anteroposterior distance of the effusion at its widest point in the midline of the suprapatellar pouch exceeds 5 mm and transverse diameter exceeds 10 mm in the lateral recess. C: On the respective far-lateral sagittal image, the anteroposterior distance of the effusion at its widest point in the lateral aspect of the suprapatellar pouch also exceeds 10 mm.
 HOW TO FILL THE STRUCTURED REPORT
HOW TO FILL THE STRUCTURED REPORT
FLUID: [<Normal> <Small effusion> <Moderate effusion> <Large effusion> <Baker cyst (present / partially ruptured)> <Synovial hypertrophy> <Cartilaginous or osteochondral bodies>]
Typically, effusion in the knee joint first accumulates in the suprapatellar bursa, a potential space, which normally contains minimal amount of fluid. Joint effusion is established on sagittal images when the anteroposterior distance of the effusion at its widest point in the midline of the suprapatellar pouch is more than 5 mm or when the transverse distance of the effusion at its widest point in the lateral recesses on the axial image exceeds 10 mm (Fig. 7). Joint effusion can be graded as small (minimally exceeding the criteria as described), moderate (distending anterior and posterior recesses), and large (substantial distention of all recesses). Additional components, such as fat-fluid level or hematocrit level indicating recent intra-articular fracture, should be identified (Figs. 8, 9). The normal synovium is a thin imperceptible layer. With worsening internal derangement, whether mechanical or inflammatory, it may undergo thickening, with or without associated fibrofatty proliferation of the prefemoral fat pad. Synovial thickening can be graded as mild, moderate, or extensive. The suprapatellar bursa is the most frequent site of lipoma arborescens (villous lipomatous proliferation), a rare benign intra-articular lesion of unknown etiology, which is characterized by diffuse replacement of the subsynovial tissue by mature fat cells. On MR imaging, the entity appears as frond-like proliferation of the synovium, which features fat-like signal on all sequences. Visualization of the fronds is improved in case effusion co-exists. Chemical shift artifact is sometimes evident at the fat–fluid interface on gradient-echo images (Figs. 9, 10). This diagnosis should be made in younger individuals and they may benefit from synovectomy. In older subjects, partial (uni-compartmental) or bicompartmental joint involvement with lipoma arborescence is usually a manifestation of worsening internal derangement.
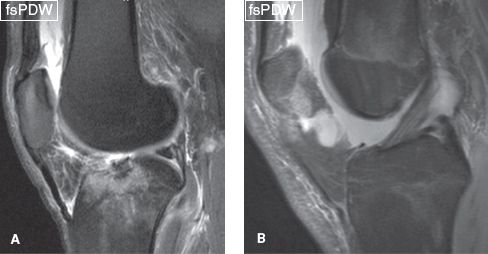
Fig. 8: Moderate and large knee joint effusion. Compared to Figure 7, these sagittal midline images demonstrate increased amount of synovial fluid, corresponding to moderate (A) and large (B) joint effusion.
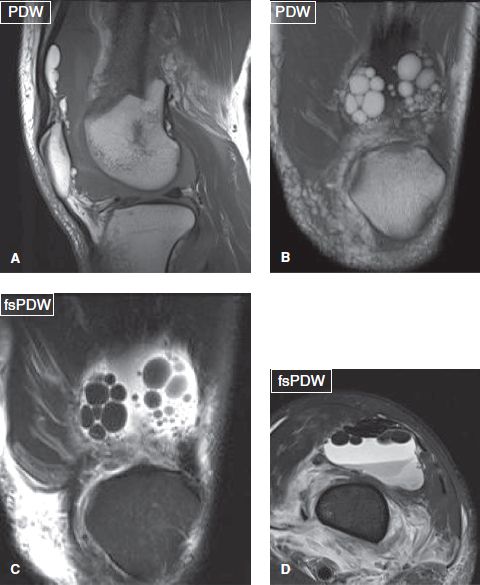
Fig. 9: Moderate lipohaemarthrosis. On sagittal (A), coronal (B, C), and axial (D) images, a femur fracture and lipohaemarthrosis with multiple fat globules can be seen.
The knee is a common location for pigmented villonodular synovitis, in which the synovium is focally or diffusely thickened and features nodularity and low signal on all sequences (even more evident on gradient-echo images related to blooming artifacts) due to hemosiderin deposition. Joint effusion is typically present. The entity is usually mono-articular, involves large joints, and is infrequently associated with bone erosions (Figs. 11–14). Differentiation from hemophilic arthropathy is difficult and is usually based on clinical history (Fig. 15). Other causes of joint hemorrhage include rheumatoid arthritis and prior arthroscopy. Other causes of hypointense synovial thickening or lesions include gout and amyloidosis; however, these entities are predominantly para-articular rather than intra-articular. A thorough search should be performed for intra-articular loose bodies. The latter may be a) cartilaginous, featuring intermediate signal on T1W and PDW images, or b) osteochondral, demonstrating variable signal, depending on the degree of ossification, but usually showing hypointense cortical lining and internal marrow signal. In case one or two bodies are detected, the articular surfaces should be checked for potential donor sites. Multiple loose bodies in the knee are commonly encountered in primary and secondary synovial osteochondromatosis (Figs. 16, 17). In the primary variety, the bodies are numerous and similar sized with no obvious predisposing pathology or internal derangement. The secondary variety usually affects older individuals with a predisposing underlying cause or internal derangement, such as trauma or arthritis and the bodies are of variable size and fewer in number.
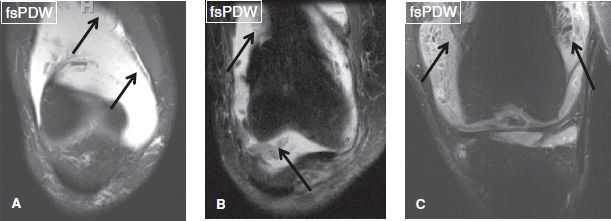
Fig. 10: Synovial thickening. Coronal images from different cases demonstrate mild (A), moderate (B), and severe (C) synovial thickening (arrows). The frond-like projections of the synovium in C are named as lipoma arborescens.
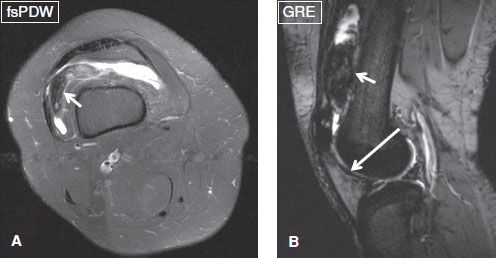
Fig. 11: Pigmented villonodular synovitis. Axial spine echo (A) and sagittal gradient echo (B) images from the same subject demonstrate focal PVNS (short arrows) with blooming artifact on GRE from internal hemorrhages. Notice diffuse hypointensity (long arrow) of the adjacent synovium from hemosiderin lining, a reflection of prior episodes of recurrent hemorrhages.
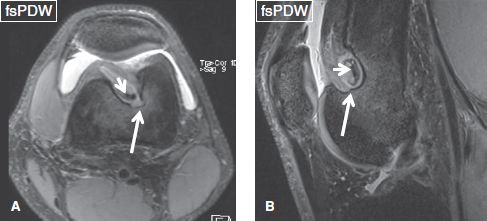
Fig. 12: Pigmented villonodular synovitis. Axial (A) and sagittal (B) images show a large erosion (long arrows) of the femoral metaphysis with bone marrow edema, associated with internal hypointensity (short arrows) within the hypertrophied synovium, a biopsy-proven case of focal PVNS.
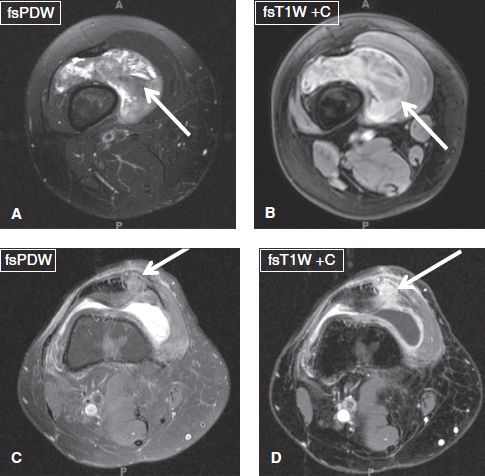
Fig. 13: Diffuse pigmented villonodular synovitis. A, B: Axial images demonstrate diffuse hypointense synovial thickening that enhances on contrast (arrows). C, D: Images obtained after synovectomy show recurrence at the surgical site (arrows).
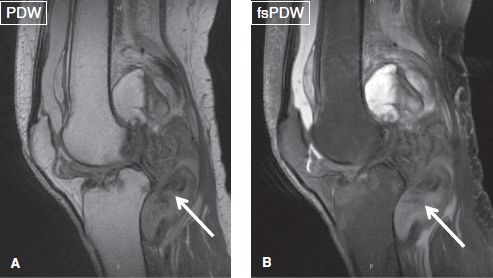
Fig. 14: Diffuse pigmented villonodular synovitis. Sagittal images demonstrate diffuse hypointense synovial thickening (arrows), a biopsy-proven PVNS.
Baker (popliteal) cyst is the most commonly encountered cyst about the knee and is considered a sign of internal derangement or degenerative disease. It is located in the posteromedial aspect of the joint and represents abnormal accumulation of joint fluid within a normally present synovial bursa, which lies between the medial head of the gastrocnemius tendon and the semimembranosus tendon. Typically, uncomplicated Baker cysts have thin low-signal wall and homogeneous high T2 signal intensity and extend in the inferomedial direction, respecting the intermuscular planes. The cysts are qualified as small (<3 cm), moderate (4 to 6 cm), and large (>6 cm) based on the length. Sagittal images demonstrate the extent of the cyst, posterior coronal images show potential leck whereas axial images reveal the cyst’s neck, which is essential for the diagnosis (Fig. 18). Popliteal cysts are asymptomatic but can undergo rupture and dissect along or into adjacent structures, clinically simulating thrombophlebitis. Rupture typically results in edema in the surrounding fascial planes and subcutaneous fat, with fluid tracking inferiorly along the medial side of the medial gastrocnemius muscle plane (Fig. 19). Blood products from intracystic hemorrhage or protein-rich synovial fluid may result in increased signal on T1W images and the cysts can extend variable distances along the knee; however, they can be distinguished from more ominous lesions based on identification of the neck location, multiloculated cystic appearance (usually following multiple prior episodes of rupture and chronicity), and peripheral enhancement on contrast. Uncommonly, popliteal cysts contain debris, loose (cartilaginous or osteochondral) bodies, or pigmented villonodular synovitis (PVNS) (Fig. 20).
MEDIAL COMPARTMENT:
Medial meniscus: [<Normal> <Degenerative free edge fraying> <Incomplete or complete radial tear/Oblique tear/Horizontal tear/Longitudinal tear/Flap tear/Displaced bucket-handle tear>]
Medial collateral ligament: [<Normal> <Thickened> <Acute sprain>]
Medial femoral condyle cartilage: [<Normal>]
Medial tibial plateau cartilage: [<Normal>]
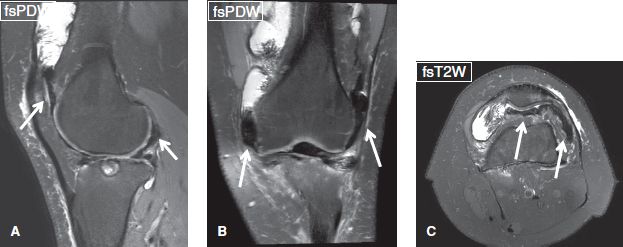
Fig. 15: Hemophilic arthropathy. Sagittal (A), coronal (B), and axial (C) images demonstrate diffuse hypointensity of the synovium (arrows), reflecting hemosiderin deposits due to repeated haemarthrosis.
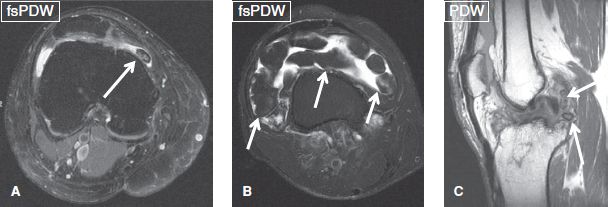
Fig. 16: Loose intra-articular bodies. Axial images. A: A single osteochondral body (arrow) is evident anterior to the medial femoral condyle. B: Multiple osteochondral bodies (arrows) of approximately the similar size are present in the suprapatellar bursa, in this case of primary osteochondromatosis. C: Two osteochondral bodies (arrows) of different size are evident in the posterior aspect of the joint space, in this case of secondary osteochondromatosis. Notice prior ACL graft failure changes.
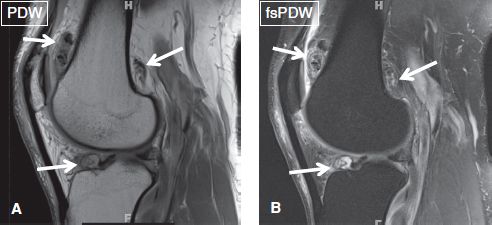
Fig. 17: Secondary osteochondromatosis. Sagittal images (A, B) show multiple intra-articular loose bodies (arrows) of different sizes in the suprapatellar bursa, intercondylar notch, and gastrocnemius recess.
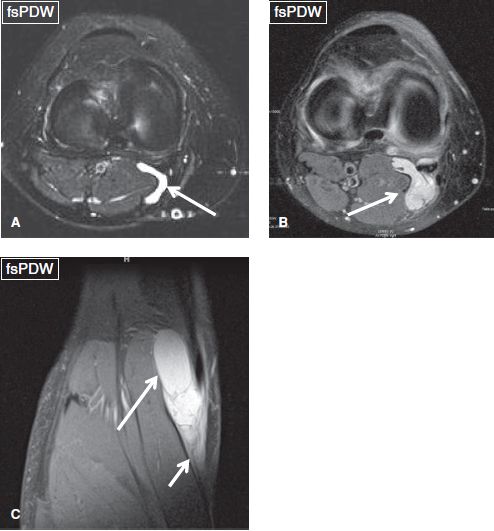
Fig. 18: Baker cyst. Axial (A, B) and coronal (C) images exhibit small, moderate, and large Baker cysts (arrows), respectively. Notice peri-cyst fascial edema and fluid related to recent leak from the cyst in C (short arrow).
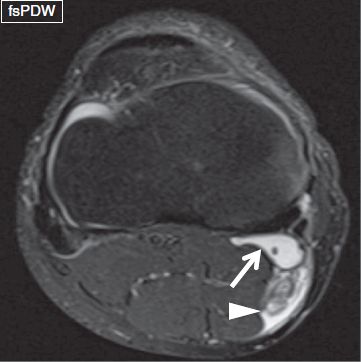
Fig. 19: Ruptured Baker cyst. Axial image shows a small Baker cyst (arrow), with fluid (arrowhead) extending posteriorly beyond the cyst margins and dissecting into adjacent muscles, indicating recent leak/rupture.
The medial meniscus (MM) and the lateral meniscus (LM) are C-shaped fibrocartilaginous structures, which are interposed between the femoral condyles and the tibial plateau. They are composed of type I collagen and encompass 65% to 75% water. The menisci bear 70% of the weight and provide proprioceptive stability, lubrication, cartilage protection, and shock absorption to the joint. Each meniscus consists of an anterior horn, a body, and a posterior horn and is triangular in cross-section, being thicker at the periphery and tapering to a thin free edge centrally. Each meniscus is fixed in the central tibial plateau by anterior and posterior roots, which represent fibers originating from the respective horns. Anteriorly, the menisci are connected via the transverse intermeniscal ligament. The MM is firmly attached to the deep medial collateral ligament (MCL) (aka meniscotibial or coronary ligament) along its entire peripheral circumference. The oblique meniscomeniscal ligament, a normal variant, originates from the anterior horn of one meniscus and inserts into the posterior horn of the contralateral meniscus. Oblique meniscomeniscal ligaments are defined as medial or lateral, based on their anterior origin, and their prevalence is about 3% to 4% (Fig. 21). Unilateral meniscomeniscal ligament is also a known variant, which connects the anterior horn of one meniscus to the posterior horn of the same meniscus. It may lead to formation of what may be called as the ring meniscus variant.
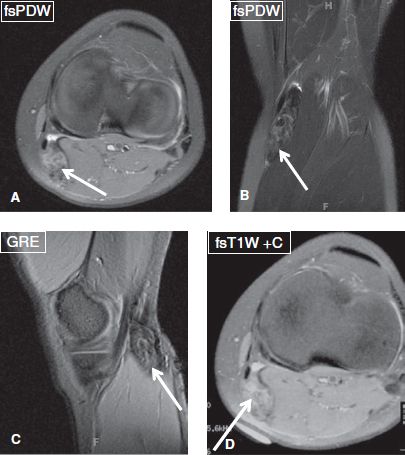
Fig. 20: PVNS localized to a Baker cyst. Axial (A), coronal (B), and sagittal (C) images show Baker cyst filled with hypointense material (arrows) in a biopsy-proven case of PVNS. D: Diffuse contrast enhancement is seen on intravenous gadolinium administration (arrow).
The normal menisci demonstrate smooth margins and uniform low signal on all imaging sequences, except in children and young adults, in whom intermediate or high intrasubstance signal in the periphery may be present, which represents normal vascularity, and should not be interpreted as abnormal. Menisci are best evaluated on non-fs proton density-weighted (PDW) sequences. The latter provide high signal to noise ratio and sharper images. However, fs-PDW provide higher specificity in detecting meniscal tears in post-meniscectomy or meniscal repair cases. Combined examination on sagittal and coronal images is essential, where the normal menisci feature smooth margins and sharp edges. In cross-section, they are triangular, with concave superior surface, flat inferior surface, convex outer curve, and apex pointing to the intercondylar notch. In the sagittal plane, provided that 4- or 5-mm thick slices have been obtained, the two most peripheral images reveal the body of the meniscus, which appears as a bow-tie or an elongated rectangle whereas the three or four more medial images show the opposing triangular shapes of the anterior and posterior horns. The posterior horn of the MM is larger than the anterior horn. As a rule, the anterior horn should never be larger than the posterior.
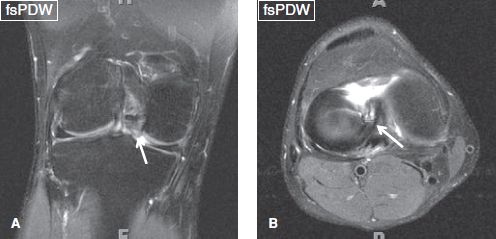
Fig. 21: Medial oblique meniscomeniscal ligament. Coronal (A) and axial (B) images demonstrate a medial oblique meniscomeniscal ligament (arrows), which extends from the anterior horn of the medial meniscus to the posterior horn of the lateral meniscus. Three structures in the intercondylar notch (in addition to normal ACL and PCL) raise the suspicion of a flipped bucket-handle tear, which can be mimicked by this ligament.

Fig. 22: Intrameniscal cyst. Coronal images display well-defined near fluid-like signal (arrow) within the posterior horn of the medial meniscus with minimal expansion.
Meniscal tears are uncommon in individuals younger than 10 years of age. In young adults, the most common mechanism is twisting injury, while in older individuals, meniscus tears result from fall or sudden squatting. The diagnostic criteria used for establishing degeneration and tears of the MM are similar to those of the LM. Clinically, there may be pain (due to inflammation around the tear) or symptoms of locking (relating to flap or bucket-handle tears) and clicking. Assessment of a possible meniscal tear is usually done clinically by locating pain and crepitation along the joint line (most sensitive signs). The palpation for these symptoms must be done while simultaneously applying a valgus or varus stress to the knee at 30 degrees of flexion. Positive findings on clinical exam suggest meniscal tear or an articular cartilage flap.
Provocative pain in the posterior aspect of the knee with maximal flexion is usually indicative of a posterior horn meniscal tear. The McMurray test, also known as the McMurray circumduction test is a rotation test for demonstrating torn meniscus of the knee in a fully flexed position, while hand is placed at the joint line. The MM is tested in external rotation with lateral force (mnemonic mel) while the LM is tested in internal rotation with medial force. A tear in the meniscus may cause a pedunculated tag of the meniscus which may become jammed between the joint surfaces. This would result in a palpable or audible click on extension of the knee. Deep posterior knee pain with squatting is also indicative of a meniscal tear.
MR imaging signs of meniscal degeneration include a) intrasubstance focal or diffuse intermediate signal on all sequences, which does not abut the articular surface, and b) fraying of the free edge, which results from multiple chronic radial microtears, best depicted on coronal images. However, any fluid-like or near fluid-like signal on the fs images warrants closer look at the meniscal surface, since in that case, a tear is likely. If the fluid-like or near-fluid-like signal is relatively well-defined and is associated with some expansion of the meniscus, it is referred to as an intrameniscal cyst (Fig. 22). With three-dimensional (3D) high resolution (0.6 to 0.7 mm isotropic) imaging, many microcysts are seen within the meniscus, which, on two-dimensional (2D) images look like a larger intrameniscal cyst (Fig. 23). Since a radiology consultant is trying to help the orthopod decide whether to go or not to go for surgery and meniscal degenerative changes are so common, it is paramount that one should carefully identify meniscal tears and not spend too much time looking for or deciding whether degenerative changes are present or absent.
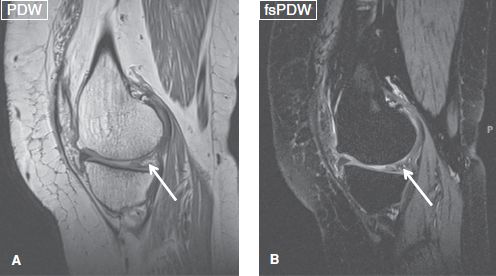
Fig. 23: Intrameniscal microcysts. Sagittal images (A, B) show microcysts within the posterior horn of the medial meniscus (arrows).
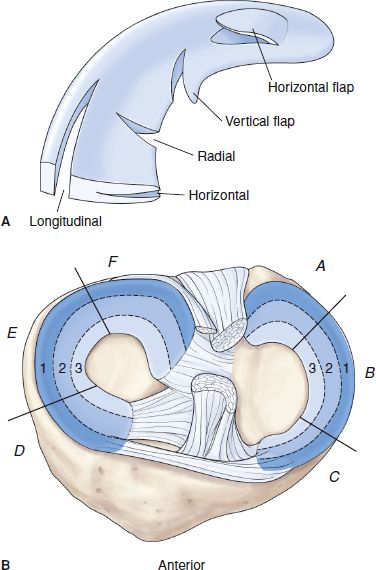
Fig. 24: Classification of meniscal tears as developed by the Knee Documentation Committee of the International Society of Arthroscopy, Knee Surgery and Sports Medicine (ISAKOS). A: Types of tears. B: Location. The meniscal parts are referred to as A, B, or C for one meniscus and D, E, or F for the other meniscus; and 1, 2, and 3 are used for the different layers of the width of the meniscus: the red, pink, and white zones, respectively.
Meniscal tears appear as: a) fluid-like signal or sharp intermediate signal clearly contacting the articular surface on at least one image and/or b) as abnormal morphology of the meniscus. The latter criterion may not apply to menisci which have undergone prior surgery. Tears can involve the anterior horn (or root), the body, or the posterior horn (or root) of the meniscus. Recently, the International Society of Arthroscopy, Knee Surgery, and Sports Medicine (ISAKOS) has made a push for standardization of terminology used for the description of meniscal tears. The Society recommends using the following terminology for different types of tears: radial, longitudinal, horizontal, horizontal flap, and vertical flap; the meniscal parts are referred to as A, B, or C for one meniscus and D, E, or F for the other meniscus; and finally, 1, 2, or 3 for different layers of the width of the meniscus, zone 1 (tears of the meniscosynovial junction or a tear with a rim of less than 3 mm), zone 2 (tears with a rim of 3 to <5 mm), and zone 3 (tears with a rim width of 5 mm or more). The use of the terms red-red, red-white, white-white is discouraged, because of the variable vascular supply of the menisci (Fig. 24). Conceptually, there are simple, complicated and complex tears. Based on shape, simple tears are classified into radial, longitudinal, horizontal, horizontal flap, and vertical flap. Further A and B qualifiers can be added depending upon the tear extends to one surface (incomplete) or both meniscal surfaces (complete). Finally, the committee discourages the use of the terms acute, subacute, and chronic tears.
Radial tears extend from the free edge perpendicularly to the meniscal circumference and appear as cleft on one imaging plane, and as truncation of the free edge on the other. They are characterized as incomplete or complete, based on whether they run through a part or the entire thickness of the meniscus, respectively (Fig. 25). Although radial tears may be small, consequences can be devastating: in acute radial tears, subchondral insufficiency fractures may develop as a result of twisting injury (Fig. 26). On the other hand, these are the most common tears in young adults and develop at points of weakening or change in directionality of meniscal fibers, that is, at the junction of anterior or posterior horn with the body. These progress to oblique (aka parrot beak or coapted flap) tears with increasing age (Fig. 27). In fact, the most common tears in a 40 to 60 year old individuals are oblique tears. The latter may further progress to displaced flaps in the medial (coronary recess) or lateral gutters, with resulting progressive thinning of the opposing articular cartilages over time (Figs. 28, 29). Finally, another type of radial tear is the root tear, which most commonly involves the posterior root of the MM and the anterior root of LM. Associated findings in root tears include subcortical cysts or fatty change (due to prior partial root avulsion), degenerative appearance of the meniscal root and medial extrusion of the meniscal body (Fig. 30). Less commonly, one sees avulsive subcortical linear or flame-shaped bone marrow edema, bony foot plate avulsion, and partial or complete avulsion of the root with medial extrusion of the body and/or insufficiency injury of the overlying femoral or tibial condyles (Figs. 31, 32). With partial tears, it is usually the anterior superior one-third to two-thirds of the root that is affected. The root tear itself is best seen on the sagittal and coronal images while bone marrow changes (cysts and edema) are best seen on the coronal images. One should not mistake these for the bone marrow changes at the PCL tibial attachment. Most times, the PCL-related avulsive changes are usually at the femoral attachment. Sometimes, prominent vessels at the posterior root tibial attachment may mimic these cysts as well; therefore, one should carefully look at the root before overcalling meniscal roots as abnormal. When incomplete, radial tears are one of the worst types of acute tears, as they make the meniscus deficient to tolerate hoop stress. Finally, the readers should be aware that the anatomy dictates the pathologic appearance. Since the MM and LM roots are anatomically different, the appearances of their tears also differ. MM anterior and posterior roots appear as dark uniform bands at the attachment, except on the high resolution images, when a uniform speckled appearance of the roots may be evident. Therefore, it is easy to identify focally increased signal or secondary bony changes, and the diagnosis of tear can be accomplished. On the other hand, the LM evaluation is little more challenging, in the sense that a speckled appearance is pretty common in the anterior root, whereas the posterior root shows two slips of attachment, on either side of the lateral tibial spine (Fig. 33). Therefore, one should carefully look for the individual slips of attachment and associated bony findings before arriving at the diagnosis of root tears. Free edge radial tears can be debrided on surgery while root tears may need repair.
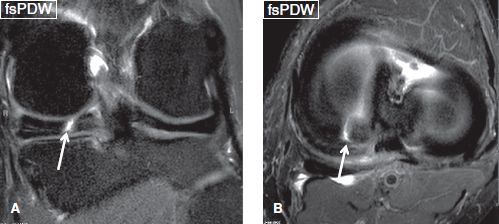
Fig. 25: Radial meniscal tear. Coronal (A) and axial (B) images show fluid-like signal (arrows), which runs perpendicular to the meniscal circumference and traverses nearly its entire thickness. Zone 2 and 3 are involved.
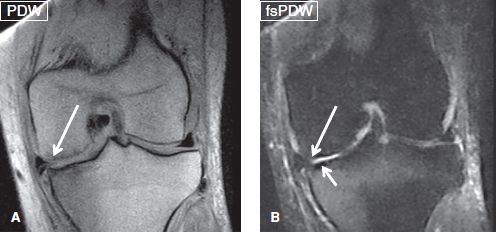
Fig. 26: Incomplete radial tear. Coronal images (A, B) display an incomplete radial tear (long arrows) as truncation of the free edge and extrusion of the body of the medial meniscus. Also note a subchondral insufficiency fracture of the medial tibial plateau (short arrow) with full-thickness cartilage defects.
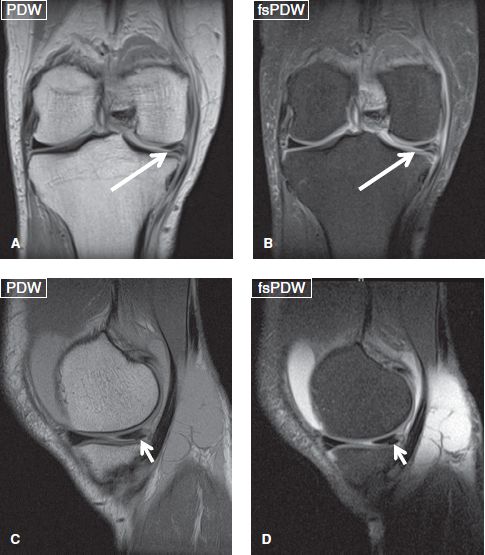
Fig. 27: Oblique (aka parrot beak/coapted flap) meniscal tear. Coronal (A, B) and sagittal (C, D) images demonstrate an oblique tear (arrows) at the junction of body and posterior horn of the medial meniscus, a classic and common location.
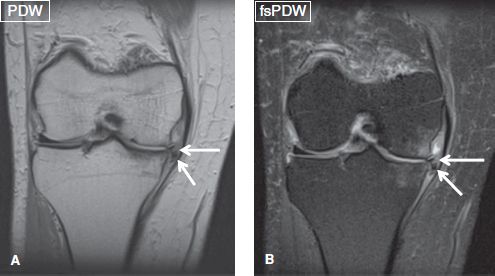
Fig. 28: Displaced flap tear. Coronal images (A, B) show extruded meniscus with a meniscal fragment (arrows) displaced within the coronary recess.

Fig. 29: Displaced flap tear. Sagittal (A) and coronal (B) images demonstrate a superiorly displaced flap tear of the posterior horn of the medial meniscus (long arrows). B: Note avulsive cystic change and bone marrow edema (arrowhead) at the posterior root attachment of the MM from incomplete radial tears and an additional horizontal tear of the posterior horn (short arrow).
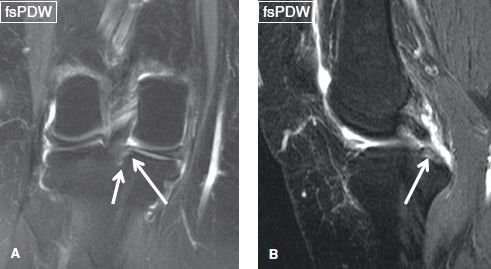
Fig. 30: Incomplete posterior root tear. Coronal (A) and sagittal (B) images exhibit fluid-like signal (long arrows) within the posterior root of the medial meniscus, corresponding to a partial radial/root tear. Also note avulsive cystic change (short arrow) adjacent to the root attachment indicating its subacute nature. Partial tears usually involve anterosuperior one-third to two-thirds of the posterior root.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







