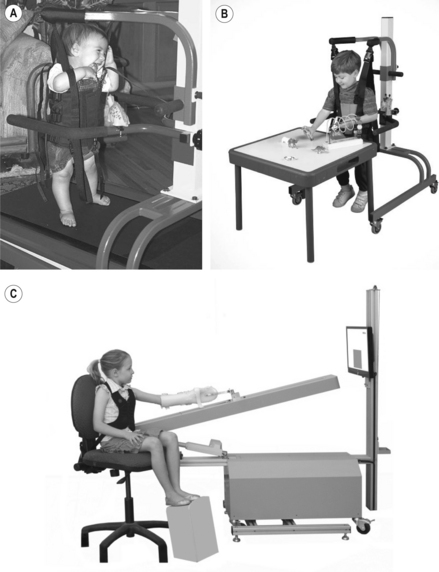
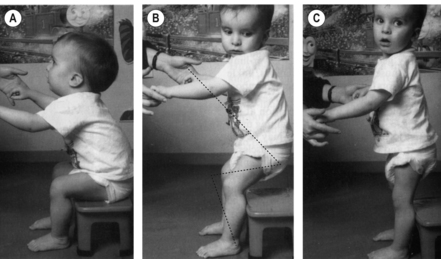
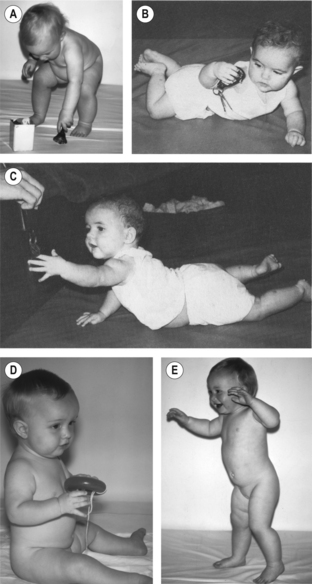
1 This chapter examines some of the issues that are most relevant in a book that argues for early and specifically targeted activity training for infants with cerebral palsy (CP), from earliest infancy to 18 months of age. Early task-oriented training directed at stimulating muscle activation, sensory and motor control processes and motor learning may encourage optimal growth and development, and minimize maladaptive and deforming changes to the neuro-musculoskeletal system. Functional motor performance may, as a result, develop to be more effective and energy efficient. Whether it is possible that augmented and specifically targeted physical activity early in infancy can ameliorate or overcome the effects of the neural lesion is not known, but basing intervention on this hypothesis seems justified at this time given the scientific knowledge available. There is now evidence that targeted training can bring about positive changes in motor behaviour and may therefore be both remedial and preventative (see Garvey et al., 2007). However, development and testing of infant training programmes requires at-risk infants to receive an early referral for intervention. The issues raised in this chapter are discussed in more detail throughout the book. Looking back at the history of intervention in CP it is clear that significant advances have been made over the past half century, at least in countries with well-developed health facilities. However, currently it is evident that therapeutic intervention may start months after birth or later, and that the focus of treatment may still be on decreasing spasticity, stretching contractures and correcting deformity after they have developed, using drug therapy, surgery, splinting and orthoses. When the infant with CP is referred for physical therapy, the emphasis has commonly been on facilitation of movement by the therapist and passive stretching techniques to decrease spasticity. A method of intervention used in many centres is neurodevelopmental or Bobath therapy developed 50 years ago. Its current emphasis is on ‘normalizing’ movement and improving the ‘quality’ of movement, with the therapist facilitating and controlling the infant’s movements. Under these conditions the infant may have little chance to experience his or her own attempts to achieve a goal, little chance of knowing who was responsible for the movement, or learning how to control self-initiated and independent limb and body movement. Learning by trial and error may not be a feature of intervention when the therapist controls the child’s movements. There is little evidence that this form of therapy might be effective−methods are not based on a modern understanding of biomechanics, neuromotor control or learning. New brain imaging methods support the view that the focus in early infancy should be, as it increasingly is in adult neurorehabilitation, on the infant’s own self-initiated activity and on developing methods of driving exploratory, self-initiated and goal- or task-directed movements in an encouraging, challenging environment that allows for intensive practice. Investigations of such programmes are showing promising results (see Chapters 11 to 14; Andersen et al., 2011; Jorgensen et al., 2010) and suggest that such intervention may actually be remedial. Since the 1980s, new developments in rehabilitation after acute brain lesion such as stroke, described in detail in textbooks and journals, have resulted from a contemporary understanding of the sciences related to movement and of the methods by which skill is developed (Carr and Shepherd, 2000, 2010; Magill, 2010; Shumway-Cook and Woollacott, 2011). The areas of particular interest to paediatric professionals, since they provide the theoretical background to clinical practice for children as well as adults, include neuroscience and muscle biology; functional anatomy; biomechanics of motor performance and changes occurring as the child develops and grows; relationships between cognition, vision, tactile sense receptors (such as plantar load receptors) and self-initiated action; the environmental (including gravitational) effects that drive the development of both structure and function; and the methods that drive learning and the acquisition of skills. The neural sciences provide the bases for understanding the mechanisms of neural impairments, but also of adaptability and of learning, two processes that go on through life with positive or negative effects (Kandel et al., 2000). More recently, investigations of factors that influence brain reorganization after a lesion using new imaging and other technologies, investigations of biomechanical changes during motor development and of muscle changes that occur over time are also stimulating the development and testing of new methods of intervention. The results of lesions in the motor system must depend initially on the location and extent of the damage. In infants with CP, specifically those who develop diplegia or hemiplegia, who are the major targets of this book, it seems likely that the major impediments to the development of effective movement in the early months are weakness due to impaired muscle activation and lack of motor control (see Chapter 5). Both can interfere with subsequent development and learning. Both can worsen over time as the infant grows and body weight increases, but also as a result of inactivity, repetitive, stereotypic activity and subsequent maladaptive reorganizational processes. Spasticity (increased sensitivity of stretch receptors) may not play a major role in physical disability in these infants and, since it appears to develop over time, may be related more to changes in the muscles, particularly length-associated changes, than to the brain lesion. There is no evidence that stretch reflex hyperactivity is a major cause of functional disability or that reducing it results in improved functional performance (Rameckers et al., 2008), although there has been little investigation. The presence of spasticity is often assumed, adequate methods of testing it are not always utilized and the nature of what is called spasticity is therefore unclear. Co-contraction is commonly reported in electromyography (EMG) studies of children with CP during actions such as walking. It is a common manifestation of poor motor control – a natural phenomenon that occurs in the able-bodied person in the early stages of learning a new and difficult skill, decreasing as skill level increases (Enoka, 1997). Such co-contraction is also a natural feature of early postnatal development (O’Sullivan et al., 1998). A significant correlation has been reported between muscle weakness and the degree of co-contraction and motor disability (Chae et al., 2002a, 2002b). A decrease in motor unit firing rate results in decreased muscle tension. Additional motor units may be recruited to enable greater force development. Stiffening the lower limb in standing can prevent limb collapse but it may also prevent movement (see Fig. A.2B). Co-contraction can also occur to an excessive degree as a result of prolonged muscle activation, for example, carried over from agonist to antagonist phase in a reciprocal movement such as flexion–extension of the elbow (Kamper and Rymer, 2001). It is possible that development of disabling co-contraction can be minimized by an exercise and training programme designed to train basic actions (see Chapter 11) with emphasis on motor control but also targeting the preservation of the natural length of muscles (Gracies, 2005). Of major significance in CP are the secondary (adaptive) morphological and mechanical adaptations of soft tissues that develop over time, in particular changes in muscle such as diminished extensibility and increased stiffness that must result to some extent from muscle inactivation and/or stereotyped muscle activity. These changes reflect the effects of growth and the level and type of infant activity. Muscle growth and development, including the muscle’s architecture, are seriously affected by inactivation of muscle and disordered contraction patterns since muscle length reflects the muscle’s ‘history’ of movement. Changes occurring to muscle spindle receptors may underlie the development of stretch reflex hyperactivity. Recent advances in the study of muscle changes in children and adults with CP are described in Chapters 4, 6 and 7. Muscle represents a classic biological example of the relationship between structure and function. A muscle’s length reflects the range of lengths it is subject to throughout daily life and is therefore subject to change if our habitual activity changes. Contracture of one muscle group, e.g., hip flexors, can also affect another group, hip internal rotators (Delp et al. 1999). Currently, findings from investigations in two different areas of science, one examining post-lesion brain function, the other muscle adaptation, support the view that what an individual actually does after a brain lesion, i.e., the amount and relevance of physical and mental activity early after the lesion occurs, is important. It is therefore possible to hypothesize that targeted physical and mental activity in earliest infancy might ‘direct’ neural reorganization and motor development. To stimulate from earliest infancy a learning process that leads to enhanced development of motor control requires the training of purposeful and effective movement. Experience in early infancy of active exercise and meaningful use of upper and lower limbs, plus experience of standing upright and weight-bearing through the feet, in actions that actively lengthen muscles known to be prone to contracture, may be critical, not only to the development of balanced movement in a gravitational environment but also to the minimizing of maladaptive changes to muscle resulting from disuse (see Chapter 11). Practice of reach, grasp and manipulation, and of weight-bearing and pushing through the hands, may not only prevent one arm substituting for the other but also prevent the development of muscle contractures. However, the opportunity for early intervention that may be both remedial and preventative can only exist for infants with CP if they are referred in the first few months after birth to the appropriate services, and if those services exist. New methods of intervention are being developed for infants and children with CP, based on a solid foundation in contemporary science and with some evidence of positive effects on motor performance and activity levels. However, there seems a lack of determination to find out whether or not it is possible to prevent or at least minimize the effects of initial impairments and of subsequent maladaptive changes on motor development by early referral to active training programmes in infancy. The focus in literature on CP is on investigation and treatment of established problems: for example, the effects of drug therapy on spasticity. There appears to be little or no focus on primary impairments such as weakness and lack of motor control, or on the development and testing of intensive activity-based programmes, and few investigations into the early history of maladaptive changes in the musculoskeletal system that must occur early in infancy, magnified by bone growth. A recent report from Sweden suggests that calf muscle contracture starts very early in susceptible infants, with the fastest increase before the age of 5−6 years (Hagglund and Wagner, 2011). Our current understanding of the plasticity of the brain and neuromuscular system now provides the stimulus to change the focus in paediatrics to address methods of stimulating neural drive, muscle activation and the processes of learning, and the minimization or prevention of maladaptations (see Chapter 2, Eyre, 2003; Garvey et al., 2007). It is hypothesized, but as yet untested, that maladaptive changes to muscle morphology– architecture, stiffness (viscosity and elasticity) and length, muscle–tendon relationships, muscle spindle sensitivity, and changes to the mechanics of intersegmental and interlimb co-ordination, may be minimized or prevented with targeted programmes. These programmes, while stimulating motor learning processes and optimizing development of activity-specific motor control, also focus on preserving active length and through-range contractility of muscles. However, the changes that occur in muscles in infants with CP are complex and further investigation is necessary before effective interventions can be identified (see Delp, 2003). In the meantime it is possible that a targeted activity programme may have beneficial effects on muscle development if pursued from infancy and with sufficient intensity. Early experience of bearing weight through the feet during varied physical activities, emphasizing the through-range activity of muscles, are critical for achieving balance but are also significant for bone and muscle growth. Weight-bearing pressure (load) and mechanical strain are powerful stimulants of bone formation and growth and physical activity, particularly while weight-bearing, increases bone density in children (Chad et al., 1999; LeVeau and Bernhardt, 1984; Moyer-Mileur et al., 2000; Specker and Binkley, 2003) and in adults (Slemender et al., 1991). Conversely, inactivity leads to resorbtion of bone and decreased bone mineral density (Kuperminc and Stevenson, 2008). Training programmes for young infants should aim to mimic the flexible but also repetitive and intense activity of the normally developing infant in order to minimize negative/non-productive adaptations, to drive brain organization and motor learning. Parents are taught simple activities and task-specific exercises that are incorporated into play; community-based infant ‘exercise’ classes can encourage exploration and activity, and promote learning. Devices to ‘drive’ upper and lower limb activities are being designed so that an infant, once set up, can practice independently exploring the environment—for example, interactive devices encourage and reward kicking actions (Chen et al., 2002; Thelen, 1994; see Chapter 15 and Annotation C). Treadmill training, commonly used and effective in adult neurology, can encourage stepping in infants and strengthen muscles (Bodkin et al., 2003; Ulrich et al., 2001; see Chapters 10 to 12), and can induce changes in the modulation of short latency reflexes during gait in children with CP (Hodapp et al., 2009). Treadmill training and cycling induced by functional electrical stimulating has been shown to be feasible in infants (Trevisi et al., 2012). It is possible that, as in older children, treadmill stepping and walking may also increase the endurance and cardiorespiratory fitness of infants. The use of limb constraint can be effective in both adults and children and is also used in infancy in conjunction with bimanual training (see Chapter 14). Effective for adults after stroke, a suspended harness can provide support and prevent a fall during practice of balancing activities in infancy (Fig. 1.1A,B). A small harness enables an infant with CP to experience standing on the feet and develop the ability to balance while moving the body. Robotic and non-robotic limb trainers (Fig. 1.1C) and virtual reality systems are in development (Sveistrup, 2004; Wu et al., 2011). It is preferable for the infant to be actively engaged in the experience of balancing rather than being held supported in sitting or standing; the ability to balance, critical for all our actions, requires practice of self-initiated movement while unsupported. Figure 1.1 The advantage of a harness held by the parent or therapist or suspended from a ceiling grill or apparatus is in giving the infant the opportunity to practice weight-bearing on the feet and balancing in standing. Although the harness prevents a fall, it does not prevent movement, so the infant has to make postural adjustments to self-initiated movements as he plays. A harness can also be used for walking practice. For infants who cannot bear weight, the harness can take some weight, but the feet must be flat on the floor. (A) Treadmill with harness LiteGait®, with permission from LiteGait®, Mobility research, Tempe, AZ, USA; (B) walkable LiteGait®, with permission from LiteGait®, Mobility research, Tempe, AZ, USA; (C) non-robotic training device (the Sensorimotor Active Rehabilitation Training Arm Neurotrac 5, Verity Medical Ltd). [Courtesy of Dr Ruth Barker, James Cook University, Townsville, Australia.] The complex set of internal processes called motor learning has for some time been the focus of interventions designed to optimize motor performance in neurorehabilitation (Carr and Shepherd, 2010; Gentile, 2000; Magill, 2010). Clinicians are increasingly aware that knowledge of biomechanics provides the foundation for understanding how we move the body’s segmental linkage and remain balanced as we acquire skill (Knutzen and Martin, 2002). Without knowledge of linked segment dynamics the clinician has only observation upon which to base analysis and training of motor actions, and several clinical studies have shown the inaccuracy of such observations. In observation of movement it is necessary to know what to look for, what matters and what does not (Eastlake et al., 1991; Malouin, 1995; Wall, 1999) and this knowledge comes from an understanding of biomechanics and functional anatomy. For example, the infant in Figure 1.2 can stand up, but only with assistance. Observation of the topology (shape) of the movement (dotted line) shows that he has started to extend into standing while his centre of body mass (COM) is too far behind his feet—if unsupported he would fall backward. If the infant’s feet were further back at the start, guiding his knees forward with gentle pressure down toward the feet may enable him to do the rest of the movement himself (see Fig. 11.3A). Raising the seat would also make it easier and enable him to practice repetitions of the basic kinematic components of the standing up/sitting down action. Training of this critical action can be started in early infancy as described in Chapter 11. Figure 1.2 This little boy with diplegia cannot stand up independently from a seat. In (A) his feet should be back under the seat at 75°. In (B) he does not rotate his upper body forward enough to move his body mass over his feet (the next base of support), i.e., hip flexion is insufficient. He will fall back if he is not held. The dotted line represents optimal segmental alignment. In (C), his weight is still too far back and he is not able to stand independently. In large part, this is the functional legacy of lack of training and ↓ calf muscle extensibility. [From Shepherd RB 1995 Physiotherapy in Paediatrics 3rd ed. with permission from Elsevier.] While the clinical focus is on motor learning processes and the mechanics of intersegmental movement, intervention also takes into account the impairments associated with the lesion (primarily, weakness and disordered motor control) and of the adaptive changes that occur when muscles are inactive or muscle activity is uncontrolled. Increasingly there are new findings related to the mechanisms underlying impairments and on adaptive muscle changes. As an example, focus of intervention after stroke in adults is moving away from spasticity (or reflex hyperactivity) as the major problem underlying disability, to the problems of impaired muscle activation and motor control, and of secondary adaptive soft tissue changes associated with inactivity (Carr and Shepherd, 2010). For infants and children with CP, interventions should be similarly focused. Although spasticity seems to attract most attention, clinically it may be confused with decreased extensibility of soft tissue (increased stiffness, decreased length). Furthermore, it is tested in the clinic and the laboratory by passive movement so its effect on active movement is not understood. In some children changes to the stretch reflex may be adaptive phenomena associated with changes to muscle fibres. Treatment of spasticity includes drug therapy that adds to the already present muscle weakness and may not be as effective as functional training (Rameckers et al., 2008; see Chapter 4). Our understanding of the importance of early and active intervention, directed toward muscle weakness and lack of motor control, is increasing and we have a better understanding of the potential effects of inactivity on an immature neuromuscular system (Clowry, 2007; Eyre, 2003; Martin et al., 2007) and on developing perceptuo-cognitive function (see Chapter 10). The goal of training in infants and children with CP is therefore to optimize the development of skilled motor performance (Shepherd, 1995). Ways to achieve these goals include physical activity targeted at the basic actions that are normally mastered by 18 months as part of an infant’s functional skill acquisition: flexion and extension of hips, knees and ankles while weight-bearing; weight-bearing through the upper limbs and pushing and pulling actions; reaching and manipulation; balancing the body mass (Fig. 1.3). Active trunk and hip extension in prone is particularly important in young infants now there are guidelines for preventing cot death that avoid the prone position for sleeping. In general the methodology comprises: Figure 1.3 Basic movements that underlie and are critical for functional motor performance are learned in the infant’s first year and should be the focus of early intervention (see Chapter 11). They include: (A) flexion and extension of lower limbs in standing; (B) weight-bearing through the arm and extending the head and spine in supine; (C) pushing and weight-bearing through the hands; (D) balancing in sitting with hips flexed; (E) balancing the body mass over the feet in standing. [From Shepherd RB 1995 Physiotherapy in Paediatrics 3rd ed. with permission from Elsevier.] These activity-based methods of motor training have been developed over several decades for rehabilitation of adults after stroke (e.g., Carr and Shepherd, 2010) and in children with CP (Damiano, 2006; Fetters, 1991; Shepherd, 1995), and are described in Part 3. Positive effects of activity-based programmes on functional performance have been reported in adults (Dean and Shepherd, 1997; Dean et al., 2000; Eng et al., 2003; Marigold et al., 2005; Sherrington et al., 2008; Wevers et al., 2009) and in children with CP (e.g., Blauw-Hospers and Hadders-Algra, 2005;Echols et al., 2002; Ketelaar et al., 2001; Liao et al., 2007; Schneiberg et al., 2010). These investigations include a pilot study with children aged 3–8 years old that showed significant improvements in muscle strength, performance of sit-to-stand and walking after a four-week programme of lower limb exercise and action-specific training (Blundell et al., 2003). Several training and exercise programmes are being developed out of a similar theoretical background. Although they have various names (Box 1.1), they are basically driven by the need to get the infant as active as possible and all could be considered activity-based. Infants with CP who are less than 18 months are not commonly referred for physical intervention, and there has therefore been little investigation of the effects on infants of this type of intervention. Many developments in interactive technologies including robotics and other interactive devices (Fig. 1.1C), in virtual reality, in orthotics and prosthetics, and in the use of brain scanning to guide treatment choice (Clowry, 2007) have the potential to impact increasingly on physical therapies and exercise science now and in the future (see Chapter 15 and Annotation C). Central neural damage can occur preterm or in the immediate perinatal period. It may be associated with prematurity, hypoxic brain damage, periventricular white matter (PWM) damage, or intraventricular haemorrhage. The sequelae are referred to as CP. The European Cerebral Palsy Study (Flodmark et al., 2003) found approximately 50% of the babies with CP who were studied had central neural damage occurring in the perinatal period. Central neural damage also occurs postnatally in association with traumatic brain injury or stroke. A major problem for physicians, therapists and parents has been difficulty predicting which infants are likely to develop significant impairments that may impact on the infant’s development. As a result, physicians have been understandably reluctant to refer infants for activity-based physiotherapy programmes before they could be confident, using neurological testing, that such a programme is necessary. Traditional neurological testing may not, however, be sensitive or specific enough to enable a reliable diagnosis or prognosis. No correlations have been found between any of these signs and the severity of later impairment (Ferrari et al., 2003). However, it is likely that failure to intervene until soft tissue adaptations have occurred and ineffective patterns of motor behaviour have become well established is a major obstacle to the optimization of the infant’s development. Early and reliable predictors allow for early intervention, and technological and theoretical advances currently being made will enable more accurate and earlier predictions (Ferrari et al., 2003). Two ongoing developments that should stimulate earlier referral are in neonatal neuroradiology and in the evaluation of infant movements. Developments in neonatal neuroradiology, particularly in functional magnetic resonance imaging (fMRI) and the use of transcranial magnetic stimulation (TMS) are clarifying the causes and nature of brain injury and improving the predictability of impairments and disability (see Chapters 2 and 3). Neonatal neuroradiology has shown that certain patterns of brain damage depend on the selective vulnerability of various parts of the brain during development and maturation of the brain (Flodmark et al., 2003). Damage to PWM, for example, is the response to insults occurring between 24 and 34 gestational weeks. The analysis of 180 MRI scans as part of the European Cerebral Palsy Study showed that PWM damage was the most common cause of CP, often but not always causing diplegia. Partial hypoxia was correlated with widespread cortical damage. Hemiplegia was commonly the result of cortical/subcortical damage. Quadriplegia and dyskinesis was caused by basal ganglia damage. Developments in clinical diagnosis include investigations into the predictive capacity of the infant movement evaluation developed by Prechtl (2001) a decade ago based on observation of spontaneous motor activity, and called general movements (GMs). It has been suggested that the nature of endogenously generated motor activity may be a better indicator of the integrity of motor function than items of the neurological examination based mainly on reactivity to sensory stimuli (Ferrari et al., 2003; see Chapter 8). General movements typical of able-bodied and healthy infants are characterized by complexity, fluency and variation (Hadders-Algra, 2004; Hadders-Algra et al., 2004). Newborn infants with brain lesions show spontaneous motility that does not differ in quantity but loses its elegance, fluency, and complexity. A standardized form of this evaluation has been found to have inter-rater reliability and reliable predictive value for CP and other developmental disorders such as minor neurological dysfunction. The range of abnormalities observable in GMs includes hypokinesis (reduced movement), poor repertoire of movements, abnormal or absent fidgety movements and chaotic and cramped synchronized GMs. A study of 84 high-risk preterm infants examined the infants five to ten times from birth to 60 weeks’ postmenstrual age (Ferrari et al., 2003). In addition, at age 2 years, the children were tested using the Griffith Developmental Scale. Infants with consistent or predominantly cramped synchronized GMs developed CP (33 infants), and the earlier they were observed the more severe the impairment. Absence or abnormality of fidgety movements at age 47–60 weeks’ post-menstrual age was a reliable predictor for later neurological impairment. A poor repertoire of GMs in the absence of fidgety movements appears to be predictive of mild impairment. Figure 1.4 is from a study of the changes in movement occurring in a low-risk infant compared with a high-risk infant (Hadders-Algra et al., 2004). Movements such as kicking that lacked complexity and variation at 2–4 months’ post-term were found to be highly predictive of CP and an indication of the need for early intervention. Figure 1.4 General Movements Assessment: analysing movements on the basis of the amount of complexity and variation. The video-frames are of two infants at fidgety GM age. Read the frames from R to L. The infant in (A) shows normal ‘fidgety’ GMs with rich spatial and temporal variation of movements. The infant in (B) shows abnormal GMs with lack of variation. [From Hadders-Algra M 2004 General movements: a window for early identification of children at high risk for developmental disorders. J Pediatr 145 (Suppl 2):12–18, with permission from Elsevier.] Until recently, attitudes toward motor training and exercise in very young infants have not been particularly positive due to lack of investigative power and knowledge of how the neuromotor system develops, of the mechanisms driving development, of motor learning processes, or of the potential for intensive physical and mental activity to drive post-lesion remedial processes. We are now aware that physical and mental activity affect brain organization through active, self-generated and meaningful physical and sensory perceptual engagement, and that lack of activity and diminished opportunity for learning can also affect brain organization. We understand the possibility that motor development may not be due to innate deterministic and maturational processes but occur largely as a result of the infant’s experiences. Physical activity also drives the development and growth of muscle, and when activity is diminished, muscles adapt and lose their capacity to generate force effectively (see Chapters 6 and 7). In summary, for remedial training in paediatrics to be effective, infants need to be referred as early as possible to enable an early start to a targeted training programme. Increased muscle activation levels, strength and motor control, effectiveness of performance and variability of movement are the goals, using methods that may stimulate motor learning, promote muscle development and preserve muscle contractility and length. A major obstacle to referral for early intervention has been the lack of reliable ways of recognizing early signs of brain injury and of assessing infants. However, this is changing. Increased understanding of the mechanisms of brain and corticospinal tract organization in infancy provides support for referral to early and specifically targeted training programmes. Research and development collaborations are enabling the development of interactive devices for infants to encourage active self-directed movement (see Figs 10.3, 10.4). The next obstacle to be overcome will be educational- updating the knowledge base and clinical skills in undergraduate and postgraduate education and in continuing professional education for paediatricians, physiotherapists, occupational therapists and those who work in infant development.
The changing face of intervention in infants with cerebral palsy
Historical view
Understanding impairments and adaptations and their effects on learning and motor performance
New methods of intervention for infants: task-oriented and activity-based training and exercise
Effectiveness and efficiency
Goals and methods of motor training
 Fostering specific actions by manipulating the infant’s environment to provide opportunity and challenge, using environmental constraints to guide and direct movement
Fostering specific actions by manipulating the infant’s environment to provide opportunity and challenge, using environmental constraints to guide and direct movement
 Activity-related, task- and context-oriented training designed to promote acquisition of specific skill and optimal (effective) motor performance in changing environments, focusing on:
Activity-related, task- and context-oriented training designed to promote acquisition of specific skill and optimal (effective) motor performance in changing environments, focusing on:
 Exercises to stimulate muscle contractility and active stretching to preserve optimal length of soft tissues
Exercises to stimulate muscle contractility and active stretching to preserve optimal length of soft tissues
 Repetitive and varied practice of exercises to build up muscle strength and endurance, and stimulate learning
Repetitive and varied practice of exercises to build up muscle strength and endurance, and stimulate learning
 Training of actions, particularly in standing and sitting, but also in four-point kneeling and half-kneeling, to develop balance and motor control under these conditions
Training of actions, particularly in standing and sitting, but also in four-point kneeling and half-kneeling, to develop balance and motor control under these conditions
 Adaptation of brain, neuromotor and cardiovascular systems and muscles in response to activity and patterns of use; the processes of brain reorganization and skill acquisition
Adaptation of brain, neuromotor and cardiovascular systems and muscles in response to activity and patterns of use; the processes of brain reorganization and skill acquisition
 Mechanisms of primary impairments resulting from the neural lesion and their functional effects
Mechanisms of primary impairments resulting from the neural lesion and their functional effects
 Biomechanics of movement and mechanisms of neuromuscular control; experiential development of movement, action, skill
Biomechanics of movement and mechanisms of neuromuscular control; experiential development of movement, action, skill
 Specificity of neuromuscular control and, therefore, of exercise and training
Specificity of neuromuscular control and, therefore, of exercise and training
 Mechanisms of motor learning, i.e., acquisition of skill, and the critical importance of repetitive, varied and intensive practice
Mechanisms of motor learning, i.e., acquisition of skill, and the critical importance of repetitive, varied and intensive practice
 Exercise science: building up muscle extensibility and joint flexibility, muscle strength and endurance, cardiorespiratory fitness.
Exercise science: building up muscle extensibility and joint flexibility, muscle strength and endurance, cardiorespiratory fitness.
New methods of diagnosis and prediction

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine












