Fig. 9.1
A cadaveric photo (a) and illustration (b) depicting normal anatomy of the posterolateral corner of the knee. The popliteus tendon, popliteofibular ligament, and fibular collateral ligament comprise the main static stabilizers of the posterolateral corner (Reprinted from the American Journal of Sports Medicine [21])
After the exam under anesthesia, the knee is positioned in a leg holder at 75–80°of flexion. A standard hockey stick-shaped incision is made extending proximally along the posterior to midportion of the iliotibial band and distally at the level of Gerdy’s tubercle to develop a posteriorly based skin flap [14–16, 20]. Once the superficial layer of the iliotibial band is visualized, a careful dissection is performed posteriorly using blunt dissection to isolate the long head of the biceps femoris.
Next, a peroneal neurolysis is completed to facilitate access to the posterolateral corner and to mitigate common peroneal nerve damage as a potential postoperative complication from swelling (Fig. 9.2). The common peroneal nerve is located either by palpating 2–3 cm distal to the long head of the biceps femoris or by dissecting through the fascial sheath of the peroneus longus muscle proximal to the lateral aspect of the fibular head. The nerve is carefully dissected from its connective tissue vestments for approximately 6–8 cm to allow for retraction of the nerve from the surgical field as needed for the duration of the procedure.
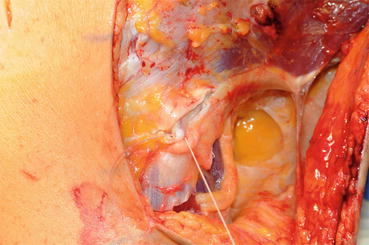
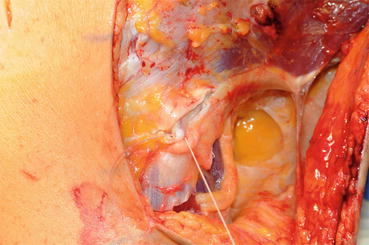
Fig. 9.2
Neurolysis of the common peroneal nerve is performed. The nerve is retracted from the surgical field as needed
After the common peroneal nerve is safely identified, blunt dissection is used to enlarge the interval anterior to the lateral gastrocnemius tendon and posterior to the soleus muscle. This facilitates access to the posteromedial aspect of the fibular styloid and posterolateral tibial plateau [21]. Through this window, the musculotendinous junction of the popliteus tendon and the popliteofibular ligament, which will serve as a posterior reference point for reconstruction tunnels in the tibia and fibula, respectively, is identified.
Next, the fibular attachment of the FCL is visualized by making a small (1.5–2.0 cm long) horizontal incision 1 cm proximal to the lateral aspect of the fibular head through the anterior arm of the long head of the biceps femoris [22]. This incision allows access to the biceps bursa where the distal attachment of the FCL can readily be located. A traction stitch can be placed in the distal remnant of the FCL at this time to aid in the identification of its proximal attachment. The attachments of both the anterior aspect of the anterior arm of the long head of the biceps femoris and the FCL are carefully removed from the fibular head. A small “saddle” should be left where the FCL previously attached to the fibular head [14, 15, 21].
9.2.1 Fibular Reconstruction Tunnel
For the fibular reconstruction tunnel, a standard cannulated cruciate ligament aiming device is positioned in the posteromedial direction, entering at the attachment of the FCL on the lateral fibular head and exiting at the attachment of the popliteofibular ligament on the posteromedial fibular styloid (Fig. 9.3). Once proper alignment is achieved, a guide pin is drilled while holding a retractor posteriorly to prevent over-penetration. The position of the guide pin is assessed by palpation. Once correct positioning is confirmed, a 7-mm tunnel is reamed over the guide pin and the entry and exit sites of the tunnel are beveled with a rasp. A passing suture is then guided through the fibular tunnel to facilitate graft passage.
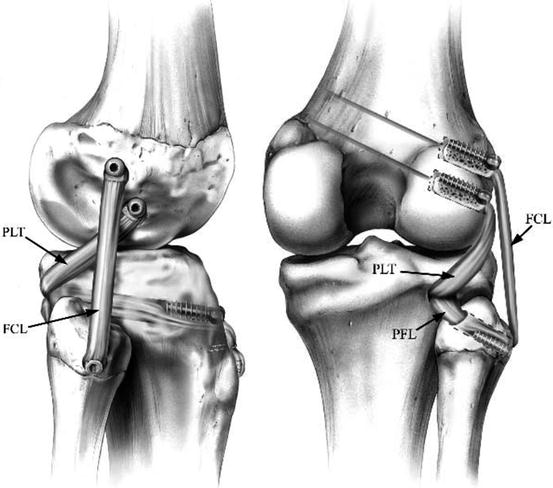
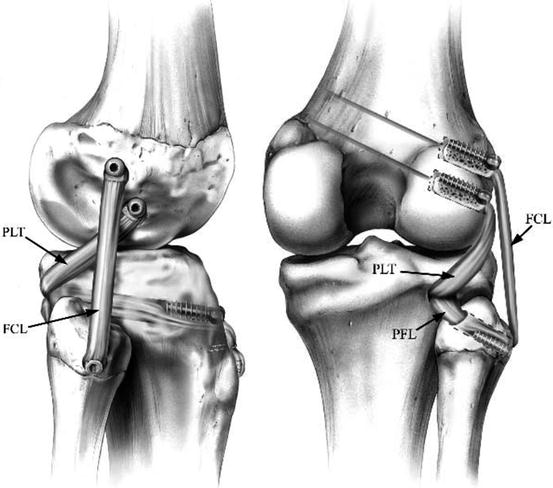
Fig. 9.3
An anatomic-based reconstruction of the posterolateral corner of the knee. Left, lateral view, right knee. Right, posterior view, right knee. Reconstructed ligaments include the main static stabilizers of the PLC: the fibular collateral ligament (FCL), popliteus tendon (PLT), and popliteofibular ligament (PFL) (Reprinted from the American Journal of Sports Medicine [14])
9.2.2 Tibial Reconstruction Tunnel
Next, Gerdy’s tubercle [20] is utilized as a landmark for positioning the tibial reconstruction tunnel. All soft tissue is carefully removed distal and medial to Gerdy’s tubercle to identify the flat spot where the anterior aspect of the tibial tunnel will be placed. The posterior tunnel exit point is determined by palpating deep (anterior) to the popliteus muscle at its musculotendinous junction to locate the posterior tibial popliteal sulcus. This location can also be approximated by inserting a blunt obturator into the fibular reconstruction tunnel to identify a point approximately 1 cm medial and 1 cm proximal to the obturator [14, 15, 21]. Utilizing these reference points, a transtibial guide pin is drilled in the anteroposterior direction from the flat spot distal and medial to Gerdy’s tubercle to the musculotendinous junction of the popliteus muscle. A retractor is used to prevent over-penetration of the guide pin into the posterior neurovascular bundle. The guide pin should exit posteriorly at approximately 1 cm medial and 1 cm proximal to the obturator in the fibular reconstruction tunnel. After verifying the correct positioning of the guide pin, a 9-mm tunnel is reamed and the entry and exits of the tunnel are beveled with a rasp. Finally, a passing suture is guided through the tunnel to aid in graft passage.
9.2.3 Femoral Reconstruction Tunnels
Two femoral tunnels are required for this reconstruction. For the proximal FCL reconstruction tunnel, the proximal attachment of the FCL is located near the lateral epicondyle of the femur by applying traction to the native FCL with the traction suture. Once the attachment is found, a number 15 knife blade is used to make a small incision in the iliotibial band slightly anterior to this site. The remaining FCL is dissected from its femoral attachment. A small indentation should be left behind at the attachment site, which is used to mark the entry of the guide pin. This point is located approximately 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle. [21]. A cruciate ligament aiming device is used to pass an eyelet-tipped guide pin beginning at the femoral attachment of the FCL and traveling in the anteromedial direction. If the guide pin travels too medially, it could breach the intercondylar notch. If the guide pin travels too posteromedially, it could injure the saphenous nerve. Moreover, this orientation of the guide pin also helps to assure that the posterolateral reconstruction tunnels will not converge with an ACL or PCL graft tunnel.
Next, the intra-articular attachment of the popliteus tendon is identified on the femur by making a vertical incision in the lateral joint capsule. The location of the incision is determined either by palpating along the anterior popliteal hiatus or by measuring 2 cm anterior to the course of the fibular collateral ligament. If the popliteus tendon has not been avulsed, it can be found at the anterior fifth and proximal half of the popliteus sulcus [20, 21]. A cruciate ligament aiming device is used to pass an eyelet-tipped guide pin beginning at the attachment of the popliteus tendon in the anteromedial direction and parallel to the fibular collateral ligament guide pin. At this stage, it is critical to measure the distance between these two guide pins in order to accurately assess the restoration of native anatomy. The distance between the guide pins should be 18.5 mm, which reproduces the average distance between the center of the femoral attachments of the FCL and the popliteus tendon [14]. Finally, the guide pins are over-reamed to create two 9-mm-diameter by 25-mm-long femoral reconstruction tunnels. Any residual soft tissue is dissected away from the tunnel apertures, and passing sutures are deployed in the tunnels to facilitate graft passage.
9.2.4 Graft Preparation and Intra-articular Pathology
After completing the four reconstruction tunnels, an allograft Achilles tendon is split lengthwise. The total length of the graft should be >23 cm. The grafts are tubularized using a no. 5 suture such that each graft passes freely through the tibial and femoral reconstruction tunnels. Two 9-mm-diameter by 20-mm-long bone plugs are prepared from a calcaneus allograft to fit the femoral tunnels. Passing sutures are added to the bone and tendon grafts to help maneuver them into their respective tunnels.
At this time, any meniscal, articular cartilage, or cruciate ligament pathologies are addressed. If one or both of the cruciate ligaments require reconstruction, the tunnels are reamed and the cruciate ligament grafts are anchored in their respective femoral tunnels. The PCL graft will be fixed in its tibial tunnel prior to anchoring the reconstructed fibular collateral ligament. The ACL graft will be fixed in its tibial tunnel near the end of the procedure, due to a risk of creating a fixed external rotation deformity [23].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








