Subtrochanteric Femur Fractures: Plate Fixation
Michael J. Beltran
Cory A. Collinge
INTRODUCTION
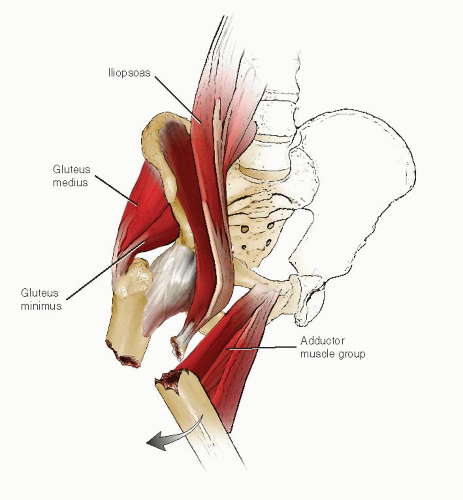
Subtrochanteric femur fractures are challenging injuries to manage, and no single method of treatment is applicable to all fracture patterns. Following a fracture, powerful hip muscle forces often lead to complex but predictable deformities (Fig. 20.1). Intertrochanteric extension, fracture comminution, and poor bone quality increase the difficulty in treatment and require careful preoperative planning. The goal of surgery is to restore length, alignment, and rotation using an implant that provides stable internal fixation and allows early mobilization and protected weight bearing. Subtrochanteric fractures are usually treated with an intramedullary nail or a fixed angle plate; however, the choice of implant depends on the fracture pattern, host factors, and the surgeon’s experience and resources (1, 2, 3, 4, 5, 6, 7 and 8). Several classification schemes have been proposed to categorize subtrochanteric fractures. The comprehensive classification of the AO/OTA is predominately descriptive while the Russell-Taylor classification attempts to guide treatment with either a nail or plate. The purpose of this chapter is to discuss the rationale for plating of the proximal femur and highlight proven techniques that are necessary to achieve a quality reduction and place appropriate, stable internal fixation.
INDICATIONS AND CONTRAINDICATIONS
Virtually all subtrochanteric femur fractures in adolescents and adults require surgery. Given the substantial and serious risks associated with nonoperative care, including deep vein thrombosis, pressure decubiti, urinary tract infections, and pneumonia, traction and casting should only be considered in patients with extremely serious medical comorbidities that preclude surgical intervention. There is widespread agreement that the benefits of correctly done surgery far exceed the risks. For any surgery in the proximal femur, the surgeon must be familiar with the anatomy around the hip to achieve consistently good outcomes. Furthermore, a working knowledge of fracture fixation principles, both mechanical and biologic, is necessary. Proximal femoral plating is contraindicated in any circumstance where the surgeon is unfamiliar with these techniques.
For most subtrochanteric fractures, an intramedullary nail is the treatment of choice. There is a large body of literature documenting successful outcomes following nailing of these difficult injuries (1,2,4,8). Plating is reserved for a subset of fractures where nailing would be challenging and place the patient at an increased risk for complication or failure.
Open reduction and plate fixation of a subtrochanteric femur fractures is indicated in the following situations:
The use of an intramedullary implant is precluded by distal implants (i.e., stemmed total knee prosthesis).
A preexisting implant that must be removed through an open approach.
Comminution of the lateral wall or fracture extension into the greater trochanter or piriformis fossa that makes the use of an intramedullary device difficult or impossible.
For internal fixation after corrective osteotomies for malunion or nonunion of the proximal femur.
The advantage of plating, compared with nailing, is that it reduces the risk of injury to the hip abductors and short external rotators, minimizing the incidence of heterotopic ossification, especially in patients with head injuries.
PREOPERATIVE PLANNING
History and Physical Examination
While subtrochanteric femur fractures are seen in all age groups, they most commonly occur in two age clusters. The first group is elderly osteoporotic patients with fractures that occur following low energy falls or bisphosphonate-related stress fractures. Recent studies have shown a correlation between prolonged bisphosphonate use and atypical fractures of the femur (9,10). In older patients, a history of malignancy should also be sought, as the subtrochanteric region of the femur is a common site for bony metastasis. The second group of patients is younger individuals whose fracture occurs after high-energy trauma (e.g., motorcycle or motor vehicle collisions and falls from a height).
A thorough history and physical examination is mandatory prior to treatment. Advanced Trauma Life Support protocols are used in all seriously injured patients. Virtually all patients present with a painful swollen thigh and are unable to stand or walk. The leg is externally rotated and shortened. Motion in the leg is reduced and very painful. The physical examination should clearly document the neurovascular status. Abnormal or asymmetric distal pulses warrant further studies (i.e., ankle-brachial indices) to rule out a vascular injury. ABIs <0.90 require a vascular consultation and workup (11).
Once life and limb-threatening injuries have been appropriately addressed, the secondary and later tertiary surveys should identify all other musculoskeletal injuries, particularly in the polytraumatized patient with a head or chest injury. Concomitant injuries often impact the timing of surgery and patient positioning and may alter the surgical approach or type of implant to be used. While uncommon, open fractures of the proximal femur often involve small anterior or anterolateral wounds secondary to an inside-out mechanism. All open fractures require early and thorough surgical débridement with fracture stabilization.
Imaging Studies
Initial radiographs should include an AP and lateral of the femur and hip, an AP pelvis, as well as knee films to rule out associated injuries. Traction views with intravenous sedation of the femur are very helpful, as shortening and external rotation are typically present and often obscure the true fracture geometry. Computed tomography (CT) is not typically required for subtrochanteric fractures below the level of the lesser
trochanter. However, a CT scan may be useful if plain radiographs suggest or show involvement of the femoral neck, greater trochanter, or piriformis fossa. Imaging studies must be critically reviewed to determine the integrity of the proximal fragment, since extensive comminution here may preclude the use of an intramedullary nail. Subtrochanteric fractures secondary to low energy falls should also be assessed to rule out a pathologic lesion or an atypical fracture secondary to prolonged bisphosphonate use. The latter typically involve a simple transverse or short oblique fracture associated with cortical beaking and thickening (9,10).
trochanter. However, a CT scan may be useful if plain radiographs suggest or show involvement of the femoral neck, greater trochanter, or piriformis fossa. Imaging studies must be critically reviewed to determine the integrity of the proximal fragment, since extensive comminution here may preclude the use of an intramedullary nail. Subtrochanteric fractures secondary to low energy falls should also be assessed to rule out a pathologic lesion or an atypical fracture secondary to prolonged bisphosphonate use. The latter typically involve a simple transverse or short oblique fracture associated with cortical beaking and thickening (9,10).
Timing of Surgery
Subtrochanteric femur fractures should be considered an urgent orthopedic injury particularly following high-energy trauma because of the inability to mobilize patients until definitive stabilization has been performed. In a patient who is stable and cleared for surgery, internal fixation with a plate or nail should be done as soon as possible, preferably within 24 hours. In the polytraumatized patient in extremis and borderline patients with head and/or chest trauma, damage control surgery using a spanning external fixator may be indicated. Open fractures require emergent débridement and irrigation. We prefer to treat Gustilo and Anderson type I and II fractures with a first-generation cephalosporin and type III open fractures with the addition of an aminoglycoside. Grossly contaminated wounds are uncommon in the proximal femur, but when present the addition of penicillin is advisable.
Surgical Tactic
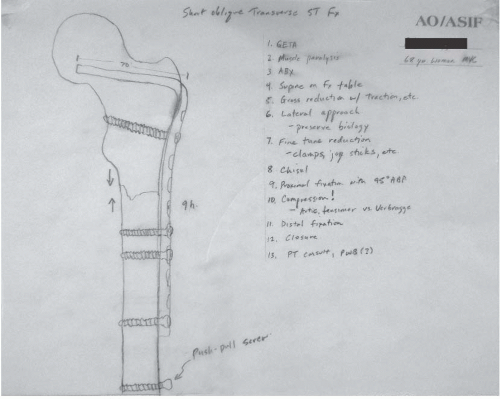
When surgery is planned, a surgical tactic should be developed to enhance efficient surgery and minimize surgical errors (Fig. 20.2). The surgical tactic outlines whether a direct or indirect reduction is required, whether a traditional fixed angle device or a proximal locking plate is necessary, and whether a percutaneous technique can be employed. Tracing out the fracture on paper may help the less-experienced surgeon understand the fracture geometry and the reduction steps better. In circumstances where hospital inventory is limited, a preoperative plan also ensures that all necessary implants are available, especially longer plates, which may require special order. With the use of a 95-degree blade plate, the length of the blade should be determined preoperatively, because intraoperative removal of a wrong-sized implant is difficult and fraught with problems.
The preoperative plan should also take into consideration how intraoperative imaging will be obtained, because the flexed, abducted, and externally rotated position of the proximal fragment makes obtaining standard orthogonal AP and lateral projections difficult. High-quality intraoperative imaging is absolutely critical for fracture reduction and screw placement into the femoral head. Prior to draping, the C-arm should be positioned to confirm that correct views can be consistently obtained, unhindered by overlap of the contralateral thigh.
Two methods of plate fixation for subtrochanteric femur fractures are presented with clinical and radiographic images to demonstrate specific points. First is the “classic” example of a 95-degree angled blade plate (see Fig. 20.10), and the second uses a “modular” fixed angled implant (see Fig. 20.11). Patient positioning and reduction and fixation strategies are similar for both implants.
IMPLANT SELECTION
Compared to plates, nails have a biomechanical advantage given their intramedullary location that decreases bending stresses, varus angulation, and prevents shaft medialization. Contemporary intramedullary nails allow for trochanteric or piriformis entry and enhanced proximal fixation with one or two screws inserted into the femoral neck and head. As a result of these advances, recent studies of subtrochanteric femur fractures fixed with intramedullary nails have demonstrated high union rates and a low incidence of complications (1,4).
Despite their mechanical advantages, intramedullary nailing of subtrochanteric fractures can be technically difficult and fraught with problems. Virtually all nails have an enlarged upper portion to accommodate the proximal interlocking screws designed for femoral head placement. This requires reaming with removal of substantial amounts of bone from the proximal femur (Fig. 20.3). Furthermore, injury to the abductor mechanism has been reported leading to gait disturbances, persistence of pain, or difficulties if revision surgery is required. Occasionally, fracture extension from the entry portal may occur during reaming or insertion of the nail and may cause fracture displacement or varus malalignment.
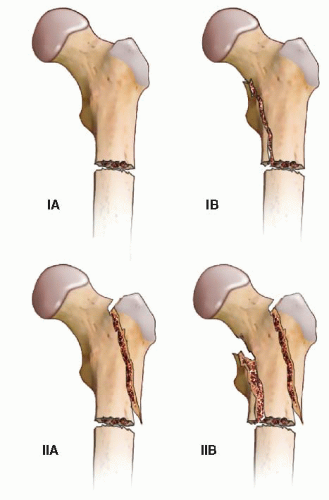
The Russell-Taylor classification system was devised to help guide implant selection (Fig. 20.4). Type IA and IB fractures are easily managed with nails placed through either a piriformis or trochanteric starting point at the discretion of the surgeon. Type 2A fractures, due to fracture extension into the piriformis fossa, preclude use of a piriformis starting point but are often still well treated with trochanteric nails. Type 2B fractures, particularly those complicated by lateral wall comminution, are perhaps the best indication for plating of the proximal femur. Fixed angle plates have been successfully used to treat selected subtrochanteric fractures and avoid many of the problems encountered during nailing. Classically, these fractures were treated with a 95-degree blade plate or a dynamic condylar screw (DCS) and side plate and recently with periarticular locking plates.
The use of these implants allows either direct anatomic reduction with internal fixation or indirect reduction and bridge plating techniques. Simple two- or three-part fractures can be reduced anatomically and fixed leading to absolute stability and primary bone healing. Plate tensioning and fracture compression allow the bone to share load with the plate, increasing mechanical stability and reducing implant fatigue. More complex and comminuted fracture patterns are better treated with indirect reduction and bridge plating (relative stability). In either case, fracture reduction in terms of axial alignment, rotation, and length must be restored if optimal healing and return of function are to be achieved.
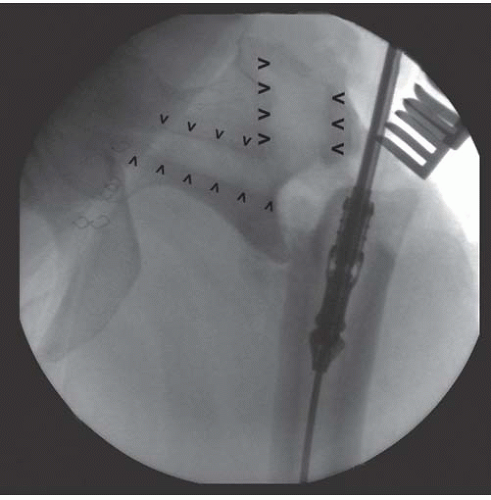 FIGURE 20.3 Intraoperative fluoroscopy during revision surgery shows significant amount of bone removed during cephalomedullary nailing (arrowheads). |
Fixed angle plates minimize injury to the abductor mechanism, which may be particularly important in younger patients, and can be used as a reduction aid, when applied properly. However, plating the proximal femur carries its own set of disadvantages. Bridge plating of unstable fractures creates a load bearing rather than load-sharing implant and is mechanically inferior to a nail. The risk of failure increases in patients with poor bone quality treated with conventional plates and screws. In this setting, the substantial forces across the subtrochanteric region may lead to implant failure.
Currently, plating of the proximal femur is most commonly performed with either a 95-degree angled blade plate, a 95-degree DCS (Synthes, Paoli, PA), or newer proximal femur locking plates. All of these implants are fixed angle devices that improve stability in the proximal femur. Historically, the 95-degree blade plate (Fig. 20.5) was the most commonly used implant for the internal fixation of proximal femur fractures, and there is a large body of literature supporting its use (6,7,12, 13 and 14). However, outside academic medical centers, it is not commonly utilized due to technical complexity and surgeon inexperience. The 95-degree DCS (Fig. 20.6) was developed to address some of these technical issues, but requires removal of significant amounts of proximal bone and has never gained widespread acceptance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree