Reconstruction of Tibialis Anterior Tendon Ruptures
James Santangelo
Mark E. Easley
DEFINITION
Tibialis anterior rupture may present as an acute injury or as a chronic painless foot drop.
The diagnosis is often delayed.
Recommended treatment is surgical for active patients and nonsurgical for low-demand patients. Surgical options include direct repair and reconstruction.
ANATOMY
The tibialis anterior muscle originates from the lateral tibial condyle and interosseous membrane.
Its insertion is the medial side of the medial cuneiform and the inferomedial base of the first metatarsal.
The musculotendinous junction is at the junction of the middle and distal thirds of the tibia.
The tendon courses within a synovial sheath from the musculotendinous junction to its insertion,2 deep to the extensor retinaculum of the ankle and foot.
Innervation is the deep peroneal nerve.
The tibialis anterior muscle controls deceleration of the foot after heel strike and dorsiflexes the ankle.
PATHOGENESIS
Younger individuals with healthy tibialis anterior tendons rarely suffer spontaneous rupture; instead, their mechanism of injury is laceration from penetrating trauma or distal tibia fracture.
Spontaneous ruptures typically occur in older individuals with degenerative tendinopathy of the tibialis anterior tendon. Minor trauma may be associated with these ruptures, with a mechanism of plantarflexion-eversion. Ruptures typically occur within 3 cm of the tendon’s insertion on the medial cuneiform.1
NATURAL HISTORY
The natural history of tibialis anterior rupture is inferred from studies documenting the results of nonoperatively treated patients. These patients will ambulate with a slap foot gait and sometimes have difficulty negotiating uneven terrain. Most patients are functional; however, they may require a brace.
Nonoperatively treated patients tend to be older and lower demand. The natural history for younger, more active patients may indicate less desirable results.
Definite conclusions regarding the natural history of tibialis anterior ruptures are limited due to the low number of reported cases in the literature and lack of natural history studies.
PATIENT HISTORY AND PHYSICAL FINDINGS
Physical examination methods include the following:
Examining for swelling. The examiner should palpate along the course of the tibialis anterior muscle-tendon. Swelling with discontinuity of the tendon indicates a tendon rupture. An anterior ankle mass may be the presenting complaint.
Gait disturbance. The examiner should observe the patient ambulating, looking for slap foot gait or foot drop. Chronic ruptures may present with minimal gait disturbance; the patient may have difficulty ambulating only when on uneven surfaces. Inability to heel walk indicates tibialis anterior dysfunction. The patient may need to hyperflex the hip and knee to clear the foot during the swing phase of gait because the ankle does not dorsiflex adequately.
Muscle strength is evaluated with manual motor testing. No contraction or weak ankle dorsiflexion suggests tibialis anterior dysfunction. Patients will substitute the toe extensors for the tibialis anterior during ankle dorsiflexion, exhibiting toe hyperextension when asked to dorsiflex the ankle.
The examiner should note any heel cord tightness. Subacute and chronic injuries often present with heel cord contractures because the major antagonist to ankle plantarflexion is forfeited with tibialis anterior tendon rupture. As a rule, at least 10 degrees of ankle dorsiflexion must be present for a tibialis anterior repair or reconstruction, and thus surgical management may require adding Achilles tendon or gastrocnemius lengthening.
The examiner should completely assess the involved extremity to rule out other diagnoses. The most common errors in diagnosis are as follows:
Lumbar radiculopathy: presents with diminished sensation, positive straight-leg raise test
Peroneal nerve palsy: affects the toe extensors and peroneal musculature in addition to the tibialis anterior. Preservation of extensor hallucis longus (EHL) and toe extensor function will distinguish tibialis anterior rupture from peroneal nerve palsy.1
IMAGING AND OTHER DIAGNOSTIC STUDIES
Imaging studies are generally not required in the evaluation of tibialis anterior tendon ruptures because the diagnosis is usually simple to make on clinical examination alone.
Radiographs are nondiagnostic and rarely required in the evaluation of tibialis anterior tendon ruptures. Radiographs are, however, useful to assess associated injures (tibial fractures).
Magnetic resonance imaging (MRI) may be useful in chronic cases where patients do not recall a history of trauma.1 MRI demonstrates lack of continuity in the tibialis anterior and signal change in the tendon, particularly with preexisting tendinopathy. Because the tibialis anterior tendon courses from lateral to medial across the anterior ankle and retracts with rupture, occasionally, it is difficult to assess.
If there is uncertainty in the diagnosis, electrodiagnostic studies may identify common peroneal palsy or lumbar radiculopathy.
DIFFERENTIAL DIAGNOSIS
Peroneal nerve palsy
Lumbar radiculopathy
Rarely, a peripheral neuropathy may present as isolated tibialis anterior tendon dysfunction.
NONOPERATIVE MANAGEMENT
Low-demand patients may be treated with an ankle-foot orthosis (AFO).
SURGICAL MANAGEMENT
Direct repair of the tendon is occasionally possible, but delay in diagnosis may preclude direct repair due to muscle contracture.
A sliding tibialis anterior tendon grafting technique has been described to gain tendon length to allow repair, and allograft tendon transfers have been proposed in the absence of tibialis anterior myofibrosis.
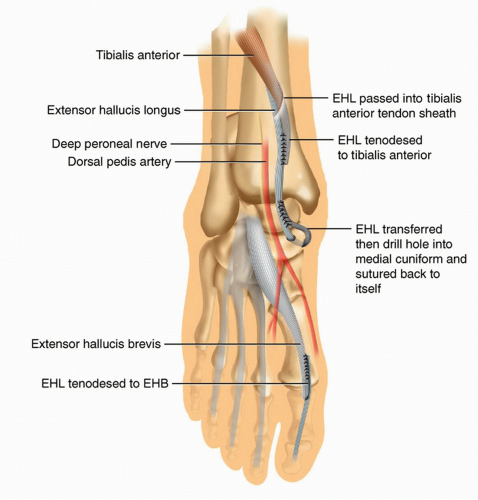
Our preferred reconstruction for tendons that cannot be directly repaired is to augment the repair with the adjacent, native EHL tendon (FIG 1).
Indications for allograft tendon reconstruction
Advanced tibialis anterior tendon degeneration
Tibialis anterior muscle excursion preserved
Minimal to no myofibrosis
Allograft reconstruction for a muscle that has no excursion, that is, is scarred, will result in a no more than a tenodesis without function.
Preoperative Planning
Imaging studies are reviewed when available to appreciate the extent of preexisting tendinopathy and to potentially identify the approximate site of the rupture.
The surgeon should prepare for Achilles tendon lengthening or gastrocnemius-soleus recession to achieve adequate (at least 10 degrees) dorsiflexion.
Positioning
The patient is positioned supine. A bump may be placed under the ipsilateral hip, but this is typically not necessary because access is required only to the anteromedial ankle.
Approach
An anterior approach is made directly over the course of the tibialis anterior tendon.
As has been learned from total ankle arthroplasty and open reduction and internal fixation of tibial pilon fractures, careful soft tissue handling is essential.
TECHNIQUES
▪ Extensor Hallucis Longus Transfer to Medial Cuneiform
Exposure
Perform gastrocnemius recession or Achilles tendon lengthening if indicated.
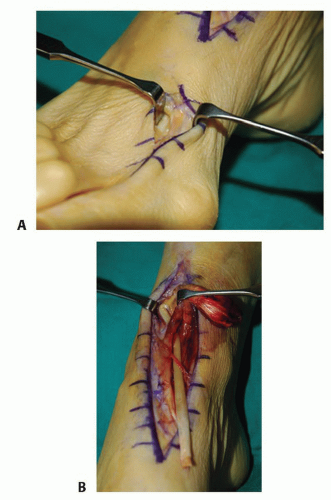
Use an anterior approach with an incision over the course of the tibialis anterior tendon (TECH FIG 1).
Divide the superior and inferior extensor retinaculum and tibialis anterior sheath.
Isolate the remnant of the tibialis anterior tendon. Occasionally, direct repair is possible, rarely by advancing the residual tendon to bone, but instead to the residual tendon stump on the medial cuneiform. If inadequate tendon is available or muscle excursion is poor, proceed with EHL transfer.
Extensor Hallucis Longus Transfer
Expose the EHL tendon. Proximally, the EHL is in a separate sheath adjacent to the tibialis anterior.
Through a separate 3- to 5 -cm incision over the distal EHL immediately proximal to the first metatarsophalangeal joint, divide the EHL tendon distally. Leave enough distal stump to suture to the adjacent tendon of the extensor hallucis brevis. Place a whipstitch consisting of no. 2 nonabsorbable suture in the free end of the EHL.
TECH FIG 1 • A. Anterior approach over tibialis anterior. B. The tendon sheath is opened, exposing the torn retracted end of the tibialis anterior. The sheath is carefully preserved for later repair.
Pass the EHL under the skin bridge and through the tibialis anterior sheath proximally. The EHL will now occupy the previous sheath for the tibialis anterior (TECH FIG 2).
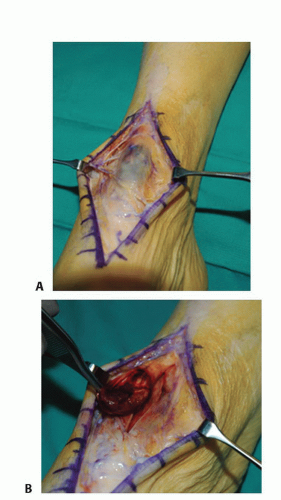
Drill a vertical hole in the medial cuneiform for attachment of the EHL. Sequentially drill using 2.5-, 3.5-, and 4.5-mm drill bits. Enlarge the hole with a curette as needed to allow graft passage. Leave enough periosteum to provide additional points of attachment for suturing the graft in place.
Fixation
Secure the graft with the ankle in 10 degrees of dorsiflexion (TECH FIG 3A-D).
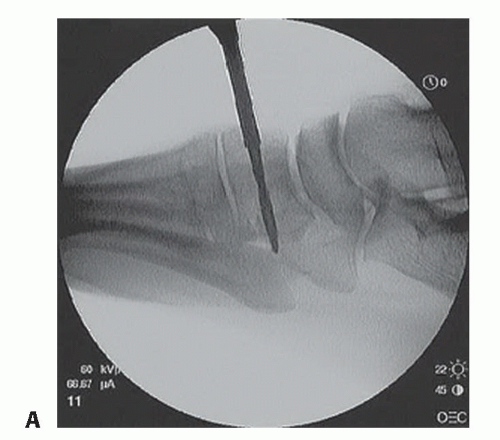
TECH FIG 3 • A. A drill hole is placed from dorsal to plantar at the midpoint of the medial cuneiform. (continued)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access