9 Preparing for exercise after stroke
Introduction
Clinical guidelines generally recommend that exercise training should be provided as part of the post-rehabilitation care of stroke survivors. This is because much of the evidence about the effectiveness of exercise comes from trials which provided exercise training after usual stroke care had been completed (chapter 5). Some stroke services may wish to integrate exercise training into usual stroke rehabilitation and, whilst it is highly plausible that exercise training may be of benefit at this stage in the patient journey, the evidence base is less strong. This may change as new trials are published.
This chapter will detail the preparatory processes, undertaken by both health-care and exercise professionals, before a stroke survivor commences exercise and fitness training. We are assuming that exercise is provided in community settings, and delivered by an exercise professional, who may have come from one of the professional backgrounds mentioned in chapter 2.
One of the central recommendations is that patients should be formally referred to exercise services, just as they might be referred to other services. This means that the referrer provides important clinical information to the exercise professional or physiotherapist delivering the exercise. In the UK, exercise referral schemes have been available in the community for many years now, and there are established referral routes in and out of the services (Department of Health 2001). In the UK, Exercise after Stroke services are being developed using the well-established exercise referral pathways for people with coronary heart disease and those who have had a fall.
Exercise referral routes into the exercise after stroke service
Referral from primary care
The other main route into Exercise after Stroke services is for stroke survivors already discharged from secondary health-care services. All health professionals who come into contact with stroke survivors should address the issue of exercise along with other lifestyle factors which are important for secondary stroke prevention. Health professionals should address personal, social and environmental barriers to exercise (see chapter 6). Referral to an Exercise after Stroke service should be made wherever possible. People who had a stroke some time ago or did not receive inpatient treatment should access Exercise after Stroke services through their general practitioner (GP) or other appropriate health professional, e.g. practice nurse (delegated by the GP), community physiotherapist, stroke specialist nurse or occupational therapist.
Process of referral to an exercise after stroke service
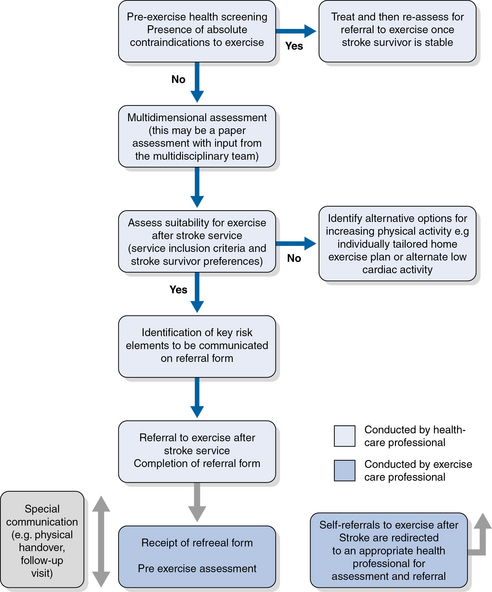
Based on an extensive scoping project to identify Exercise after Stroke services in Scotland and existing guidelines for exercise referral schemes (Best et al. 2010), we developed a referral pathway for people after stroke (Fig. 9.1). More information is given about each stage in the following sections.
Pre-exercise assessments
1. Screening for absolute contraindications for exercise: to identify people who should not be exercising due to unstable medical conditions.
2. Multidimensional assessment: to give the exercise professional a global picture of the individual stroke survivor’s medical and functional status.
3. Local Exercise after Stroke inclusion criteria: to ensure a match between the stroke survivor and the Exercise after Stroke session.
4. Risk assessment and management: to highlight areas of the multidimensional assessment that require specific tailoring of the exercise intervention in order to ensure the maximum possible benefit from exercise.
Screening for absolute contraindications for exercise after stroke
The referring health professional will determine whether there are any absolute contraindications to exercise after stroke. These absolute contraindications are based on the most recent ACSM guidelines for exercise testing (ACSM 2010) and also absolute contraindications for exercise training in vulnerable older patients (Dinan 2001). Note that the absolute contraindications are mainly due to unstable heart disease (Box 9.1).
Box 9.1 Absolute contraindications to Exercise after Stroke
 Recent electrocardiogram changes suggesting significant ischaemia, recent myocardial infarction (within 2 days) or other acute cardiac event
Recent electrocardiogram changes suggesting significant ischaemia, recent myocardial infarction (within 2 days) or other acute cardiac event
 Uncontrolled cardiac dysrhythmias causing symptoms or haemodynamic compromise
Uncontrolled cardiac dysrhythmias causing symptoms or haemodynamic compromise
 Symptomatic severe aortic stenosis
Symptomatic severe aortic stenosis
 Uncontrolled symptomatic heart failure
Uncontrolled symptomatic heart failure
 Acute pulmonary embolism or pulmonary infarction
Acute pulmonary embolism or pulmonary infarction
 Acute myocarditis or pericarditis
Acute myocarditis or pericarditis
 Suspected or known dissecting aneurysm
Suspected or known dissecting aneurysm
 Acute systemic infection, accompanied by fever, body aches or swollen lymph glands
Acute systemic infection, accompanied by fever, body aches or swollen lymph glands
 Extreme obesity, with weight exceeding the recommendations or the equipment capacity (usually >159 kg [350 lb])
Extreme obesity, with weight exceeding the recommendations or the equipment capacity (usually >159 kg [350 lb])
 Uncontrolled visual or vestibular disturbances
Uncontrolled visual or vestibular disturbances
 Recent injurious fall without medical assessment
Recent injurious fall without medical assessment
Based on American College of Sports Medicine absolute contraindications to exercise testing (ACSM 2010), and the absolute contraindications to exercise training in vulnerable older patients (Dinan 2001).
Multidimensional Pre-exercise assessment
The long-term effects of stroke are varied and wide-ranging so the exercise professional will need an overview of the stroke survivor’s residual neurological impairments (chapter 1) as well as any other post-stroke problems, co-morbidities and medication (chapter 3), so that the exercise programme can be tailored to the needs of individual stroke survivors. Once absolute contraindications to exercise have been excluded, the health professional should proceed to the multidimensional assessment, which should cover all domains shown in Box 9.2. Most of this information would be available from the stroke survivor’s medical records. This type of assessment is labelled ‘multidimensional’ as one health professional may not be able to complete all relevant sections. If this is the case, input from other members of the multidisciplinary team or primary care team should be sought where necessary. This information must be communicated to the exercise professional in appropriate terminology. Each service will need to design its own form according to local requirements. An example of a referral form that was developed by the NHS Greater Glasgow and Clyde therapeutic exercise working group is shown in Box 9.3.
Box 9.2 Multidimensional pre-exercise assessment
This information should be transferred to the exercise professional, once absolute contraindications to exercise have been ruled out, and the stroke survivor has given written informed consent to be referred. (For an example of the content of a referral form see Box 9.3.)
 General medical and stroke medical history
General medical and stroke medical history
 Information on any co-morbidity that might contraindicate or restrict exercise, e.g. ischaemic heart disease, heart failure, respiratory disease, poor circulation, uncontrolled epilepsy, joint replacements, etc.
Information on any co-morbidity that might contraindicate or restrict exercise, e.g. ischaemic heart disease, heart failure, respiratory disease, poor circulation, uncontrolled epilepsy, joint replacements, etc.
 Medications and how these may restrict exercise ability
Medications and how these may restrict exercise ability
 Pain status: stroke-related (central or shoulder), musculoskeletal or other
Pain status: stroke-related (central or shoulder), musculoskeletal or other
 Joint active and passive range of motion (particularly with relation to the risks associated with subluxation or poor control in shoulder movement – a common source of post stroke pain)
Joint active and passive range of motion (particularly with relation to the risks associated with subluxation or poor control in shoulder movement – a common source of post stroke pain)
 Motor control: coordination of joint stability, strength and power, protective reactions, movement involving single and multiple body segments, and functional activities
Motor control: coordination of joint stability, strength and power, protective reactions, movement involving single and multiple body segments, and functional activities
 Balance both in static and dynamic situations and recovery responses
Balance both in static and dynamic situations and recovery responses
 Gait (walking ability), addressing both neurological and biomechanical aspects of gait. Ideally, this should include different variations of gait (i.e. slow, fast, backward and side-stepping, turning, managing obstacles and stair climbing) in different environments (i.e. rough and smooth ground, flat ground and slopes, different lighting and noise conditions)
Gait (walking ability), addressing both neurological and biomechanical aspects of gait. Ideally, this should include different variations of gait (i.e. slow, fast, backward and side-stepping, turning, managing obstacles and stair climbing) in different environments (i.e. rough and smooth ground, flat ground and slopes, different lighting and noise conditions)
 Visuospatial problems, difficulties with body schema awareness
Visuospatial problems, difficulties with body schema awareness
 Functional abilities history and direct observations of functional tasks related to activities of daily living
Functional abilities history and direct observations of functional tasks related to activities of daily living
 Compensatory overuse of less affected side
Compensatory overuse of less affected side
 Activity history including current physical activity status, interests, preferences, means and readiness to exercise. This indicates that the stroke survivor has agreed with the referring party that they are ready to exercise, are motivated enough to attempt a programme, and able to attend the intended exercise programme times
Activity history including current physical activity status, interests, preferences, means and readiness to exercise. This indicates that the stroke survivor has agreed with the referring party that they are ready to exercise, are motivated enough to attempt a programme, and able to attend the intended exercise programme times
 Communication: the stroke survivor’s ability to understand and follow instructions and to communicate with the exercise instructor, including the presence of aphasia and/or dysarthria (see chapter 3)
Communication: the stroke survivor’s ability to understand and follow instructions and to communicate with the exercise instructor, including the presence of aphasia and/or dysarthria (see chapter 3)
 Cognition: the presence of memory impairment, executive dysfunction, impaired insight or dementia, may require adapted communication strategies to allow the individual to participate or require the involvement of a communication assistant
Cognition: the presence of memory impairment, executive dysfunction, impaired insight or dementia, may require adapted communication strategies to allow the individual to participate or require the involvement of a communication assistant