Week
Goals of the activity
0–6
Pain reduction, rest, icing, elevation
Muscle reeducation, submaximal quadriceps/hamstring isometrics (pain-free)
Electrical stimulation with the Swiss ball
Taping and/or knee bracing in extension
Scar tissue mobilization
6–10
Single-leg stance balancing and weight shifts
Gentle quadriceps, hamstrings of motion, and gastrocnemius stretches
Hip strength and knee stabilization by TheraBand
Improve knee strength: squatting (30–60–90°)
Standing electrical muscle stimulation (20 min)
10–24
Restore neuromuscular balance-coordination activities on board
Quarter squats
Bicycle, jog, and swim endurance for cardiovascular endurance
Normal knee strength by using isokinetic system
Half squats, hamstring curls, lunges, leg press
28–52
Return to sport, sport-specific drills, functional tests, isokinetic evaluation
16.1 Phase 1 (0–6 Weeks)
The initial treatment phase includes modalities such as weight-bearing activities to normalize gait, quadriceps strengthening for muscle reeducation, and gentle knee stretches for restoring flexibility. Strict guidelines are to be followed: a home exercise program consisting ice, gastrocnemius and hamstring stretches, heel slides, quadriceps setting, and straight-leg raising (SLR) is emphasized. The appropriate method of exercise in the early phase of soft tissue healing is isometric exercises involving isometric contractions of the quadriceps, hamstrings, and gastrocnemius muscle groups as a cocontraction activity. Modalities as interferential electrical stimulation, cryotherapy, compression, and nonsteroidal anti-inflammatory drugs can be used for decreasing the pain and edema. Electrical stimulation is a supplementary method to regain quadriceps strength [3].
Prolonged immobilization in the early postoperative period is associated with periarticular adhesions and arthrofibrosis that lead to decrease in ROM, destruction of joint cartilage, muscle atrophy, and disuse osteoporosis. Therefore, patellar mobility and quadriceps strengthening/stretching exercises are to be started in the earliest time as pain and effusion would allow. Also to avoid flexion contracture, full passive extension should be gained in the early period with a great precaution not to harm reconstructed tissues.
One of the most important goals to achieve in the initial phase of the rehabilitation is to improve the proprioception and kinesthesia that had been disturbed at the time of the injury. The damaged mechanoreceptors on the injured collateral or cruciate ligaments can never regrow into the grafts. Instead, specific exercises may facilitate the intact mechanoreceptors for compensation. Various exercises that can be used for this purpose are angular joint replication training, end-ROM reproduction training, and perturbation training [4].
In a review of the literature, [5] stated that, continuous passive motion does not provide any substantial advantage following ACL reconstruction, except a possible pain relief. Similarly, Smith and Davies concluded that there was no difference between joint laxity, functional outcomes, postoperative complications, radiological changes, ecchymoses, and muscle atrophy in patients who received continuous passive motion or not [6]. Despite the absence of evidence about any advantages, continuous passive motion may be considered in the immediate postoperative period to decrease postoperative pain.
16.1.1 Early Weight Bearing
The weight bearing must be strictly avoided in the first 4 weeks. Further, as the pain and edema decreases and ROM and neuromuscular control improves, partial weight bearing can be gradually allowed in compliant patients. Besides, a healing time, ranging from 6 to 12 weeks, which is dependent to the type of fixation determines the duration of protection [7]. The timing and amount of weight bearing after reconstruction of isolated ligamentous injuries are well defined. Wright et al. investigated the efficacy of immediate weight bearing versus delayed weight bearing following ACL reconstruction. No deleterious effects of early weight bearing were found regarding stability or function. They suggested that anterior knee pain would decrease with early weight bearing [8]. Following medial collateral ligament (MCL) repairs, non-weight bearing is recommended for the initial 3 weeks with weight bearing as tolerated at 3 weeks; however, effects of early weight bearing are unknown following MCL injury or repair to the MCL [8–10]. Despite that little evidence exists regarding weight-bearing status following posterior cruciate ligament (PCL) injuries, partial weight-bearing status is recommended for 2–4 weeks following PCL surgery to protect the healing structures [11].
In case of multiligamentous reconstructions of the knee joint, no weight bearing for the first week and limited weight bearing for the first 6 weeks is recommended [12]. The effects of early weight bearing following multiligamentous knee surgery are not clear, while early weight bearing following anterior cruciate ligament (ACL) reconstruction is safe without any detrimental effects on stability or function [13].
16.1.2 Knee Bracing
We recommend protecting the reconstructed and repaired tissues with a knee brace locked in extension for 6 weeks postoperatively. After 1 week, controlled non-weight-bearing limited flexion is allowed. Because knee flexion past 100° can increase strain on PCL, knee flexion should be limited at 90° in phase 1 rehabilitation protocols [7].
Despite several studies demonstrated the efficacy of a functional knee brace during early treatment following acute ACL rupture or prophylactic bracing in ACL-deficient knees, there is no evidence to support the routine use of postoperative bracing following ACL reconstruction in systematic reviews [14–17]. However, recent surveys demonstrated that approximately 50–60 % of orthopedic surgeons still use bracing in the early postoperative period following ACL surgery [18].
In the postoperative management of PCL reconstruction, a hinged brace is typically used as the knee is locked in full extension for 2–4 weeks to avoid the effects of gravity and the pulling effect of the hamstrings [19]. However, there is no current evidence indicating that bracing prevents posterior tibial translation [11].
Bracing seems to be beneficial for severe grade II and grade III ruptures of the MCL or following MCL surgery. A long-hinged brace allowing 30–90° of knee motion for the first 3 weeks followed by progressive weaning off the brace starting at week 6 is recommended [9].
16.1.3 Immediate Versus Delayed Mobilization
The current evidence points the benefits of the early mobilization for a successful outcome after ACL and PCL reconstructions. Beynnon et al. summarized five randomized controlled trials on the effects of immediate knee motion as compared to delayed knee motion following ACL reconstruction. The authors concluded that early joint motion after reconstruction of the ACL appears to be beneficial with reduction in pain, lesser adverse changes to the articular cartilage, and helping prevent the formation of scar and capsular contractions that have the potential to limit joint motion [20]. Harner et al. recommend a 2- to 4-week period of immobilization in full extension following a grade III PCL injury to maintain reduction of the tibia and minimize posterior sag to limit forces on the damaged PCL and posterolateral structures. The same recommendations can be applied for following PCL reconstructions [21].
16.2 Phase 2 (6–10 Weeks)
In this phase, the knee brace is unlocked to allow full flexion. The patient is allowed for protective weight bearing to approximately 20 % of body weight with crutches. Furthermore, the weight bearing can be allowed to progress by 20 % each week until full weight bearing is allowed at the postoperative week 10. Any residual flexion contracture can cause extensor mechanism irritation. Although the crutches are discontinued at this point, a multi-instability-specific brace providing anterior-posterior-lateral-medial support is recommended to protect the knee.
In this phase, the goal of knee extension is to obtain and maintain physiologic recurvatum because active neutral extension must be achieved to assume full weight bearing. A gradual increase in passive flexion is allowed to reach the uninvolved side by weeks 8–12. It permits the graft and other soft tissues to adapt the length changes. To not cause early failure on grafts, patient should not be encouraged to attain over 90° of flexion until the end of postoperative week 10. One hundred twenty-five degrees of flexion is adequate even for high-demand activities after week 12.
16.2.1 Neuromuscular Reeducation
Neuromuscular reeducation or neuromuscular (proprioceptive) training has been defined as movement training progressions that facilitate the development of multijoint neuromuscular engrams that combine joint stabilization, acceleration, deceleration, and kinesthesia through intermittent protocols that progress from low-intensity movements focused in a single plane to multiplanar power training [22]. Cooper et al. investigated the use of proprioceptive and traditional strengthening exercises in individuals with ACL deficiency. Limited improvements were noted in muscle strength, subjective rating, and hop testing following neuromuscular training when compared to traditional strengthening in patients with ACL deficiency [23].
The proprioceptive and kinesthesia exercises progress in a systematic sequence. Partial weight bearing progresses to full weight bearing, double-leg exercises progress to single-leg, single-plane tilt board exercises progress to multi-plane, and open-eye exercises progress to closed eye [24]. Proprioceptive neuromuscular facilitation exercise for hamstrings and quadriceps (Fig. 16.1a, b), progressive resistance training, and balance-coordination exercises for multiligamentous injuries are effective in reducing pain and improving quality of life.
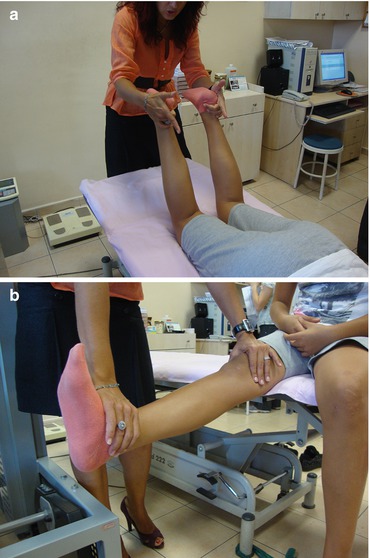
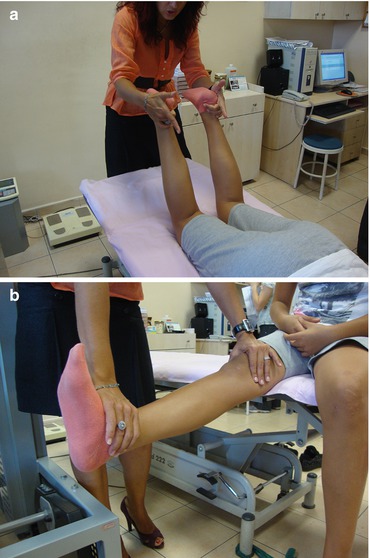
Fig. 16.1




(a, b) Proprioceptive neuromuscular facilitation techniques for hamstrings and quadriceps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








