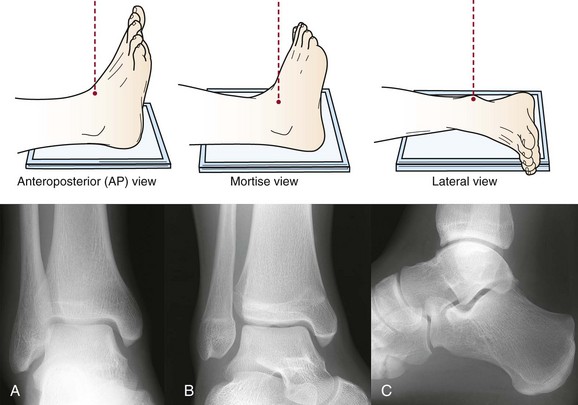
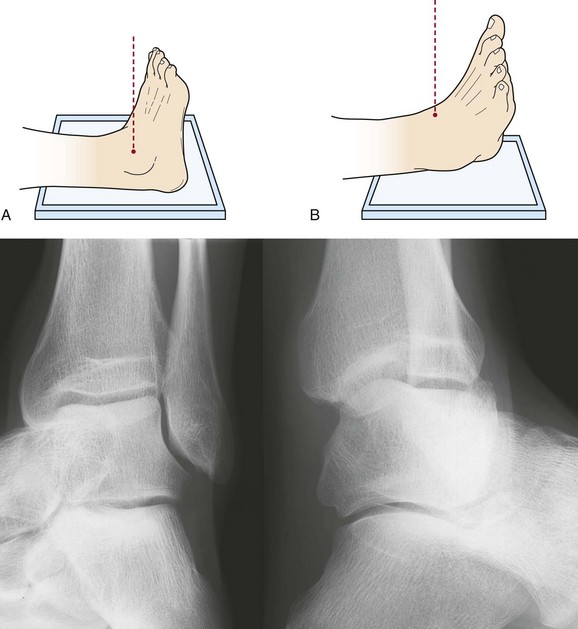
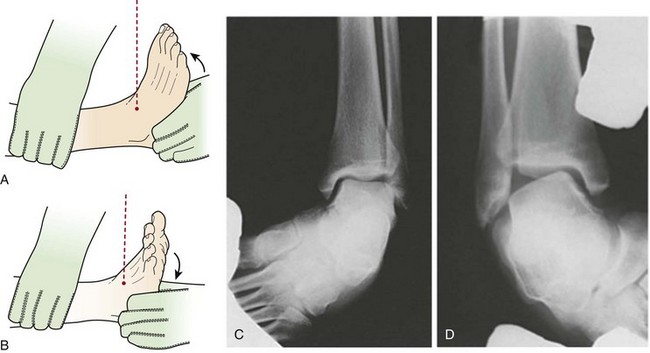
Chapter 3 Magnetic Resonance Imaging Clinical Sequences T1-Weighted Fast Spin-Echo Sequences T2-Weighted Fast Spin-Echo Sequences Proton-Density–Weighted Fast Spin-Echo Sequences Short Tau Inversion Recovery or “Fat-Sat” Sequences Magnetic Resonance Arthrogaphy New Magnetic Resonance Imaging Technique: Biochemical Imaging Contraindications to Magnetic Resonance Imaging Pitfalls and Artifacts in Magnetic Resonance Imaging IMAGING OF FOOT AND ANKLE PATHOLOGY Imaging Chondral and Osteochondral Lesions Imaging Articular Cartilage Repair Imaging Inflammatory Arthropathies Imaging Nerve Pathology in the Foot and Ankle Imaging Tumors in the Foot and Ankle Imaging Infections in the Foot and Ankle Miscellaneous Conditions in the Foot and Ankle Although valuable as a diagnostic tool, imaging should only be requested if the result will be used to guide management and is most effective when used to confirm or exclude a specific clinical hypothesis or to narrow a clinical differential. In this setting, the test has a specific purpose, and the result has direct clinical meaning. The importance of a thorough clinical assessment therefore cannot be overemphasized, because it is only on the basis of specific questions that arise from the history and physical examination that the most appropriate imaging test(s) can be chosen. A valid clinical role for imaging can include the detection or exclusion of sinister or systemic disease when clinical “red flags” are present (Table 3-1). Table 3-1 Plain radiographs, computed tomography (CT) scans and isotope bone scans all expose patients to ionizing radiation that carries a risk of both cancer induction and genetic damage. This risk is well established at high doses (e.g., Hiroshima victims) but remains uncertain at low doses, such as those used in medical imaging. Because all populations are exposed to the natural background radiation of cosmic rays (Table 3-2) and also have an incidence of cancers arising from causes other than radiation, it is statistically difficult to evaluate the cancer risk associated with medical radiations at doses of 100 mSv or less.25 A cautious “linear no-threshold model” has therefore been adopted that assumes that even the smallest radiation dose carries a level of risk and that this risk increases linearly with cumulative lifetime exposure. It is also well recognized that, depending on age, children can be up to 10 times more sensitive to ionizing radiation than adults, and an actual effect equivalent to one excess case of leukemia and one excess case of brain tumor per 10,000 head CT scans has recently been shown for the first time in children younger than 10 years who underwent multiple CT head scans with a cumulative dose of 50 to 60 mGy.57 Table 3-2 Typical Effective Radiation Dose3,42,44 These risks should be kept in perspective. The radiation dose associated with a basic three-view foot radiograph is at least 10 times lower than the exposure associated with a single trans-Atlantic air flight (Table 3-2), and it is generally accepted that medical imaging tests are justified if there is a reasonable likelihood they will provide a health benefit or inform patient management.6 Nevertheless, medical exposures should always be kept “As Low As Reasonably Achievable” (ALARA principle), and alternative tests, such as ultrasound and MRI, which avoid ionizing radiations altogether are preferable to CT or isotope studies whenever they offer equivalent or superior diagnostic efficacy, particularly in children and especially for follow-up imaging. In clinical practice, radiologists normally exercise caution and specify imaging protocols that minimize the ionizing radiation dose. The surgeon should also feel comfortable that the doses involved in foot and ankle imaging are mostly extremely low (see Table 3-2). Last, the American Association of Physicists in Medicine has recently issued a reassuring policy statement that asserts that “the risks of medical imaging at effective doses below 50 mSv for single procedures or 100 mSv for multiple procedures over short time periods are too low to be detectable and may be nonexistent.”1 An effective radiographic examination provides fine anatomic detail and comprises appropriate views that have been correctly positioned. Poor radiographic technique may contribute to diagnostic error by invalidating established radiographic signs, measurements, and alignment criteria. Whenever the relevant anatomy of clinical interest has not been clearly demonstrated, the examination is technically inadequate and should be repeated.2 Film interpretation requires knowledge of (1) normal bone development in the pediatric patient65 (Fig. 3-1) and (2) normal anatomic variants at all ages. Secondary centers of ossification and sesamoids of the foot can both be mistaken for fractures65 (Fig. 3-2). A full discussion of normal variants is beyond the scope of this chapter, but appropriate references should be consulted when in doubt.30,66 The routine ankle series consists of an anteroposterior (AP) view, mortise view, and lateral view (Fig. 3-3). The routine foot series consists of an AP view (Fig. 3-4), oblique view (Fig. 3-5) and a lateral view (Fig. 3-6). The optimal assessment of alignment and joint space at the foot and ankle requires weight-bearing views whenever possible (Figs. 3-7 to 3-10). The diagnostic impact of weight-bearing views can be substantial (Fig. 3-11). Depending upon clinical context, a limited number of additional views may be warranted. 1. Ankle impingement: Lateral dorsiflexion or plantar-flexion views (Fig. 3-12); “lazy” lateral view (Fig. 3-13) 2. Talocalcaneal coalition: Harris-Beath view (Fig. 3-14), oblique views (Fig. 3-15), Brodén views (Fig. 3-16) 3. Trauma: AP view of proximal fibula if Maisonneuve fracture suspected (Fig. 3-17); reverse oblique view of ankle if medial malleolus fracture suspected (Fig. 3-18) 4. Ankle instability: Stress views of ankle joint (Figs. 3-19 and 3-20); stress view of distal tibiofibular syndesmosis (Fig. 3-21) 5. Heel: Lateral and axial views of calcaneus (Fig. 3-22) 6. Navicular: Navicular view (Fig. 3-23) 7. Talus: Talar neck view (Fig. 3-24). 8. Tarsometatarsal joints or base of second metatarsal: Plantar-dorsal projection of midfoot (Fig. 3-25) 9. Toes: Lateral and lateral-oblique phalangeal views (Fig. 3-26) 10. Sesamoids: Axial, medial-oblique, lateromedial, and stress views of sesamoids (Figs. 3-27 to 3-30). Common radiographic measurements used to assess foot deformities are shown in Figures 3-31 to 3-37. However, the significance of any apparent radiographic abnormality should always be weighed in the overall clinical context because radiographic measurements are subject to a wide range of normal variation and are also susceptible to error through poor radiographic technique. The advantages of US include low cost, patient comfort, an absence of hazardous ionizing radiation, the clinically interactive nature of the test (Fig. 3-38), the ability to assess tissue dynamics such as tendon glide and stability (Fig. 3-39), the ability of Doppler techniques to detect soft tissue hyperemia and neovascularity (Fig. 3-40), and the ability to guide diagnostic and/or therapeutic injections accurately (Fig. 3-41). The clinical aspect of directly probing the visualized anatomy with an US transducer allows the operator to accurately correlate any site(s) of pain and/or tenderness with the imaging appearance. This has been described as “sonopalpation” and can be very helpful in confirming a symptomatic structure or clinically relevant finding. Similarly, the demonstration of locally increased tissue vascularity using Doppler techniques serves to increase the likelihood of a gray-scale finding being relevant to symptoms.62 The limitations of US include an inability to see through bone/gas/metal, image quality degraded by obesity and marked subcutaneous edema, reduced resolution and sensitivity at tissue depths greater than 3 cm, the local availability of a reliable and well-trained operator, the “keyhole” nature of images that may be difficult for the surgeon to orient and understand, and image artifacts that can limit visualization of some tendon segments or be a diagnostic pitfall for the inexperienced (Fig. 3-42). US is well suited to the assessment of many superficial tendons and ligaments (Figs. 3-43 and 3-44), foreign bodies, ganglion cysts (Fig. 3-45), and other superficial masses (Fig. 3-46; see Fig. 3-38). In addition, because metal does not distort the sonographic image, US is a good alternative to MRI for the assessment of soft tissue structures adjacent to orthopedic hardware (Fig. 3-47).
Imaging of the Foot and Ankle
Role of Imaging
Effective Use of Imaging
Radiation Safety
Average U.S. background radiation/yr
3.0 mSv
Single trans-Atlantic flight
0.04 mSv
Radiograph: chest (PA)
0.02 mSv
Radiograph: foot (single exposure)
0.001 mSv
Computed tomography: ankle
0.07 mSv
Isotope (Tc-99m–MDP) bone scan
6.3 mSv
Radiographs
Ultrasound
Use of Ultrasound
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Imaging of the Foot and Ankle