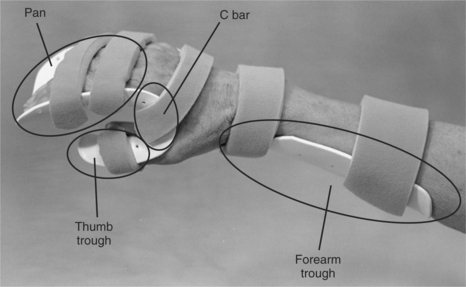
CHAPTER 9 1 List diagnoses that benefit from resting hand splints (hand immobilization splints). 2 Describe the functional or mid-joint position of the wrist, thumb, and digits. 3 Describe the antideformity or intrinsic-plus position of the wrist, thumb, and digits. 4 List the purposes of a resting hand splint (hand immobilization splint). 5 Identify the components of a resting hand splint (hand immobilization splint). 6 Explain the precautions to consider when fabricating a resting hand splint (hand immobilization splint). 7 Determine a resting hand (hand immobilization) splint-wearing schedule for different diagnostic indications. 8 Describe splint-cleaning techniques that address infection control. 9 Apply knowledge about the application of the resting hand splint (hand immobilization splint) to a case study. 10 Use clinical judgment to evaluate a fabricated resting hand splint (hand immobilization splint). Physicians commonly order resting hand splints, also known as hand immobilization splints [American Society of Hand Therapists 1992] or resting pan splints. A resting hand splint is a static splint that immobilizes the fingers and wrist. The thumb may or may not be immobilized by the splint. Therapists fabricate custom resting hand splints or purchase them commercially. Some of the commercially sold resting hand splints are prefabricated, premolded, and ready to wear.Table 9-1 outlines prefabricated splints for the wrist and hand. Others are sold as precut resting hand splint kits that include the precut thermoplastic material and strapping mechanism. Each of these splints has advantages and disadvantages. Table 9-1 A resting hand splint kit typically contains strapping materials and precut thermoplastic material in the shape of a resting hand splint. Kits are available according to hand size (i.e., small, medium, large, and extra large). An advantage of using a kit is the time the therapist saves by elimination of pattern making and cutting of thermoplastic material. Similar to premolded splints, precuts from perforated materials contain perforations in only the body of the splint. Precuts are interchangeable for right or left extremity application. The therapist has control over joint positioning. A disadvantage is that the pattern is not customized to the person. Therefore, the precut splint may require many adjustments to obtain a proper fit. A therapist can customize a resting hand splint by making a pattern and fabricating the splint from thermoplastic material. The advantage is an exact fit for the person, which increases the splint’s support and comfort. The therapist also has control over joint positioning. A disadvantage is that customization may require more of the therapist’s time to complete the splint and may be more costly. In addition, when a resting hand splint pattern is cut out of perforated thermoplastic material it is difficult to obtain smooth edges because of the likelihood of needing to cut through the perforations (which causes a rough edge). Commercially available products such as the Rolyan Aquaplast UltraThin Edging Material can be applied over the rough edges to help create a smooth-edged reinforcement on splints fabricated from Aquaplast materials [Sammons Preston Rolyan 2005]. Therapists must make informed decisions about whether they will fabricate or purchase a splint. Many products are advertised to save time and to be effective, but few studies compare splinting materials when used by therapists with the same level of experience [Lau 1998]. Lau [1998] compared the fabrication of a resting hand splint with use of a precut splint, the QuickCast (fiberglass material) with Ezeform thermoplastic material. The study employed second-year occupational therapy students as splintmakers and first-year occupational therapy students as their clients. The resting hand splint has three purposes: to immobilize, to position in functional alignment, and to retard further deformity [Malick 1972, Ziegler 1984]. When inflammation and pain are present in the hand, the joints and surrounding structures become swollen and result in improper hand alignment. The resting hand splint may retard further deformity for some persons. The therapist may provide a splint for a person with arthritis who has early signs of ulnar drift by placing the hand in a comfor table neutral position with the joints in mid-position. Rest through immobilization reduces symptoms. Joints that are receptive to proper positioning may allow for optimal maintenance of range of motion (ROM) [Ziegler 1984]. The therapist must know the splint’s components to make adjustments for a correct fit. Four main components comprise the resting hand splint: the forearm trough, the pan, the thumb trough, and the C bar (Figure 9-5) [Fess et al. 2005]. Figure 9-5 The components of a resting hand splint are the forearm trough, pan, thumb trough, and C bar. Forearm troughs can be volarly or dorsally based. The volarly based forearm trough at the proximal portion of the splint supports the weight of the forearm. Dorsally based forearm troughs are located on the dorsum of the forearm. The therapist should apply biomechanical principles to make the trough about two-thirds the length of the forearm to distribute pressure of the hand and to allow elbow flexion when appropriate. The width should be one-half the circumference of the forearm. The proximal end of the trough should be flared or rolled to avoid a pressure area. When a great amount of forearm support is desired, a volarly based forearm trough is the best design (Figure 9-6). When the volar surface of the forearm must be avoided because of sutures, sores, rashes, or intravenous needles, a dorsally based forearm trough design is frequently used (Figure 9-7). Dorsally based troughs can be a helpful design for applying a resting hand splint to a person with hypertonicity. The forearm trough can be used as a lever to extend the wrist in addition to extending the fingers. The thumb trough supports the thumb and should extend approximately ½ inch beyond the end of the thumb. This extension allows the entire thumb to rest in the trough. The width and depth of the thumb trough should be one-half the circumference of the thumb, which typically should be in a palmarly abducted position. The therapist should attempt to position the carpometacarpal (CMC) joint in 40 to 45 degrees of palmar abduction [Tenney and Lisak 1986] and extend the thumb’s interphalangeal (IP) and metacarpal joints. The C bar keeps the web space of the thumb positioned in palmar abduction. If the web space tightens, it inhibits cylindrical grasp and prevents the thumb from fully opposing the other digits. From the radial side of the splint, the thumb, the web space, and the digits should resemble a C (seeFigure 9-6). To rest the wrist and hand joints, the resting hand splint positions the hand in a functional or mid-joint position [Colditz 1995] (Figure 9-8). According to Lau [1998, p. 47], “The exact specifications of the functional position of the hand in a resting hand splint and the recommended joint positions vary.” One functional position that we suggest places the wrist in 20 to 30 degrees of extension, the thumb in 45 degrees of palmar abduction, the metacarpophalangeal (MCP) joints in 35 to 45 degrees of flexion, and all proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints in slight flexion. The antideformity position is often used to place the hand in such a fashion as to maintain a tension/distraction of anatomic structures to avoid contracture and promote function. The antideformity position places the wrist in 30 to 40 degrees of extension, the thumb in 40 to 45 degrees of palmar abduction, the thumb IP joint in full extension, the MCPs at 70 to 90 degrees of flexion, and the PIPs and DIPs in full extension (Figure 9-9). Several diagnostic categories may warrant the provision of a resting hand splint. Persons who require resting hand splints commonly have arthritis [Egan et al. 2001, Ouellette 1991]; postoperative Dupuytren’s contracture release [Prosser and Conolly 1996]; burn injuries to the hand, tendinitis, hemiplegic hand [Pizzi et al. 2005]; and tenosynovitis [Richard et al. 1994]. The resting hand splint maintains the hand in a functional or antideformity position, preserves a balance between extrinsic and intrinsic muscles, and provides localized rest to the tissues of the fingers, thumb, and wrist [Tenney and Lisak 1986]. Although hand immobilization splints are commonly used, a paucity of literature exists on their efficacy. Thus, it is a ripe area for future research. Therapists should consider the resting hand splint as a legitimate intervention for appropriate conditions despite the lack of evidence. Therapists often provide resting hand splints for people with rheumatoid arthritis (RA) during periods of acute inflammation and pain [Biese 2002, Ziegler 1984] and when these people do not use their hands for activities but require support and immobilization [Leonard 1990]. The biomechanical rationale for splinting acutely inflamed joints is to reduce pain by relieving stress and muscle spasms. However, it may not additionally prevent deformity [Biese 2002, Falconer 1991]. Typical joint placement for splinting a person with RA positions the wrist in 10 degrees of extension, the thumb in palmar abduction, the MCP joints in 35 to 45 degrees of flexion, and all the PIP and DIP joints in slight flexion [Melvin 1989]. For a person who has severe deformities or exacerbations from arthritis, the resting hand splint may also position the wrist at neutral or slight extension and 5 to 10 degrees of ulnar deviation [Geisser 1984, Marx 1992]. The thumb may be positioned midway between radial and palmar abduction to increase comfort. These joint angles are ideal. Therapists use clinical judgment to determine what joint angles are positions of comfort for splinting. Note that wrist extension varies from the typical 30 degrees of extension. When the wrist is in slight extension, the carpal tunnel is open—as opposed to being narrowed, with 30 degrees of extension [Melvin 1989]. Finger spacers may be used in the pan to provide comfort and to prevent finger slippage in the splint [Melvin 1989]. Melvin [1989] cautions that finger spacers should not be used to passively correct ulnar deformity because of the risk for pressure areas. In addition, once the splint is removed there is no evidence that splint wear alters the deformity. However, it may prevent further deformity. In persons who have RA, the use of splints for purposes of rest during pain and inflammation is controversial [Egan et al. 2001]. Periods of rest (three weeks or less) seem to be beneficial, but longer periods may cause loss of motion [Ouellette 1991]. Phillips [1995] recommended that persons with acute exacerbations wear splints full-time except for short periods of gentle ROM exercise and hygiene. Biese [2002] recommended that persons wear splints at night and part-time during the day. In addition, persons may find it beneficial to wear splints at night for several weeks after the acute inflammation subsides [Boozer 1993]. When splinting a joint with chronic RA, the rationale is often based on biomechanical factors. According to Falconer [1991, p. 83], “Theoretically, by realigning and redistributing the damaging internal and external forces acting on the joint, the splint may help to prevent deformity __or improve joint function and functional use of the extremity.” Therapists who splint persons with chronic RA should be aware that prolonged use of a resting hand splint may also be harmful [Falconer 1991]. Studies on animals indicate that immobilization leads to decreased bone mass and strength, degeneration of cartilage, increase in joint capsule adhesions, weakness in tendon and ligament strength, and muscle atrophy [Falconer 1991]. In addition to splint intervention, persons with RA benefit from a combination of management of inflammation, education in joint protection, muscle strengthening, ROM maintenance, and pain reduction [Falconer 1991, Philips 1995]. Persons in late stages of RA who have skeletal collapse and deformity may benefit from the support of a splint during activities and at nighttime [Biese 2002, Callinan and Mathiowetz 1996]. Compliance of persons with RA in wearing resting hand splints has been estimated at approximately 50% [Feinberg 1992]. The degree to which a person’s compliance with a splint-wearing schedule affects the disease outcome is unknown. However, research indicates that some persons with RA who wore their splints only at times of symptom exacerbation did not demonstrate negative outcomes in relation to ROM or deformities [Feinberg 1992]. For persons who have hand burns, therapists do not splint in the functional position. Instead, the therapist places the hand in the intrinsic-plus or antideformity position (seeFigure 9-9). Richard et al. [1994] conducted an in-depth literature review to find a standard dorsal hand burn splint design. The literature cited 43 splints to position the dorsally burned hand joints. Twenty-six of these splints were labeled as antideformity splints and 17 were identified as having a position of function. Thus, a wide range of designs exists for splinting dorsal hand burns [Richard et al. 1994]. The antideformity position for a palmar or circumferential burn places the wrist in 30 to 40 degrees of extension and 0 degrees (i.e., neutral) for a dorsal hand burn. For dorsal and volar burns, the therapist should flex the MCPs into 70 to 90 degrees, fully extend the PIP joints and DIP joints, and palmarly abduct the thumb to the index and middle fingers with the thumb IP joint extended [Salisbury et al. 1990]. After a burn injury, the thumb web space is at risk for developing an adduction contracture [Torres-Gray et al. 1996]. Therefore, palmar abduction of the thumb is the position of choice for the thumb CMC joint. The emergent phase is the first 48 to 72 postburn hours [deLinde and Miles 1995]. During this time frame, dorsal edema occurs and encourages wrist flexion, MCP joint hyperextension, and IP joint flexion [deLinde and Miles 1995]. Static splinting is initiated during the emergent phase to support the hand and maintain the length of vulnerable structures [deLinde and Miles 1995]. Positioning to counteract the forces of edema includes placing the wrist in 15 to 20 degrees of extension, the MCP joints in 60 to 70 degrees of flexion, and the PIP and DIP joints in full extension, with the thumb positioned midway between palmar and radial abduction and with the IP joint slightly flexed [deLinde and Miles 1995]. For children with dorsal hand burns, during the emergent phase the MCP joints may not need to be flexed as far as 60 to 70 degrees. deLinde and Knothe [2002] suggested that for children under the age of three therapists may not need to splint unless it is determined that the wrist requires support. If a child is age three or older, splinting should be considered. Young children who have burned hands may not need splints because the bulky dressings applied to the burned hand may provide adequate support. A prefabricated resting hand splint in an antideformity position can be applied if a therapist cannot immediately construct a custom-made splint [deLinde and Miles 1995]. deLinde and Miles [1995] suggested that prefabricated splints may be appropriate for superficial burns with edema for the first three to five days. For full-thickness burns with excessive edema, custom-made splints are necessary [deLinde and Miles 1995]. A splint applied in the first 72 hours after a burn may not fit the person 2 hours after application because of the significant edema that usually follows a burn injury. The therapist should closely monitor the person to make necessary adjustments to the splint. When fabricating a custom splint for a person with excessive edema, a therapist should avoid forcing wrist and hand joints into the ideal position and risking ischemia from damaged capillaries [deLinde and Miles 1995]. With edema reduction, serial splinting may be necessary as ROM is gained to splint toward the ideal position. Serial resting hand splints for persons with burns should conform to the person, rather than conforming the person to the splints [deLinde and Miles 1995]. Persons with hand burns have bandages covering burn sites. According to Richard et al. [1994, p. 370], “As layers of bandage around the hand increase, accommodation for the increased bandage thickness must be accounted for in the splint’s design, if it is to fit correctly.” To correct for bandage thickness on a resting hand splint, the bend corresponding to MCP flexion in the pan should be formed more proximally [Richard et al. 1994]. The initial splint provision for a person with hand burns should be applied with gauze rather than straps. This reduces the risk of compromising circulation. Splints on adults should be removed for exercise, hygiene, and appropriate functional tasks. For children, splints are removed for exercise, hygiene, and play activities [deLinde and Miles 1995].
Hand Immobilization Splints
THERAPEUTIC OBJECTIVE
DESCRIPTION
Resting hand splints immobilize the wrist, thumb, and metacarpophalangeal (MCP) joints to provide rest and reduce inflammation. The proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints are free to move for functional tasks.
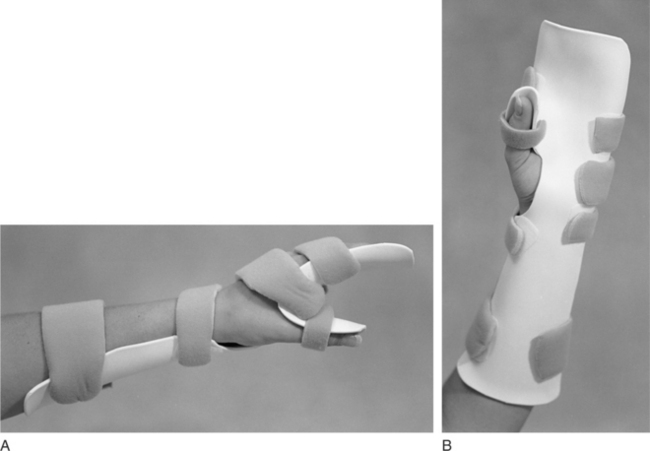
Similar to the resting hand splint design, splints can provide rest to the wrist, thumb, and MCP joints (Figure 9-1). Padding and strapping systems can help control deviation of wrist and MCPs. Splints are available in different sizes for the right and left hands.
Design to optimally position the hand in an intrinsic-plus position after a burn injury.
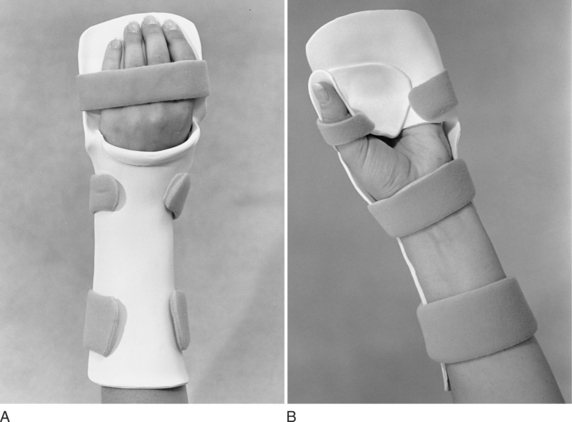
Burn resting hand splints typically position the wrist in 20 to 30 degrees of extension, the MCP joints in 60 to 80 degrees of flexion, the PIP and DIP joints in full extension, and the thumb midway between radial and palmar abduction (Figure 9-2).
Several splints are designed to reduce spasticity.
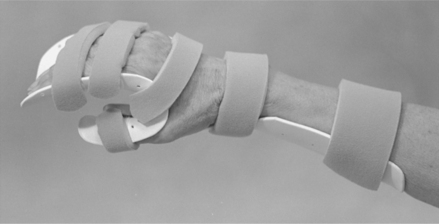
Ball splints implement a reflex-inhibiting posture by positioning the wrist in neutral (or slight extension) and the fingers in extension and abduction. Cone splints combine a hand cone and a forearm trough, which maintains the wrist in neutral, inhibits the long finger flexors, and maintains the web space (Figure 9-3).
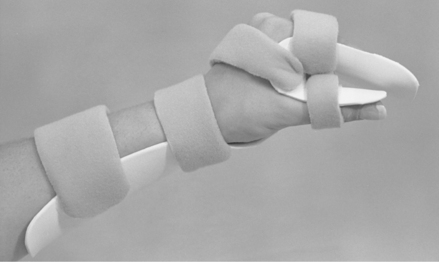
A resting hand splint positioning the hand in a functional position is also advocated for spasticity (Figure 9-4).
Precut Splint Kits
Customized Splints
Purpose of the Resting Hand Splint
Resting Hand Splint Positioning
Functional Position
Antideformity Position
Diagnostic Indications
Rheumatoid Arthritis
Acute Rheumatoid Arthritis
Chronic Rheumatoid Arthritis
Hand Burns
Emergent Phase
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hand Immobilization Splints