Fig. 32.1
Supracondylar humeral fracture
Supracondylar fractures are divided into displaced and undisplaced injures. Undisplaced fractures can be treated non-operatively with immobilisation in an above elbow cast or splint [2]. The Cuomo case series includes all consecutively enrolled patients, and documents 100 % treatment success with posterior splinting. Case series are more valid if patients are enrolled consecutively and fully accounted for, and are most useful in assessing 100 % or 0 % outcomes (‘penicillin and parachutes’ studies).
Closed reduction and percutaneous pinning (CRPP) of displaced fractures yields predictable results with the fewest complications when compared to alternatives such as closed reduction and cast immobilisation or traction. Pirone’s classic retrospective comparative study published in 1988 compared 4 methods of management; closed reduction and casting (130 patients), closed reduction and percutaneous K-wire fixation (78 patients), traction (15 patients), and open reduction with internal fixation (7 patients). Of the 130 patients managed in cast, 29 had conversion to K-wire fixation due to circulatory problems experienced due to hyperflexion of the elbow, 14 had varus malunion, 6 had reduced range of movement and 1 patient developed Volkmann’s ischaemic contracture. In the group managed with K-wire fixation there were 3 varus malunions and 2 patients who experienced loss of motion. Despite several patients who had initially absent radial pulse with a well-perfused hand, no patient in the K-wire group developed Volkmann’s ischaemic contracture. Approximately half had all lateral wires, and half crossed pins, there were no pin-related nerve complications but there were 2 pin infections. At final follow-up 78 % of patients managed with K wires had both carrying angle and range of motion within 5° of the contralateral side, compared to 51 % of the group treated with cast [3]. Although this study has some potential for bias (better, or worse patients may have been selected for the new technique of closed pinning so results may indicate patient selection rather than treatment effectiveness), the differences in important outcomes were compelling and all favoured closed reduction and pinning, which was increasingly adopted following the results of this influential paper. Given the harm (ischemic contracture, malunion) documented in the closed reduction and cast group, it is impractical to propose a randomized trial comparing these treatments at present.
There is a grey zone regarding the management of minimally displaced Gartland type 2 injuries. Care should be taken particularly in those fractures that have medial comminution and/or initial varus displacement. This pattern of injury can be more unstable than the initial radiographs suggest leading to medial collapse and varus malunion if managed non-operatively [4, 5]. A retrospective review of 189 type 2 supracondylar humerus fractures managed operatively concluded that following CRPP there was a high probability of satisfactory outcome with a low complication rate (4 pin tract infections, no loss of reduction) [6]. The American Academy of Orthopaedic Surgeons (AAOS) [7] guidelines of the treatment of paediatric supracondylar humerus fractures advise that all Gartland type 2 and 3 fractures be managed with CRPP. This management is supported by the practice at our institution as well as others [5, 8].
There has been debate regarding the most appropriate placement of percutaneous pins. Initial descriptions of percutaneous pinning techniques described crossed pins inserted through medial and lateral entries, whereas recent literature emphasizes the importance of all-lateral pinning constructs in avoiding iatrogenic injury to the ulnar nerve. Excellent outcomes have been reported with all lateral pins that are placed in a bi-cortical fashion that avoid crossing, and give adequate spread at the fracture site [9]. Kocher published a small randomized trial showing no difference in outcome between crossed or lateral entry pins either from displacement or ulna nerve injury [10], but the trial was underpowered to detect differences in ulnar nerve injury which is a rare outcome. A systematic review in 2007 reported an iatrogenic nerve injury rate of 1.9 % in all lateral pins and 3.5 % for crossed pins with a loss of reduction of 0.7 % in lateral entry pins and 0 % in crossed pins [11]. A further meta-analysis in 2012 [12] showed a 4.3 times greater risk of ulna nerve injury with crossed pins. Others showed a decrease in ulna nerve injury of 15–2 % by using all lateral pins with selective use of a medial pin if the fracture was deemed unstable [13]. Well placed all lateral insertion of pins yield a construct that is ‘strong enough’ to prevent displacement and avoids the higher risk of iatrogenic ulna nerve injury. The British Orthopaedic Association Standards for Trauma (BOAST) guidelines advise that 2 mm diameter wires should be used where possible [14]. The AAOS guideline carefully considered all of the published literature reporting on pin placement and nerve outcomes. Both case series and comparative studies were used to provide the most robust estimate of ulnar nerve lesions from medial pin placement. The pooled estimated was a 6 % risk of iatrogenic ulnar nerve injury (49 of 808 patients in published series) and this was sufficient for AAOS to recommend stabilization of displaced supracondylar fractures with two or three laterally inserted wires [7]. Language in the guideline permits the use of medial wires if the specific fracture anatomy cannot be adequately stabilized with lateral pins only – this may occur, for example, if an oblique fracture line runs from proximally medially to distally laterally.
There is a wide variation across the literature regarding the need for open reduction suggesting that we do not yet have a clear statement on what can be called an acceptable reduction. Routine open reduction has been shown to cause increased stiffness at 2-year follow-up and is not advised [15]. There is limited evidence to suggest that using open reduction techniques will improve reduction [7]. Fracture, surgeon, and hospital factors are taken into account and it is possible that a low rate of open reduction, seen in higher volume centres, is not as attainable or desirable in lower volume practices. In evaluating the results of a reduction all would agree that anatomical reduction, if attainable, is optimal. Varus malunion, so called gunstock deformity must be avoided as this is cosmetically unacceptable to many patients and is the most common reason for revision operation. Small amounts of medial and lateral translation, anterior or posterior translation, or angulation in the sagittal plane may be consistent with perfect functional results, but one of the biggest gaps in the literature is clear information about what position short of anatomic reduction is acceptable (Fig. 32.2).


Fig. 32.2
Deformities after supracondylar humeral fractures. Top images: extension deformity of the distal humerus. Bottom left: valgus deformity of the distal humerus. Bottom right: varus deformity of the distal humerus (often called gunstock deformity)
Neither the BOAST nor the AAOS guidelines are able advise on out of hours surgical intervention unless there are indications for urgent surgery. These indications include absent radial pulse, clinical signs of impaired perfusion of the hand and evidence of threatened skin viability [7, 14]. A retrospective study in 2001 showed that supracondylar fractures operated within 8 h had no difference in outcome with regard to conversion to open reduction, pin track injections or iatrogenic nerve injury compared to those operated on after 8 h from injury [16]. Other groups support these findings, with one retrospective study also showing no differences in quality of reduction once united [17, 18]. One study did show an increased need for open reduction when fractures were operated on after 8 h, 33 % open reduction rate in 45 patients. They also had a higher than usual requirement for open reduction for those operated within 8 h, 11.2 % of 126 patients, which brings into question their threshold for open reduction, and whether this is a suitable outcome measure [19]. The BOAST guidelines suggest that supracondylar fractures without indications for urgent surgery require early surgical treatment, ideally on the day of admission but not during the night. This practice is supported in our institution.
Injuries with vascular compromise, specifically those with an absent radial pulse can be divided into two distinct groups. One is the pale, cold pulse-less limb that does not improve after reduction; this type of injury should be explored and the brachial artery identified and repaired if necessary. The second is the perfused pulse-less hand, specifically an absent radial pulse with good capillary refill, good skin colour, and a warm extremity. There is mixed literature on this subject, with two series reaching opposite conclusions from similar clinical data. One study explored all injuries with a pink pulseless hand [20], the other managed all with observation [21]; in both cases patients did well, with no circulatory problems at follow-up. Another study divided cases into those that were explored and had vascular repair, and those that were managed expectantly. At follow-up ten patients were imaged using magnetic resonance angiography, five showed occlusion or re-stenosis of the brachial artery despite repair, all had a radial pulse present [22]. BOAST guidelines suggest that a perfused limb does not require brachial artery exploration whether or not the radial pulse is present. For those injures where the limb remains ischemic after fracture reduction, a surgeon competent to perform small vessel vascular repair should explore the brachial artery [14].
The majority of associated nerve injuries in supracondylar fractures are transient neurapraxias that can be managed expectantly. It is worth considering that if there is neurological compromise pre-operatively and it is not possible to achieve a perfect reduction, then the nerve may be lodged in the fracture site. If there is suspicion of an iatrogenic nerve injury, any medially placed wire should be removed, and consideration should be given to surgical exploration [14].
The duration of immobilisation following percutaneous pinning varies in the literature. The AAOS drew inconclusive recommendations on the optimal time for pin removal and mobilisation. In our institution pins are removed at 3 weeks, and children are allowed to mobilise as tolerated. Physiotherapy is not routinely used in our institution. The AAOS guidelines were unable to recommend either for or against the use of physical therapy as there are no high quality studies documenting any long-term benefit of the intervention. The rapid and near complete return of range of motion experienced by most children suggests that the role of physical therapy might be restricted to the small number of patients who have persistent stiffness a few weeks after pin removal.
The AAOS guideline on paediatric supracondylar fractures was created because this is such a common fracture with the potential for significant associated injuries, and significant complications. The guideline supports closed reduction for displaced fractures, with percutaneous pinning using two or three lateral entry pins. AAOS applies strict criteria to the inclusion and evaluation of evidence with a consistent approach for all the guidelines it creates [23]. An initial meeting of a clinical panel is used to carefully define 15 key questions, which will produce the recommendations. Clinicians from academic and community practices and from all specialties involved in the care are represented. Expert methodologists guide the process of guideline development. Trained methodologists and medical librarians do literature searches and abstraction. Only the highest level of evidence is considered in formulating a particular recommendation however both quality and quantity criteria apply – so, for example, a small underpowered but randomized trial will not exclude the consideration of larger retrospective studies. The literature review document for this guideline, prepared by the methodologists, ran to some 1200 pages and included 1726 citations, with 1682 articles finally excluded, leaving 44 to be considered for the recommendations [7]. Novel meta-analyses were performed for some questions including the rate of ulnar nerve injury from medial placement of pins. A second meeting of the clinical panel confirmed the application of the literature review to the answers to clinical questions. Level of evidence and quality of evidence are both considered in determining the strength of a particular recommendation. For many sensible clinical questions, there simply is not enough evidence to make evidence based recommendations and an inconclusive statement is required. An exception is in the case of potential life or limb outcomes, in which case a consensus recommendation is permitted – as in the case of a vascular injury. The advantage of adhering strictly to process is that the guideline itself should be without bias. The potential for practice guidelines to be either biased or conflicting has been demonstrated in, for example, discrepancies in recommendations regarding thromboprophylaxis generated by orthopaedic surgeons versus haematologists versus chest physicians working from the same literature [24]. A disadvantage of a strict adherence to methodology is that the resulting guideline may be seen as predictable, unremarkable, indecisive, or difficult to use in the clinical setting. AAOS has addressed this disadvantage by creating appropriate use criteria (AUCs) for supracondylar fractures based on the guideline [7] (Fig. 32.3). An AUC is a web-based tool designed for easy application. The clinical scenario is input into the tool, and the tool presents treatments with a rating of how appropriate each treatment is for that particular situation. The appropriateness is based on a clinical panel voting explicitly on how the guideline applies to that clinical setting. Clinicians should resist the temptation to read and apply individual studies in isolation now that systematic summaries of the literature exist.
Fig. 32.3
The AAOS clinical practice guideline. The AAOS clinical practice guideline has been turned into an appropriate use criteria or AUC as shown here. The user can select a combination of clinical circumstances, and view treatment recommendations considered most appropriate by an expert panel applying the guideline to each situation
Lateral Condyle Fractures
Lateral condyle fractures can be difficult to diagnose and have a propensity for late displacement. Compared to other paediatric fractures they have a higher risk of non-union, which, if allowed to occur can result in progressive valgus deformity of the elbow and tardy ulna nerve palsy (Fig. 32.4).
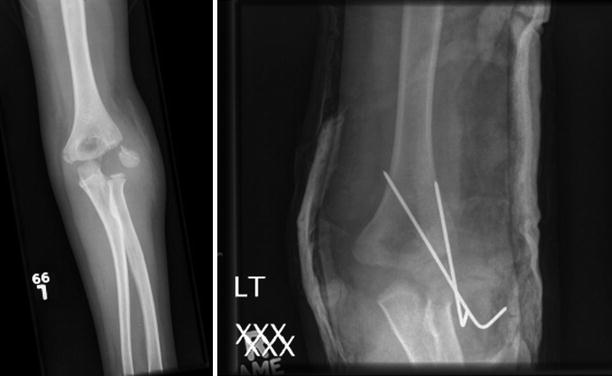
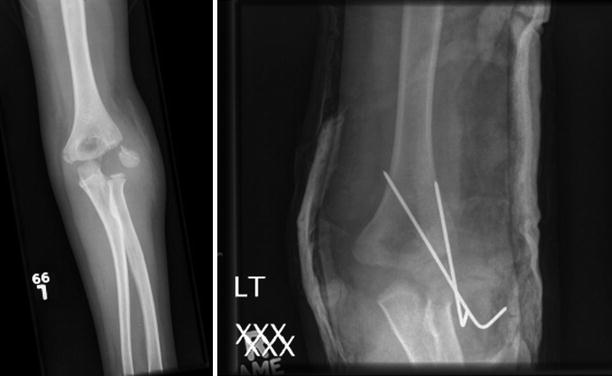
Fig. 32.4
Lateral condyle fracture of the elbow
An internal oblique radiograph is the most sensitive view to ascertain the displacement of a lateral condyle fracture of the elbow. This was shown in a prospective cohort of 54 patients where 70 % of patients were noted to have different amounts of displacement of the fracture on an internal oblique view compared to standard antero-posterior and lateral images [25]. For undisplaced or minimally displaced fractures MRI studies can be useful to determine the stability of the fracture. A prospective cohort of 16 patients was imaged with both radiographs and MRI. There were 12 patients who had radiographically unstable (>3 mm displacement) lateral condyle fractures; of these 10 had an intact articular cartilage hinge, none of these displaced, of the 2 who had disrupted articular cartilage, one displaced [26]. Studies regarding the management of ‘undisplaced’ fractures (less than 2 mm displacement on internal oblique view) have shown mixed reports. One retrospective comparative series showed poor result with cast immobilisation alone; of the 17 patients 5 displaced, 4 required later surgery, 2 malunited and 2 went on to non-union. For the 13 treated with open K-wire stabilisation, 2 lost reduction and malunited [27]. Conversely a large case series reported 95 non-operatively managed lateral condyle fractures that had <2 mm initial displacement; 93 healed and only 2 displaced then went on to unite when treated with open reduction and K wire fixation [28]. Neither of these studies used MRI in their diagnostic algorithm. MRI may have supplied further prognostic information regarding the stability of the fracture and some explanation for the discrepancy in their findings.
It is well reported that displaced lateral condyle fractures require accurate reduction, usually open, then fixation. A biomechanical study showed that greater than 60° divergent pins yielded better stability than parallel pins [29]. Screw fixation is an alternative to pin fixation, which is, advocated in some case series however there is inadequate comparative information to recommend one over the other. Screw fixation has been shown to have increased biomechanical stability in synthetic bone [30]. However a comparative cohort study comparing 44 patients managed with screw osteosynthesis and 33 patients managed with K-wires found that K-wire fixation had comparatively similar outcomes to screw fixation, with no fracture going on to non-union in either group [31]. In our institution patients are usually immobilised postoperatively for 3 weeks then examined clinically and radiographically following pin removal. The rate of non-union after 3 weeks of pin fixation was 1 in a consecutive series of 104 patients [32].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







