Fig. 43.1
This 13 old boy with a simple bone cyst of the humerus had 5 pathological fractures over 5 years and the cyst did not heal

Fig. 43.2
A simple bone cyst caused pathological fracture and subsequent growth arrest at the right distal femur physis
Do Simple Bone Cysts Heal Spontaneously After a Pathological Fracture?
A simple bone cyst seldom heals after a pathological fracture. While abundant callous may initially form, it tends to resorb after 6 months and there is a low likelihood of the cyst healing following a fracture (Fig. 43.3). Garceau and Gregory [58] showed a 15 % healing rate after a fracture. Others found less than 5 % [59–61]. Moreover, Neer [44] found 70 % of the cysts developed another fracture within 2 years.
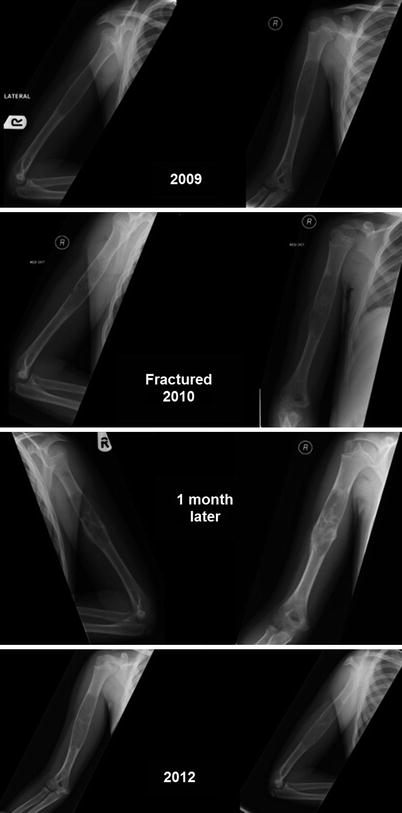
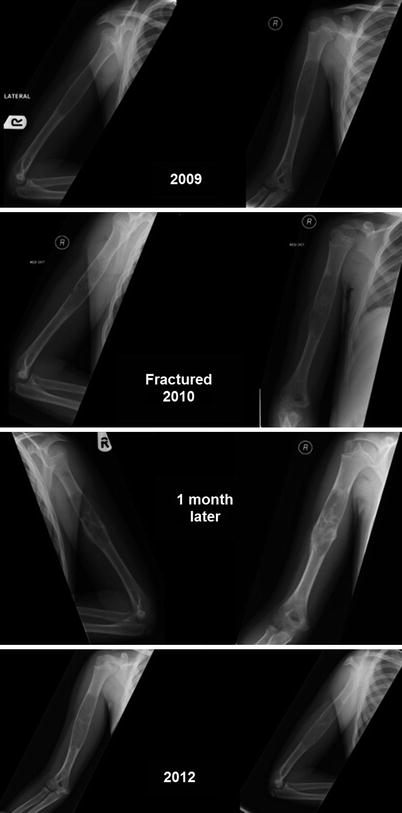
Fig. 43.3
This young boy was treated non-operatively for simple bone cyst. He had a pathological fracture in January 2010. After a month, plain x-ray showed the cyst was filling with bone; however, the cyst was larger after a year (see also Fig. 43.7)
Can We Predict Simple Bone Cysts that Could Cause Problems Such as Fractures or Deformities?
Researchers have been trying to identify patients and/or cyst features that predict outcomes in SBC. Several factors were investigated including but not limited to the size and site of the cyst, symptoms, previous fractures, patients’ age, sex, types of interventions and length of follow-up. The literature is contradictory on virtually all these prognostic factors. Issues included definition of prognostic factors, duration of follow-up (cyst often recurs after signs of initial healing), definition of healing, lack of multivariate analysis and lack of blinding.
Kaelin and MacEwen [50] found that the larger the cyst, the more cortex was destroyed and the bone weakened. To quantify the strength of the remaining cortex, which is related to the size of the cyst and the size of the involved bone, they devised the cyst index. This gives the proportion between the radiographic area of the cyst and the size of the involved bone, measured as the diameter of the diaphysis squared:
Cyst Index = Area of the cyst/Diaphysis diameter2
A low cyst index indicates a small cyst area in relation to the bone; conversely, a high index indicates a large cyst. The smallest cyst in their series was measured 0.1, the largest 12.78. Recent pathological fractures were found in 53 radiographs and the cyst index was measured in each. The average index in humeral fractures was 6.12 (SD = 1.8) and in femoral fractures 4.74 (SD = 1.19). The humeral index is higher because these fractures occurred later than those in the lower limb.
Before the first fracture, the children are normally active, but once the diagnosis is made activity is often reduced, and for a subsequent fracture the trauma is likely to be less than in the first instance. The index would then be larger, and the results confirmed this hypothesis. However, as discussed below the change in cyst index could be due to the natural history of the cyst and/or reaction to the fracture.
In 21 initial fractures through humeral cysts, the average index was 5.38 (SD = 1.02), and in 14 recurrent fractures the index was 7.38 (SD = 2.4) which was a significant difference (P < 0.005). Interestingly it was shown that the cyst index does not show any tendency towards regression after a fracture, in fact the cyst often continues to grow in parallel to the healing process. In these cases the slope of the increase remained in the same range as before fracture, showing a rise of about two points a year. Thus a fracture did not change the natural course of the development of a cyst. Kaelin reported that there were no fractures in 40 patients who had an index lower than 3.5 and who did not curtail their activities.
In all 57 included patients, Kaelin found no further increase in the index occurred after its spontaneous. Cysts with at least two consecutive decreased indices of <3 and a cortical wall thicker >2 mm are considered to be healed. When these conditions are present, fractures never occur and the result is always favourable.
A recent study questioned the reliability of the cyst index as a predictor of fracture [62]. The cyst index of 32 femoral and humeral SBCs was determined by 8 reviewers. The risk group cyst index was compared with whether a fracture took place. Sensitivities, specificities, and positive and negative predictive values were calculated across varying cutoff levels. Intra-observer and inter-observer reliability testing for 10 cysts was also made. The mean value for the cyst index was significantly different for different observers (P < 0.05). The sensitivities, specificities, and positive and negative predictive values were small; particularly for the femoral cysts (0.5, 0.33, 0.33 and 0.50 respectively). The study conclusion did not validate the cyst index to be an accurate predictor of fracture. One significant weakness of the study was the short follow-up of 1.4 years.
Ahn and Park [59] carried out a retrospective review of 75 children with SBC to determine which cysts were likely to be at risk and whether healing was accelerated after a fracture. They found the percentage of bone occupied by the cyst in the transverse plane was more than 85 % in both AP and lateral radiographs in every case of pathological fracture. In most cases, the cyst recurred and sometimes became large without any acceleration of healing after fracture.
In another study, Leong et al. [63] investigated the use of quantitative computed tomography-based structural analysis to predict fractures in children with a benign appendicular skeletal lesion between 2002 and 2007. The resistance of the affected bone to compressive, bending, and torsional loads was calculated with rigidity analysis performed with the use of serial transaxial quantitative computed tomography data obtained along the length of the bone containing the lesion and from homologous cross sections through the contralateral, normal bone. At each cross section, the ratio of the structural rigidity of the affected bone to that of the normal, contralateral bone was determined.
Thirty-four of 41 of included individuals completed activity questionnaire at least 2 years after the quantitative computed tomography-based rigidity analysis. None of the patients for whom no increased fracture risk had been predicted by the rigidity analysis sustained a fracture, even though they had not received surgical treatment.
In conclusion, quantitative CT may be the most accurate method of predicting fracture but even this method has false positives and false negatives and does involve risks associated with ionising radiation.
What Are the Indications to Treat Simple Bone Cyst?
Parent and child psycho-social attitude to treatments or activity restriction usually guide indication for surgery. Families may choose observation for an asymptomatic humeral SBC with satisfactory cortical thickness. For cysts that are gradually increasing in size, causing expansions and progressive thinning of the cortex with imminent threat of pathological fracture, families may want surgical treatment.
Some authors have suggested the use of a cyst index aimed at predicting the future risk of a pathologic fracture as shown above. Kaelin et al. recommended observation for humeral cysts with an index of less than 4 and for femoral cysts with an index of less than 3.5. As noted above the value of these is uncertain [62].
What Is the Best Evidence We Have to Support the Current Treatment Options for Simple Bone Cyst?
Treatments of SBC have evolved over time; we present treatments and the underlying evidence, from a historical perspective.
Curettage and Grafting
The lining of SBC is believed to play a role in its formation. Hence removing the lining is a logical action for treatment. Aggressive curettage of the lining was practiced and often this was combined with using phenol or zinc chloride to further destroy the cyst lining. Curettage was often followed by bone grafting. Graft materials were initially autograft. Allograft and other non-biologic materials were also used (no donor site morbidity, less operating time and potentially unlimited quantity).
Neer et al. [44] reported on 175 SBC treated between 1930 and 1960 with a minimum follow-up of 2 years. One hundred and twenty nine cysts were treated by curettage and bone grafting within 1 year of the diagnosis. Twenty-seven underwent chemical cauterisation using phenol or zinc chloride and 44 did not. The results were excellent in 15 (55 %), residual defect in 4 (15 %) and re-operation in 8 (30 %). Forty-four cysts were not cauterised with phenol or zinc chloride and the results were excellent in 21(48 %), residual defect in 17 (39 %) and re-operation in 6 (13 %). He concluded that chemical cauterisation was not of value.
In 93 cysts of the proximal humerus or femur, comparison between bone autograft and allograft was possible. In 35 treated with autograft the results were excellent in 21 (60 %), residual defect in 6 (17 %) and reoperations in 8 (23 %). In 58 cysts that treated with allograft the results were excellent in 28 (48 %), residual defect in 12 (21 %), and reoperation in 8 (36 %) favouring autograft over allograft.
Neer also demonstrated that the results of treatment differed depending upon the specific bone involved; cysts present in infrequent locations heal far better than those present in common locations such as humerus and femur. The incidence of re-operations was 30 % in the upper ends of the humerus, 17 % in the proximal femur, 11 % in the upper end of the tibia and none in the lower end of the tibia, whereas in the infrequent sites or unusual location, the incidence of recurrence was mostly 12 %.
Neer also found that true recurrence following surgical treatment is significantly more frequent in patients over 10 years old and age was a better prognostic criterion than the proximity of these cysts to the epiphyseal plate.
In another large study of 144 SBCs treated by curettage and grafting with freeze-dried, crushed, cortical-bone allograft, all had been followed from 12 to 48 months after surgery, Spence et al. [47] showed that 98 healed primarily and completely and 10 healed with a small, static, non- progressive residual defect, for an over-all rate of healing of 75 %. However there was a recurrence in 36 patients (25 %) which was quite apparent in most cases by 6 months. In none of the recurrent cysts did spontaneous healing occur after the recurrence had been established.
Spence also concluded that age, sex, size and site of the SBC, cyst activity and extent of cyst packing were important factors in cyst healing. In his series, in contrast to that of Neer, above, the rate of recurrence was higher in patients below the age of ten than in patients above that age. Of the 82 cysts in patients under 10 years old, 57 (70 %) healed and 25 (30 %) recurred, while of the 62 cysts in patients over ten, 51 (82 %) healed and 11 (18 %) failed to do so. The correlation between age and healing was consistent regardless of the activity (active or latent) of the cyst and the sex of the patient.
Eighty-one percent of the 103 cysts in male patients healed after the first allograft, while only 61 % of the 41 in female patients healed primarily. The recurrence rate in males was 19.4 % (20 of 103) in comparison to 39 % (16 of 41) in females. This recurrence rate was not related to the location, size, or type of cyst.
The size of the cyst was classified as small if its longest diameter was less than one-eighth of the length of the involved bone; medium, if the length was from one-eighth to one third of the bone length; and large, if its maximum dimension was longer than one-third of the bone length. The incidence of postoperative healing was 73 % for the small, 64 % for the medium and 82 % for the large cysts. Authors stated that low incidence of healing in the medium-sized cysts could not be explained by differences in distribution with respect to sex, age, cyst type, or cyst site. However, testing these findings revealed the difference was not statistically significant (χ2: P = 0.26).
All cysts in non tubular bones (6 in number) were fully healed. While 73 % of the 78 humeral cysts, 77 % of the 43 femoral cysts healed primarily and 67 % of the 12 tibial cysts healed.
Thirty-one (53 %) of the 59 active cysts and 75 (91 %) of the 85 latent cysts were healed after allografting. The degree of cyst packing was also correlated directly with the healing results since 88 % of 110 cysts which were completely packed healed primarily while only 32 % of the 34 incompletely packed ones healed, giving an over-all recurrence rate of 68 % in cysts not completely packed at the time of surgery.
Subtotal Resection with and Without Grafting
A more aggressive surgical approach was used to overcome the high recurrence rate of curettage and grafting. Subtotal resection with bone grafting was first presented in a scientific exhibit at the Annual Meeting of The American Academy of Orthopaedic Surgeons in 1962. It involved sub-periosteal excision of the cyst and the adjacent normal bone, followed by bone autograft harvested from the iliac crest or tibia. Freeze-dried allograft was also used in grafting large defects in younger children.
Fahey [40] published his findings in 20 patients who were treated with subtotal resection and bone grafting. There was only one recurrence (5 %). One patient developed growth arrest after surgery.
McKay and Nason [41] published their series of 21 patients who underwent subtotal resection but without bone grafting. They reported a 90 % (19/21) success rate. No infectious or neurovascular complications were reported, however six patients with humeral lesions and one with a femoral lesion, a fracture occurred at the time of operation as a result of the extensive decortications. The authors reported three patients with humeral growth disturbances before the surgery. To avoid the high rate of fractures, authors used internal fixation [42, 43].
In 1973, Scaglietti et al. [23, 24], an Italian surgeon introduced the approach of using steroids to treat SBC. He found that the chemical composition of fluid obtained from SBC was indistinguishable from that of a tissue transudate seen in joint arthritis [23]. On the basis of these observations, Scaglietti injected corticosteroids into these cysts. Depo-Medrol was chosen because it is a microcrystalline suspension of acetate of methylprednisolone that is relatively insoluble and, therefore, believed to have a prolonged pharmacological effect. Dr Scaglietti reported a 96 % healing success rate which started a new era of percutaneous treatment of simple bone cyst.
Percutaneous Techniques/Corticosteroid Injection
In 1979, Scaglietti published his series of 72 cysts treated with up to 6 injections of methylprednisolone acetate. Follow-up period was a minimum of 18 months; 60 % of patients healed completely, and 36 % healed “almost complete and only a 4 % failure to heal rate.” In 1982, he published a larger series (163 cysts) with a longer follow. Complete obliteration of the cyst was noted in 55 % of the cases and recurrence of the lesion was rare. However, in 45 % of the cases in which there was some improvement following injection, e.g., thickening of the cortex, some areas of new bone formation within the cyst interspersed in areas with little evidence of repair, there was a higher “recurrence” rate, i.e., the lesion subsequently enlarged or a lesion of a significant size persisted. He also stated that complete repair of the cystic cavity was observed mainly in patients younger than 11 years who have lesions localised in metaphyses near the epiphyseal line whereas older patients who were nearer to growth termination had arrest of the osteoblastic process and the persistence of some part of the cyst.
Capanna [22, 45, 65, 66] reported similar success rate with steroid injection and recurrence rate of 7 % only. Capanna et al. [67] promoted using contrast examination to identify non-contiguous septated areas to ensure the steroid was distributed through the whole cyst (Fig. 43.4).
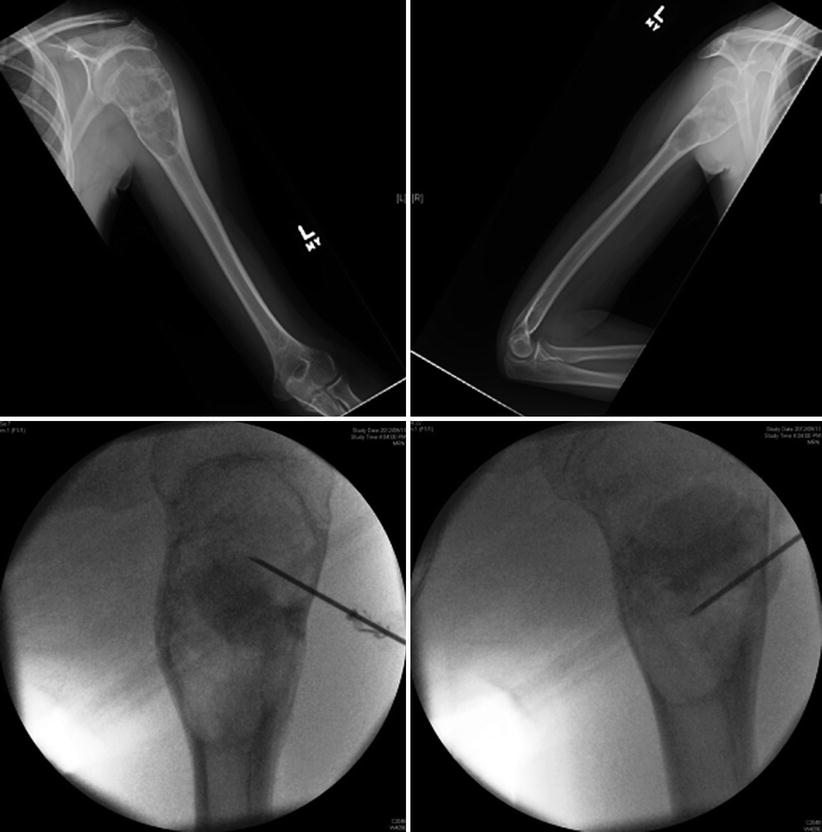
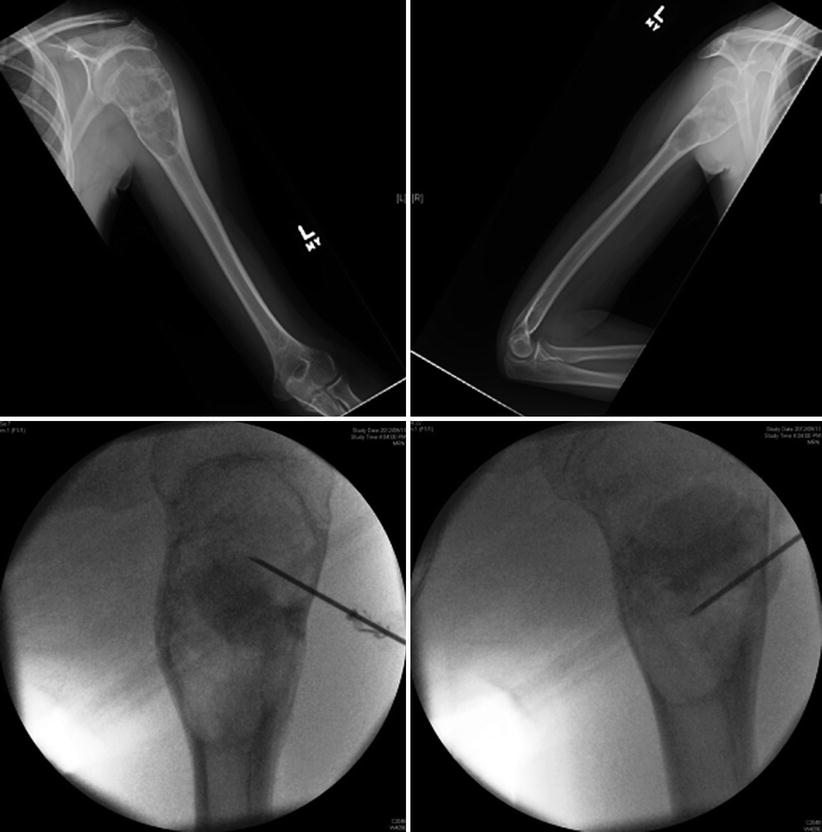
Fig. 43.4
Proximal humerus cyst underwent a cystogram before steroid injection. Bottom images show a non-contiguous septated areas
Various authors have reported comparable results and suggested refinements of the percutaneous steroid techniques such as using different types of steroids, different doses and combination with bone graft [68–72].
Two studies have compared steroid injection with curettage and grafting (Level III). Oppenheim and Galleno [73] compared 37 patients with SBC treated operatively to 20 patients treated with steroid injection with a minimum follow-up of 2 years. In the operative group the average operative time was 100 min, with a mean estimated blood loss of 300 ml. The recurrence rate was 40 %, rising to 88 % in patients under the age of 10 years with active cysts (less than 1 cm from the physis). Major complications occurred in 15 % and included infection, refracture, coxa vara, extremity shortening, and physeal damage. In contrast, the steroid-injected group had a recurrence rate of 5 %, although 50 % required more than one injection for maximum obliteration. The average operative time was 30 min, with negligible blood loss and a minimum hospital stay and rehabilitation. The only complications were a mild steroid flush in one patient and extremity shortening due to preexisting fracture in another. The end point of healing for this study was reconstitution of cortical thickness, rather than total obliteration at the cyst. No secondary fractures were encountered. They concluded that both operative treatment and percutaneous steroid injection exhibited a high rate of recurrence or persistence. The greater simplicity and lesser morbidity associated with the steroid technique favored it as their method of choice.
Bovill and Skinner [74] reviewed 32 patients with SBC treated in 3 different ways; 15 patients were treated surgically, 12 were given steroid injections, and five were treated nonoperatively. Thirteen of the 32 cysts were latent and 19 were active, judged by their proximity to the growth plate. The average follow-up was 5.6 years. They showed that steroid injections were as effective as surgical intervention while having lower morbidity.
Percutaneous Techniques/Bone Marrow Injection
The cellular contents of bone marrow particularly stem and undifferentiated cells have been the subject of extensive research in various medical fields. Bone marrow transplant has been successfully used in haematological malignancy, severe types of haemoglobinopathies and mucopolysaccharoidosis. It has also been used to promote fracture healing.
Lokiec [25] published a preliminary case series of 10 patients with SBC who were treated with bone marrow injection. Of note these patients also had curetting of the cyst, raising the possibility that mechanical disruption rather than the injection was responsible for cyst healing. All the patients became pain free after a mean of 2 weeks and resumed full activities within 6 weeks. All ten cysts consolidated radiologically and showed remodeling within 4 months. Review at 12–48 months showed satisfactory healing without complications.
Several authors reported positive results (but not 100 % healing) [75–77]. Yandow [75] reported 83 % (10/12) success rate. Delloye et al. [78] reported good results in approximately 88 % (7/8) of their patients.
Kose et al. [77] prospectively evaluated the outcome of the autologous bone marrow procedure in 12 patients. The mean volume of the lesions was 51.2 cc (27–74 cc). The mean follow-up time was 23 months (range: 18–38 months). Complete healing occurred in two of the patients. Three cysts had residual cystic defect in which two required curettage and bone chip grafts. Six cases recurred. One patient failed to show any signs healing. He found factors such as the size, multi-loculation, and completeness of the filling of the cyst with bone marrow grafting might influence the results.
Chang et al. [79] published a study comparing the results of aspiration and injection of bone marrow with those of aspiration and injection of steroid (level III). All were treated by the same protocol. The only difference was the substance injected into the cysts. The mean radiological follow-up to detect activity in the cyst was 44 months (12–108). Of the 79 patients included, 14 received a total of 27 injections of bone marrow and 65 a total of 99 injections of steroid. Repeated injections were required in 57 % of patients after bone marrow and in 49 % after steroid. No complications were noted in either group. In this series no advantage could be shown for the use of autogenous injection of bone marrow compared with injection of steroid in the management of SBC.
We identified a single randomised controlled trail [48] (level I) and a Cochrane systematic review and meta-analysis [80, 81] that compared bone marrow injection with steroid (methylprednisolone acetate) injection for treating simple bone cysts. The Cochrane systematic review and meta-analysis was published in 2014 and based on the above RCT only.
In their RCT [48] of 90 patients (72 were available after 2 years follow-up) Wright et al. randomly allocated to treatment with injection of either bone-marrow or methylprednisolone. The primary outcome was radiographic evidence of healing. The cyst was judged by independent radiologist to be either:
- 1.
Not healed (grade 1 = a clearly visible cyst or grade 2 = a cyst that was visible but multilocular and opaque).
- 2.
Healed (grade 3 = sclerosis around or within a partially visible cyst or complete healing (obliteration of the cyst)).
Patient function was assessed using the Activity Scale for Kids, and pain was assessed with the Oucher Scale. Sixteen (42 %) of the 38 cysts treated with methylprednisolone acetate healed, and 9 (23 %) of the 39 cysts treated with bone marrow healed (p = 0.01). There was no significant difference between the treatment groups (p > 0.09) with respect to function, pain, number of injections, additional fractures, or complications. Although the rate of healing of simple bone cysts was low following injection of either bone marrow or methylprednisolone, the latter provided superior healing rates. This trial suggested that even with steroid, the healing rate was low (42 %). Hence the search for better treatments modalities must continue.
Mechanical Disruption of the Cyst with or Without Fixation
Simple mechanical disruption of the cyst wall in a controlled fashion may produce a facture healing like state and potentially continuous drainage of the cyst and open cyst to marrow contents. Kirschner wires (K-wires), elastic nails and cannulated screws have been used to allow such continuous drainage [38, 82–85]. Elastic nails may also provide mechanical support for the bone while cyst is healing (Fig. 43.5).









