Fig. 3.1
Differential diagnosis—groin pain in the athlete
Hip
Groin pain often results from extra- and intra-articular problems in the hip. Extra-articular problems may be related to acute overload or trauma, or may arise more insidiously as a result of multiple factors such as guarding, repetitive overuse or overload, and maladaptations in response to articular pathology. The complex biomechanics of the pelvic girdle involve multi-directional loading and transmission of forces across the pelvic girdle itself in conjunction with the loading and transmission of forces from the spine and hip. Extra-articular soft tissues function to reduce loads across the pubic symphysis, the L5-S1 complex (disc and facet joints), the sacroiliac joint, and the hip joint itself. Injury to the underlying bone such as acute fracture or acquired deformity can overload the extra-articular soft tissue support, resulting in pain and dysfunction. Conversely, extra-articular soft tissue pathology can contribute to changes in the bone and cartilage. An extensive body of work has reviewed the complex biomechanics of the lumbar spine and pelvic girdle and how its dysfunction can lead to clinical problems [7–16].
Extra-Articular
Muscle and Tendon Disorders
Iliopsoas Tendon
Specific muscle and tendon disorders can be extra-articular causes of hip and groin pain. The iliopsoas muscle tendon complex can be a source of groin pain in athletes. Made up of the psoas major, psoas minor, and iliacus, the muscle fibers originate on the bodies of the twelfth thoracic vertebrae and the lumbar vertebrae, cross distally into the pelvis and join with fibers of the iliacus to form the iliopsoas tendon. The tendon passes over the anterior hip capsule on its way to insert into the lesser trochanter of the femur. As a prime generator of hip flexion, this tendon is an essential contributor to many athletic movements, often requiring both power and endurance. Furthermore, the tendon contributes to functional stability of the hip, pelvis, and spine.
Iliopsoas pathology can generate anterior hip pain directly. Alternatively, dysfunction may generate compensatory alterations in hip and pelvic girdle functioning which lead to secondary pain generation. Guarding from a primary hip or spine problem can increase firing of this muscle complex, often due to the inefficient biomechanics of altered muscle tendon unit length. In the acute setting, any of these situations can generate bursitis while the result of chronic dysfunction is typically tendinosis. Intra-articular hip problems are often present in association with iliopsoas muscle tendon dysfunction. Decreased hip internal rotation and extension resulting from intra-articular pathology often leads to a shortened, painful iliopsoas tendon. Acute injuries such as tendon tears or avulsions can also occur in athletes [17, 18]. While these typically occur from single traumatic event, repetitive overuse common in many athletes may increase the risk of these injuries.
Iliopsoas tendon disorders typically manifest as anterior groin or hip pain increased with active hip flexion. Forceful hip flexion or adduction is painful even with low intensity activities such as walking or getting out of a seated position [17]. Running, especially uphill or during speed training, typically generates anterior groin pain [17, 19]. Physical examination findings include tenderness over the distal tendon and lesser trochanter and pain with passive hip abduction and extension and active hip flexion [17].
Snapping Hip Syndrome
Groin pain can be associated with snapping hip syndrome, defined by the presence of an audible snap at or around the hip joint [20]. Snapping hip syndrome can result from external, internal, and intra-articular sources. The most common cause of a snapping hip is external, resulting when the iliotibial band or gluteus maximus tendon snaps over the greater trochanter. Internal snapping results when the iliopsoas tendon snaps over the iliopectineal bursa or less commonly the femoral head or lesser trochanter [17, 20–23]. This usually occurs as the hip extends out of a flexed position. The iliopsoas tendon may be thickened [19, 24] although it is usually normal in thickness. Athletes will have complaints and findings similar to iliopsoas tendon disorders plus a painful, audible snap over the anterior hip [17, 19]. Bringing the hip out of the flexion abduction external rotation (FABER) position into extension, adduction, and internal rotation often reproduces the snap [25]. Intra-articular snapping results from an abnormal structure in the hip joint itself, such as loose bodies, labral tears, chondral flaps, synovial osteochondromatosis, and even transient hip subluxation [19, 20].
Adductor Strains
Adductor strains are a common source of morbidity in athletes, especially ice hockey and soccer players [26, 27]. The adductors consist of the adductor longus, brevis, and magnus, as well as the gracilis, obturator externus, and pectineus. Primarily hip adductors in open chain activities, the adductors stabilize the pelvis and lower extremity during closed chain activities [28]. The most commonly strained adductor is the longus, due to its mechanical disadvantage of crossing two joints [29]. Adductors weakness, both in absolute strength and relative to the hip abductors, and decreased hip range of motion (ROM) predispose athletes to adductor strains [30].
The typical presentation is medial groin or thigh pain triggered by activity. Often insidious in onset, acute injury with avulsion or rupture can occur [31]. Swelling and less often a palpable defect may be present. Tenderness over the adductors, pain with active hip adduction and passive hip abduction and weak hip adduction are often present [25–32].
Sports Hernia
Anterior groin pain may be a result of a sports hernia, also referred to as athletic pubalgia [33] and which is described in detail in Chap. 1. This condition is more common in sports with repetitive twisting and rotation of the trunk and lower extremity such as soccer, ice hockey, and American football [33–36]. The precise pathophysiology is debated as it has been described as a hyperextension injury to the insertion of the rectus abdominus onto the pubic symphysis [34] and, alternatively, as an occult hernia of the posterior inguinal wall without a discrete tear [33, 36]. A related injury is Gilmore’s groin, defined as a tear in the external oblique aponeurosis and conjoint tendon [33]. An imbalance between strong hip flexors and weaker abdominal muscles is a risk factor for sports hernia [33]. The mechanism of injury is thought to be repetitive thigh hyperabduction and trunk hyperextension, generating shear at the pubic symphysis [33]. Night pain is very rare, with some concluding that the presence of night pain excludes a diagnosis of sports hernia [37, 38].
Athletes usually complain of groin pain which may be insidious in onset and is heightened with explosive movements such as kicking or sprinting. They may be tender over the conjoined tendon, superficial inguinal ring, posterior inguinal canal, or pubic tubercle. By definition, no palpable hernia is present. Resisted sit-ups and the Vasalva maneuver often elicit pain.
Osteitis Pubis
Thought to be the manifestation of degenerative or inflammatory changes at the pubic symphysis, osteitis pubis is a cause of groin pain in athletes (Fig. 3.2). The exact etiology is not known although it is associated with twisting and kicking in athletes, and chronic overuse injuries to the rectus abdominus and hip adductors [39, 40]. Athletes with decreased hip ROM are more likely to develop osteitis pubis [41]. Pain can be experienced in the groin, as well as the abdomen and medial or anterior thigh, often with activation of the lower abdominals or hip adductors. While symptoms often worsen with athletics, they may be present during simple ambulation.
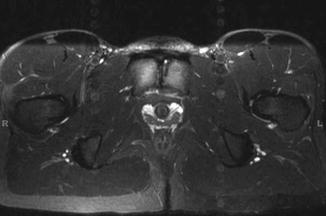
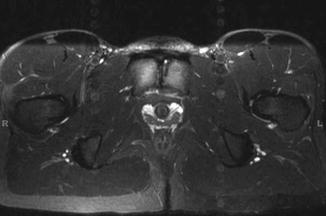
Fig. 3.2
MRI of soccer athlete with 6-month history of groin pain. Bony edema is present in the setting of degenerative changes across the pubic symphysis
Stress Fractures
Athletes are at risk for stress fractures in and around the hip which can present with groin pain. The pain is often over a diffuse area including the groin, anterior hip, and proximal thigh. Pain typically worsens with activity and progresses over time. Advanced cases may present with night pain and a noticeable limp even with walking. The single leg hop test is very sensitive for a stress fracture, although it should be used cautiously in athletes with severe symptoms. Tenderness is rarely elicited, even with severe stress fractures.
Stress fractures of the pubis or sacrum are rarely associated with significant complications, although they can be quite painful and require a lengthy recovery period. Femoral neck stress fractures are more concerning due to the risk of complete fracture, specifically for tension-type fractures on the superior neck. Compression fractures on the inferior neck are considered to be at much less risk of progression to complete fracture.
Clinicians should have a high index of suspicion for stress fractures as the cause of groin pain in the athlete. Insidious onset of a vague, poorly localized pain is particularly concerning. A positive hop test combined with no tenderness raises particular concern for a stress fracture, which must be ruled out with imaging.
Nerve Injuries
Groin pain can often arise from nerve pathology, and athletes are not immune to these disorders. Peripheral nerves at risk include the lateral femoral cutaneous, genitofemoral, ilioinguinal, iliohypogastric, femoral, and obturator. Lumbar radiculopathy (L1–L3) can also be a source of groin pain. Compression, either resulting from extended external pressure or internal fascial or muscle bands, is the most common mechanism, although direct injury from trauma or surgery can be a cause.
The lateral femoral cutaneous nerve passes under the ilioinguinal ligament anterior to the anterior superior iliac spine (ASIS) prior to piercing the tensor fascia lata. Repetitive cycling can irritate this nerve. Athletes will complain of burning pain over the groin and anterolateral thigh. Tinel’s sign may be positive and sensation may be decreased over the anterolateral thigh. Rest and activity modification are often adequate treatment [43].
Entrapments of the genitofemoral nerve and ilioinguinal nerve overlap in their clinical presentation. The genitofemoral nerve is usually injured as a result of surgery. The ilioinguinal nerve travels along the pelvic brim and transverses the abdominal wall medial to the ASIS prior to entering the ilioinguinal canal. Injuries to either nerve can result in pain and paresthesias on the medial thigh and lateral external genitals.
The iliohypogastric nerve pierces the abdominal musculature midway between the ASIS and the most proximal part of the iliac crest, where it may injured. Athletes will complain of referred pain in the nerve’s dermatome just superior to the pubis.
The femoral nerve enters the thigh under the inguinal ligament lateral to the femoral artery. The nerve can be compressed due to a psoas bursitis or an iliopsoas hematoma, typically due to a muscle tear. A forced hyperextension of the hip can also injure the femoral nerve. Athletes will have pain as well as significant thigh weakness [43].
Compression of the obturator nerve can occur at the obturator foramen or from the adductor brevis. Athletes will complain of pain and paresthesias in the groin, often radiating towards the distal medial thigh. Adductor weakness may be present. Symptoms typically worsen with exercise. Active adduction and passive abduction may be painful. Nerve stretch with hip external rotation and hip abduction can reproduce the pain and paresthesias [44].
Lumbar radiculopathy can result in groin, hip, and anterior thigh pain. Athletes may complain of hip flexor weakness. The femoral nerve stretch test will be positive but the straight leg raise will be negative [1].
EMG and nerve conduction studies are helpful and may be necessary to confirm the diagnosis of nerve entrapment. Nerve blocks can be diagnostic and sometime therapeutic. Surgical decompression is often necessary for nerve entrapment.
Sacroiliac Joint Dysfunction
Although patients with sacroiliac (SI) joint dysfunction typically present with gluteal pain near or surrounding the posterior superior iliac spine [45], up to 14 % of patients present with groin pain [46]. Athletes will often notice pain, sometimes associated with popping and/or clicking, with sport-specific activities involving unilateral loading or torsion through the pelvis and lower extremity. Sports that require single leg stance and torsion, such as skating and bowling, put athletes at greater risk. Rowing has also been associated with symptomatic SI joint dysfunction [47, 48].
Asymmetries of the pelvic girdle and sacroiliac joint are present on physical examination, especially at the levels of the anterior and posterior superior iliac spines. Leg lengths should be checked in both the supine position and with the patient seated upright with the hips flexed to 90º and the knees fully extended. With SI joint dysfunction, the measured length of the affected limb will change between these two positions. Other asymmetries that may be picked up on physical examination include hip rotation, with more internal rotation in one hip and more external hip rotation in the other hip, and hamstring flexibility, which will be lower on the side with anterior rotation. There are several provocative tests used to assess pain related to the SI joint, but none have been found to be specific when used in isolation. An example is the flexion abduction external rotation (FABER)/Patrick’s test. This test can be used to assess a hip or SI joint disorder (Fig. 3.3). Athletes with SI joint dysfunction may present with a constellation of symptoms and no single physical examination test has been proven to help guide the diagnosis. As a result, image-guided intra-articular injection of the SI joint is often used to help confirm the diagnosis [49].






Fig. 3.3
Flexion abduction external rotation (FABER)/Patrick’s test. A test used to provoke pain. If the pain is provoked in the groin, this may indicate a hip disorder. If pain is provoked in the posterior pelvis, it may indicate an SI joint problem
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







