Fig. 2.1
(a, b) Superficial medial collateral ligament and posterior oblique ligament, sMCL: superficial medial collateral ligament; MR: medial retinaculum; OPL: oblique posterior ligament; SM: semimembranosus tendon; VMO: vastus medialis obliquus muscle
Layer II is formed by the largest structure at the medial aspect of the knee, the superficial medial collateral ligament (sMCL) (Fig. 2.1b). It has been described to be between 10 and 12 cm long [23, 37]. It originates at the posterior-superior edge of the medial femoral epicondyle [20] and fans out to the tibial crest at 5–7 cm below the joint line, where two separate attachments can be found. The proximal tibial attachment is primarily to the anterior arm of the semimembranosus tendon. The larger distal bony attachment can be found anteriorly to the posteromedial crest of the tibia. Posterior to its tibial attachment, the sMCL blends within tibial expansions of the semimembranosus tendon. Anterior to the femoral attachment of the sMCL, it is continuous with the medial patellofemoral ligament (MPFL). The MPFL lies anterior to the medial capsule extra-articularly. It has been reported to have a length of approximately 55 mm and a varying width of 3–30 mm [1]. At the proximal edge of the MPFL, the vastus medialis obliquus muscle attaches. Often the MPFL can only be identified as a thickening of a fascial layer running from the proximal-medial edge of the patella to its femoral attachment between the posterior-superior site of the medial epicondyle and anterior-inferior site of the adductor tubercle [2, 20]. Soft tissue connections can be found to femoral attachments of the adductor magnus tendon and sMCL. Three muscles insert with their tendons to the posteromedial side of the knee joint. Most proximally, the adductor magnus tendon is attached in an osseous depression posterior-proximal to the adductor tubercle. At the distal-medial aspect of the adductor magnus tendon, a thick fascial expansion adheres to the medial gastrocnemius tendon, the capsular arm of the posterior oblique ligament, and the posteromedial capsule. More distally, the medial gastrocnemius tendon attaches in a depression proximal-posterior to the gastrocnemius tubercle. It has a thick fascial attachment to the adductor magnus tendon and a thin fascial attachment along its medial and posterior aspect to the capsular arm of the POL. Most distally, the semimembranosus tendon attachments are located on the medial and posteromedial parts of the tibia. The anterior arm of this distal insertion attaches deep to the proximal tibial attachment of the sMCL in an oval-shaped pattern distal to the tibial joint line. A direct arm connects to the posteromedial part of the tibia.
The medial joint capsule constitutes layer III. Posteriorly, its oblique fibers blend into layer II. It forms the deep MCL (dMCL) as a thickening below the sMCL, which spreads from the femoral condyle via the medial meniscus to the tibia. The dMCL shows a separate meniscotibial and meniscofemoral attachments, while blending with the sMCL posteriorly. The posteromedial capsule (PMC) is formed by dense tissue of layers II and III. Its femoral attachment site is at the adductor tubercle [12, 13, 24, 37]. Some authors identified a ligament-like structure within the PMC and termed it as the posterior oblique ligament (POL) [12, 13, 24]. The posterior border of the dMCL blends into the central arm of the POL, just posterior to the posterior edge of the sMCL. The POL is created by three fascial attachments to the semimembranosus tendon. It can be divided into a capsular, central, and superficial arm [12, 13]. The central and superficial arms blend into each other to form its femoral attachment posterior-inferior to the adductor tubercle and anterior-inferior to the gastrocnemius tubercle [20]. Distally, the thin superficial arm, which runs parallel to the posterior edge of the sMCL, merges with a distal expansion of the semimembranosus tendon. The strongest central part attaches distally to the posteromedial aspect of the medial meniscus, the posteromedial capsule, and the posteromedial aspect of the tibia [13, 20]. Anteriorly to the sMCL, layer III blends with layer I into the retinaculum.
The pes anserine tendons are situated between layers I and II–III and connect distally to the anteromedial aspect of the proximal part of the tibia. They consist of the sartorius, gracilis, and semitendinosus tendon in a proximal to distal fashion.
2.1.2 Biomechanics
The medial and posteromedial structures of the knee joint are loaded throughout the overall range of knee motion under valgus loads, internal and external rotation [6], as well as anterior and posterior drawer loads. There is a sharing response between the respective structures of the medial knee site, which act as primary and secondary restraint to various loads. The superficial medial collateral ligament (sMCL) has been identified as the primary restraint to valgus laxity of the knee [7, 17, 26] (Fig. 2.2). Griffith et al. [6] found that the sMCL does not function as one unit, but that its distal division was carrying larger loads than its proximal division, especially at flexion angles >20°, while the proximal sMCL was experiencing similar loads at all flexion angles. These differences in load transmission have been attributed to the different anatomy of the tibial attachments of the sMCL with the distal portion attaching directly to the tibia, therefore transmitting loads directly to the bone. In contrast, the proximal part only has soft tissue adherences, which might disperse loads among the soft tissue structures more evenly. Mechanical testing of the distal and proximal sMCL has confirmed this different loading capacity with the distal MCL providing significantly higher structural properties (sMCL failure loads ≈ 500 N, stiffness ≈ 63 N/mm) than the proximal sMCL (failure load ≈ 85 N, stiffness ≈ 17 N/mm) [39]. It has been stated that this functional separation of the sMCL could have implications for future procedures for reconstruction of the sMCL [6]. The overall sMCL functions as a primary restraint to valgus loading with the knee joint in external rotation, especially when knee flexion increases [6, 32]. It acts as a secondary stabilizer to the ACL and PCL in restraining anterior and posterior translation of the tibia [6, 10, 28]. The posterior oblique ligament (POL) works as an important reinforcement of the posteromedial joint capsule (Fig. 2.2). It functions as a primary constraint to valgus loads toward extension [7, 13, 25, 27]. It has a failure load of around 250 N and provides a stiffness at around 40 N/mm [39]. While the sMCL primarily stabilizes at external rotation, the POL primarily provides stability at internal tibial rotation [6]. In internal rotation a reciprocal load response can be seen between the sMCL and POL with increasing flexion, suggesting a complementary relationship of these two structures [6]. Also, the POL works as a secondary restraint to anterior and posterior tibial translation throughout the range of knee motion [6] in the cruciate ligament intact and especially in the cruciate ligament-deficient knee joint [10, 17, 25, 27, 28]. The deep medial collateral ligament (dMCL) has significantly lower structural properties than the sMCL (failure load ≈ 100 N, stiffness ≈ 28 N/mm) [39]. It has been discovered as a secondary restraint to valgus loads with its meniscofemoral portion acting at all flexion angles and its meniscotibial portion working predominantly at 60° of flexion [5, 27, 40]. At flexion between 30° and 90°, the dMCL provides restraints against external rotation torque flexion [5, 40].
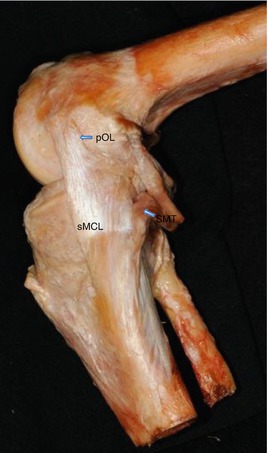
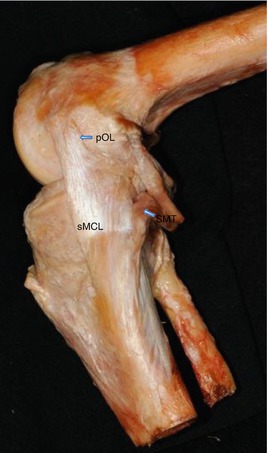
Fig. 2.2
Medial side knee anatomy. POL posterior oblique ligament, sMCL superior medial collateral ligament, SMT semimembranosus tendon
The semimembranosus tendon is known to produce direct stabilization of the posterior capsule through the oblique popliteal ligament and, indirectly, to add a synergistic action to the popliteus muscle through the fibrous expansion toward this muscle [14] (Fig. 2.2). As a dynamic stabilizer it provides additional stability to the posterior and posteromedial aspects of the knee, resisting internal torque and valgus stress with increasing knee flexion. Together with the popliteus muscle, it contributes to maintain posterior tibial stability. The attachments of the semimembranosus tendon to the posterior horn of the medial meniscus allow pulling of the meniscus backward in knee flexion, therefore protecting it from injury [13, 14].
The medial patellofemoral ligament (MPFL) is the primary restraint to lateral translation of the patella from extension until 30° of flexion, providing a mean tensile strength of 208 N [1]. While the medial retinaculum is tight at full extension, it slackens with flexion, contributing only around 11 % to overall lateral patella stabilization [4].The MPFL also guides the patella to engage centrally into the trochlea, underlining its importance for the alignment of the patellofemoral joint [3].
2.2 Lateral Periphery
2.2.1 Anatomy
Similar to the medial side, different tissue layers can be identified on the lateral side of the knee joint, which form the posterolateral complex (PLC).
Subcutaneously, the superficial layer of the iliotibial band can be found. It has a fascia-like structure and covers its deep fibers, which insert to the lateral supracondylar tubercle of the femur and blend into the lateral intramuscular septum [29, 33] (Fig. 2.3). Often, these layers are termed as “Kaplan fibers.” Fibers of the iliotibial band run medially to the lateral gastrocnemius and plantaris muscles, while blending on the lateral aspect of the knee with the short head of the biceps femoris. These expansions of the iliotibial band, also called capsule-osseous layer, function as an anterolateral ligament of the knee [15, 22, 33]. Distally, the iliotibial band inserts onto the lateral tibial tuberosity at Gerdy’s tubercle [33] (Fig. 2.3).
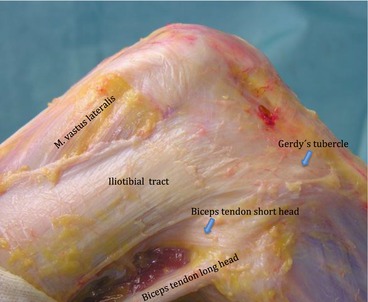
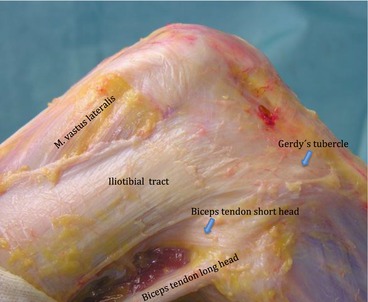
Fig. 2.3
Superficial structures of lateral compartment
Medially, below the iliotibial band, the biceps femoris muscle with its long and short head tendinous insertions can be identified. The long head of the biceps tendon displays two tendinous insertions to the bone. The direct arm inserts onto the lateral aspect of the fibular styloid, covering the fibular insertion of the lateral collateral ligament (LCL). The anterior arm runs lateral to the LCL and inserts onto the lateral tibial plateau. Aponeurotic expansions connect the long and short heads of the biceps femoris to the posterolateral region of the LCL [33, 34]. The short head of the biceps femoris consists of three tendinous arms. The capsular arm runs from the main tendon to the posterolateral joint capsule and inserts lateral to the tip of the fibular styloid. The fabellofibular ligament is formed by the distal edge of the capsular arm [33, 34]. The anterior arm inserts with the meniscotibial adhesions of the LCL at the proximolateral tibia. Often, ACL injuries are associated with an avulsion of this anterolateral aspect of the tibia, which has been termed a “Segond fracture” [31]. Identification of the biceps femoris tendon is imperative, since the peroneal nerve can be found posteriorly, 1.5–2 cm distal to the fibular styloid, advancing distally posterolateral to the fibular head.
The lateral collateral ligament (LCL) is an extra-articular structure of approximately 70 mm length. It inserts at the lateral aspect of the fibular head below the long head of the biceps tendon. Its femoral insertion can be found posterior to the lateral epicondyle (Fig. 2.4).
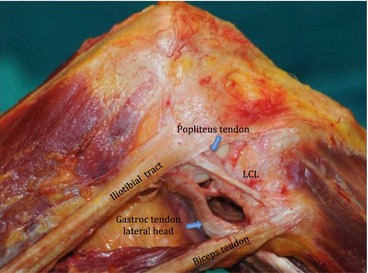
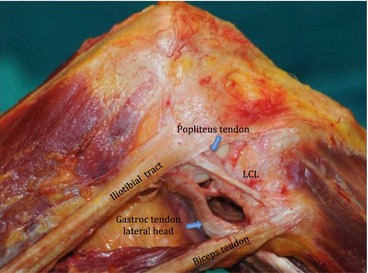
Fig. 2.4




Lateral collateral ligament
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








