Adult Scoliosis
Andrew P. White
James S. Harrop
Todd J. Albert
DEFINITION
Adult scoliosis is a coronal deformity of the spine, typically also involving axial and sagittal plane abnormalities.
Adult scoliosis can be categorized by patient presentation.11
One group, predominantly defined by lumbar stenosis and neurogenic claudication with degenerative deformity, has surgical management typically achieved by posterior lumbar procedures.
A second group, categorized by progressive deformity, with or without back pain, is more frequently treated with combination anterior and posterior procedures that may involve the thoracic spine to achieve surgical goals.
Although the surgical principles and techniques used to address these different categories are similar, important variations exist.
ANATOMY
Anatomic characterization of adult spinal deformity involves the coronal, sagittal, and axial plane.
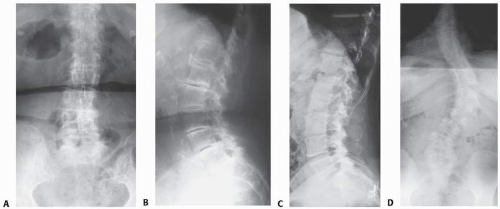
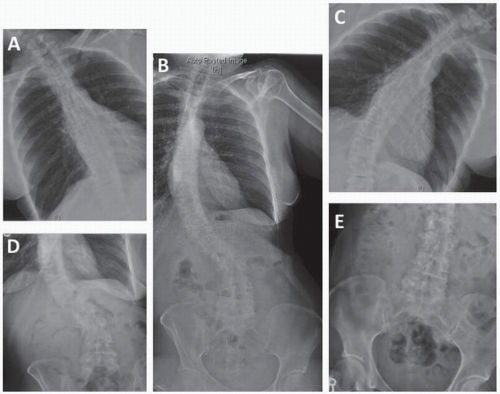
Lumbar degenerative scoliosis may be characterized by loss of lordosis and intervertebral disc height as well as listhesis in the anteroposterior, lateral, or rotary direction (FIG 1A,B).
Long curves, typically the result of a preexisting spinal deformity, may involve the entire thoracolumbar spine and may be associated with a significant rotational component (FIG 1C,D).
PATHOGENESIS
Adult scoliosis develops either as the progression of a spinal deformity that was present in adolescence or as the development of a deformity related to other spinal disorders.
The progression of the adolescent spinal deformity is related to increasingly unbalanced forces in the axial skeleton over time.
De novo adult deformity is commonly the result of degenerative disease and may also be related to osteoporotic fragility fractures of the vertebrae, resulting in a deformity frequently associated with spinal stenosis and mechanical back pain.
NATURAL HISTORY
The progression of an adolescent deformity is often seen as a long thoracolumbar curve in the adult.
Curves that reach a magnitude of more than 50 degrees are likely to progress, resulting in symptom exacerbation.
As patient age increases, curve flexibility typically decreases.
Lumbar degenerative curves typically involve fewer segments and may be limited to the lumbar spine.
Degeneration and deformity can cause central, lateral recess, and neural foramen stenosis as a result of the following:
Loss of intervertebral height
Hypertrophy of facet joints
Hypertrophy and buckling of the ligamentum flavum
Compression deformities
Neurogenic claudication, as well as radiculopathy and back pain, may result.
PATIENT HISTORY AND PHYSICAL FINDINGS
Determining the reason for the patient’s presentation is the first step in establishing the goals of surgical treatment.
Patients with extensive thoracolumbar deformity may present with concerns related to curve progression with an impact on the following:
Balance
Ambulation
Pain
Cosmesis
Patients with lumbar degenerative scoliosis classically present with complaints of neurogenic claudication or radiculopathy.
Hip and knee flexion contractures, related to the typical forward-flexed ambulation that limits the symptoms of neurogenic claudication, may be found (FIG 2).
Major focal neurologic abnormalities are unusual in this patient group, although relatively mild degrees of weakness in the tibialis anterior and extensor hallucis longus are not uncommon.
Physical examination should include the following:
Assessment of sagittal balance based on lateral observation of the patient standing with knees extended. A plumb line is dropped from the ear and the deviation (anterior or posterior shift) at the greater trochanter is measured, as is the regional (lumbar) lordosis and (thoracic) kyphosis. An upright posture with head over trunk and trunk over pelvis is a critical treatment goal.
Assessment of coronal balance based on posterior observation of the patient standing. A plumb line is dropped from the occiput and the deviation (leftward or rightward shift) at the sacrum is measured. A centered posture reduces gait abnormality.
Observation and palpation of the vertical relationship of the right and left acromions with the patient standing. Shoulder asymmetry may indicate coronal postural compensation to maintain upright stance.
Observation and palpation of the vertical relationship of the right and left iliac crests with the patient standing on the right, left, and both legs. Pelvic obliquity may be a primary or compensatory mechanism with spinal deformity.
Assessment of hip and knee range of motion. Long-standing sagittal plane deformities, as well as neurogenic claudication, may result in hip and knee flexion contractures.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs
Standing posteroanterior (PA) radiographs on 36-inch cassettes characterize the spinal deformity by
The magnitude of primary and compensatory curves, by the Cobb method (FIG 3)
Coronal balance: the relationship between the C7 plumb line and center of S1 on PA views (FIG 4)
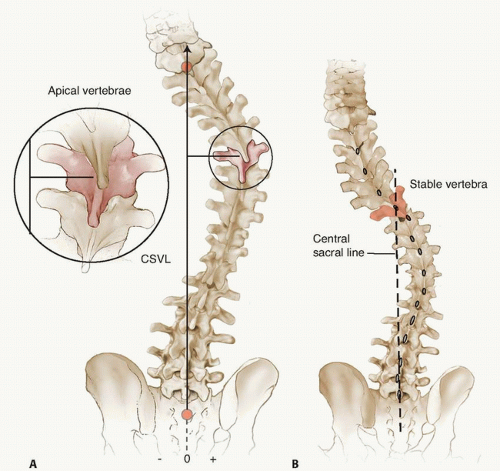
The apical vertebrae (most laterally deviated; FIG 5A)
The stable vertebra (caudal vertebra that is transected by the z-axis; FIG 5B)
Rotary and lateral listhesis
Standing lateral radiographs on 36-inch cassettes characterize the spinal deformity by
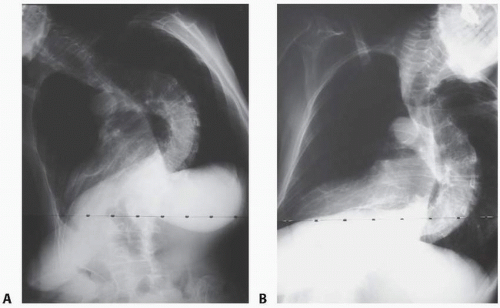
Regional lordosis and kyphosis (FIG 6)
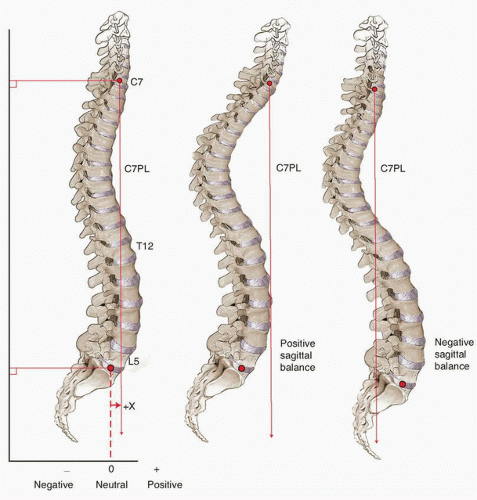
Sagittal balance: the relationship between the C7 plumb line and center of S1 on lateral views (FIG 7)
Anterolisthesis or retrolisthesis
Evaluate spinal flexibility
Determine the structural or nonstructural nature of the curve
Supine traction radiographs may also be used to evaluate curve flexibility.
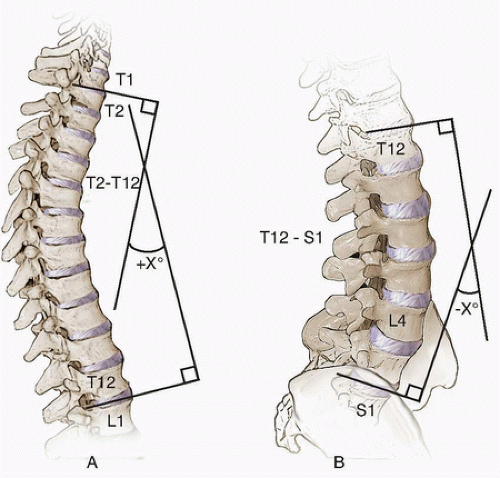 FIG 6 • Regional lordosis and kyphosis are measured on the standing lateral radiograph. Typically, the vertebral endplates are used as references for measurement. |
Computed Tomography Scans
Computed tomography (CT) images, reformatted in the plane of the superior endplates of each vertebra, can be used to measure pedicle dimensions, assess for potential auto fusions (that may impact curve flexibility and surgical correction), and assess local bone quality (osteoporosis, sclerosis, osteophyte density); all of which is used for preoperative planning.
Plain radiographs and CT images can be used to assess the degree of bone loss and tailor the reconstructive techniques to the bone quality of the patient.
Magnetic Resonance Imaging
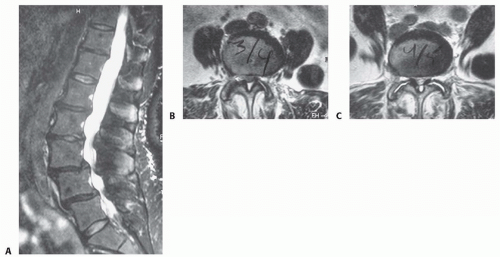
MRI is used to assess neurologic compression (FIG 10) as well as the status of the disc, ligamentum flavum, and other soft tissues.
Dual-Energy Radiographic Absorptiometry
Dual-energy radiographic absorptiometry (DEXA) is often performed for patients with identified risk factors:
Provocative Tests
Discography, although not 100% accurate, can be useful to assess for painful segments and evaluate the competence of the disc annulus, particularly in the lower lumbar spine.
Facet blocks have been employed to determine levels that should be included, or need not be included, in the fusion. This may be particularly relevant at the lumbosacral junction.
NONOPERATIVE MANAGEMENT
A physical therapy regimen may be tried, focusing on the following:
Stretching and core-strengthening exercises
Postural training
Gait training
Resolution of hip and knee flexion contractures
General conditioning
Nonsteroidal anti-inflammatory medications may be used if safely tolerated.
SURGICAL MANAGEMENT
The treatment of adult scoliosis is complex because of the global nature of the spinal deformity and the multiple causes of this disorder.
Efficiency, safety, and effectiveness in meeting surgical goals are each optimized by a well-designed procedure.
Preoperative Planning
Preoperative planning is instrumental to a successful treatment algorithm; avoiding both short- and long-term complications is paramount.
In 1968, the complications associated with surgical correction of adult deformity were quite significant17:
Five percent risk of death
Six percent risk of major neurologic deficit
Twenty percent risk of correction loss
Ten percent risk of deep infection
Forty percent risk of major medical complication
With advances in surgical and anesthesia techniques, neurophysiologic monitoring, and improvements in perioperative management, these risks have been decreased.1
The patient with adult scoliosis may carry a myriad of comorbidities that may increase the risk of a spinal operation or even contraindicate it. A complete preoperative assessment of those considering surgical treatment provides the opportunity to minimize risks by optimizing health status.
Modifiable conditions that affect surgical risk include the following:
Tobacco smoking
History of asthma or chronic obstructive pulmonary disease
Coronary or cerebrovascular disease
Diabetes
Nutritional deficiency
Osteoporosis
Depression
Current significant life stressors
Collaboration with consulting medical specialists who are trained in perioperative management is an important technique to optimize outcomes for patients with adult scoliosis.
Anesthesia colleagues familiar with this surgical course may also reduce risks.
Certain medical considerations directly affect the selection of surgical techniques for a patient with adult scoliosis.
Assessment of bone quality plays a critical role in the design of the operation.
Osteoporosis is the rule, not the exception.13 Although bisphosphonate medications may be helpful (and common) in treating osteoporosis, they inhibit osteoclastic bone resorption, which may have a negative impact on fusion biology.
Approach
Posterior surgical approaches are typically used for the treatment of adult deformity correction.
Anterior surgery may be used alone in isolated cases but is more frequently combined with posterior surgery to augment the deformity correction, reconstruction, or both.
Anterior exposure allows the soft tissue releases and interbody reconstruction that are often required for adequate coronal and sagittal deformity correction. Interbody reconstruction can help with decompression of the neurologic elements, particularly by restoring the height of the neural foramen.
TECHNIQUES
▪ Fixation Strategies for Osteoporotic Bone
Pedicle screw fixation is less effective in osteoporotic bone.5
Trabecular bone is predominantly affected by osteoporosis.
Because pedicle screws have cortical contact limited to the pedicle isthmus, a “windshield wiper” mode of failure may lead to screw loosening.
Fixation strategies for osteoporotic bone include the following4:
Taking advantage of the relatively stronger cortical bone
Augmenting the fixation of a pedicle screw within the existing trabecular bone
Extending the fixation, that is, to the pelvis, in order to “protect” the fixation in the sacrum, to prevent sacral fracture.
Bone implant interface complications in the osteoporotic spine can be reduced by various methods.
Sublaminar wires, laminar hooks, and pediculolaminar fixation take advantage of the cortical bone composition of the posterior spinal lamina.
Fixation of pedicle screws within osteoporotic trabecular bone may be improved by polymethylmethacrylate (PMMA) cement augmentation.21
Fluoroscopy is used to visualize the placement of 2 to 3 mL of PMMA per pedicle to ensure that cement does not migrate to the neural elements.
Calcium sulfate paste may also be used; this has the theoretical advantage of becoming replaced by bone over time.
Modified pedicle screws may also be used, including conical screws, hydroxyapatite-coated screws, and expandable screws.
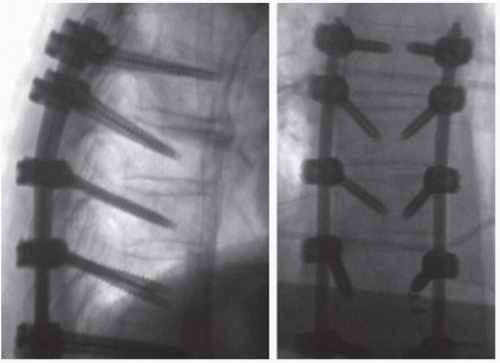 TECH FIG 1 • These radiographs depict both the straight ahead trajectory (uppermost and lowermost vertebrae on these images) and the anatomic trajectory (central three vertebrae on these images) for thoracic pedicle screws. Alternating trajectories at adjacent segments may help improve fixation.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|