Wrist, Hand, and Finger Injuries
Wade A. Lillegard
The significance of wrist, hand, and finger injuries is often underestimated by the athlete and clinician because of their non–weight-bearing status, a tendency to consider this injury as a sprain, and the pressure to continue playing. These injuries are therefore considered “minor” and not often included in the statistical records. McGrew et al. reported that 11% of 1,286 injuries in a primary care sports medicine setting were to the fingers and hands (1). In Dobyn’s series of 1,425 fractures, dislocations, and fracture–dislocations of the fingers and hands, the distribution was as follows: dislocations; 14 distal interphalangeal (DIP), 43 proximal interphalangeal (PIP), 19 metacarpophalangeal (MCP), 3 carpometacarpal (CMC), and 4 carpal (2). The remaining 1,342 fractures and fracture–dislocations were as follows: distal phalanx 133 (9%), DIP joint 160 (11%), middle phalanx (MP) 86 (5%), PIP joint 216 (14%), proximal phalanx 229 (15%), MP joint 88 (5%), metacarpalphalangeal (MC) joint 348 (24%), CMC joint 62 (4%), and carpal bones 217 (14%) (2).
The misdiagnosis of a sprain is potentially harmful as it may overlook an osseous, tendinous, or ligamentous injury, which could lead to chronic instability or pain.
Wrist Anatomy
Functional Anatomy
No tendons originate from or insert into the carpal bones (except for the sesamoidal pisiform), rendering wrist motion purely passive, with the carpal bones functioning as an intercalated segment (3).
The scaphoid (navicular) is the only carpal bone to cross the proximal and distal carpal rows (see Figure 27.1). This position provides stability by preventing the proximal row from collapsing in a zigzag configuration under compressive loads. The position and function also places the scaphoid at the greatest risk of injury (3).
Ligamentous Anatomy
The general configuration of the ligaments in the volar wrist is a double inverted V (4). The distal inverted V is formed by the two components of the deltoid ligament (capitoscaphoid and capitotriquetral ligaments); these are intracapsular and intrinsic. The proximal inverted V is formed by two intracapsular extrinsic ligaments: the radiolunate and ulnolunate. Between these two Vs is an area frequently devoid of ligamentous support of the capitolunate articulation. This potentially weak space is called the space of Porrier and may predispose the wrist to perilunate instability in hyperextension injuries (5).
Hand Anatomy
Tendons
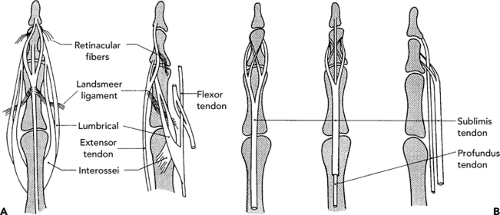
The nine finger flexors and the median nerve pass into the hand through the carpal tunnel beneath the transverse carpal ligament in the wrist (6). Five of the nine are deep flexors that pass through a split in the superficialis tendons and course to the distal phalanx of each finger and thumb (see Figure 27.2). The other four are superficial flexors that insert on the MP of each finger. The flexor tendons pass beneath a series of unique anchoring ligaments between the distal palmar crease and the DIP joint. These annular ligaments create “pulleys” and prevent the tendons from bowstringing. Tendon repair in this so-called “surgical no
man’s land” is therefore often complicated due to adhesions that form between the lacerated tendon-ends and these ligaments.
man’s land” is therefore often complicated due to adhesions that form between the lacerated tendon-ends and these ligaments.
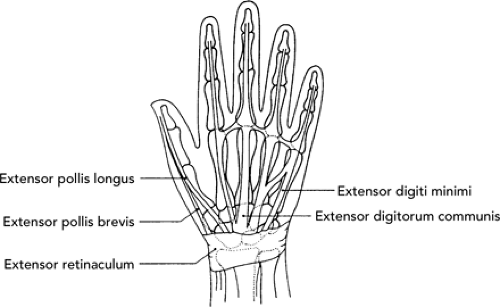
The extensor tendons enter the dorsal extensor hood at the distal end of the MCs. Distal to the sagittal fibers of the extensor hood enter the transverse and oblique fibers from the interosseous and lumbrical muscles. These blend into the sides of the extensor hood over the proximal phalanx and flex the MCP joint by pulling on the extensor hood (7). The central portion of this extensor complex (central extensor tendon) travels distally over the PIP joint and inserts into the proximal dorsal aspect of the MP to extend the PIP. The lateral bands continue radially and ulnarly forming the terminal extensor tendon and insert onto the proximal dorsal aspect of the distal phalanx to extend the DIP (7) (see Figure 27.3).
Ligaments
The volar plate is a U-shaped thickened portion of the joint capsule on the volar aspect of the finger joints and is a static stabilizer against hyperextension forces. Disruption of this will lead to chronic deformities if not allowed to heal in its proper anatomic position.
The collateral ligaments afford medial and lateral stability and are at maximal tautness at 70 degrees flexion for the MCP, 30 degrees for the PIP, and 15 degrees for the DIP (7). When the hand is immobilized for any length of time, the collateral ligaments will contract, therefore the ligaments should be immobilized flexed at the above angles (collaterals maximally lengthened) to prevent permanent contractures.
Physical Examination Principles—Wrist
Significant pain and/or swelling after trauma to the wrist imply a significant injury. Osseous and ligamentous injury that may lead to instability must be carefully investigated and ruled out before the injury is classified as a wrist sprain (8). The history is generally similar for most of these injuries—the athlete falls on or
strikes a dorsiflexed wrist (commonly referred to as a foosh injury or fall on an out-stretched hand), has rotational stress, or the mechanism of occurrence is not remembered. Pain and/or swelling are often noted immediately.
strikes a dorsiflexed wrist (commonly referred to as a foosh injury or fall on an out-stretched hand), has rotational stress, or the mechanism of occurrence is not remembered. Pain and/or swelling are often noted immediately.
On physical examination there may be a variable degree of swelling, with greater swelling indicating a more serious injury. Tenderness can be diffused or localized over the general area of injury, and range of motion (see Table 27.1) is limited by pain, swelling, or instability. The neurovascular status must be assessed on all injuries. Other specific tests and findings are mentioned under specific injuries.
Physical Examination Principles—Hand
Most injuries to the hand resulting in significant disability are caused by direct or indirect trauma, with subsequent disruption of a static (capsule, volar plate, collateral ligament, or bone) or dynamic (tendon, dorsal hood) stabilizer. Intricate interactions of the bones, ligaments, capsule, and tendons allow the exquisite functioning of the hand, and yet maintain its stability. Disruption of any of these may lead to significant functional disability (9). Central tendon rupture leads to “boutonniere” deformity, volar plate disruption leads to dorsal instability or a “swan-neck” deformity, angulated fractures lead to decreased grip function, and so on.
Clues to significant injuries can be any of the following: severe deformity on initial examination, incomplete reduction of the initial deformity, loss of normal alignment or joint motion (including catching, locking, or crepitus) during active or passive flexion and extension, an increase of more than 20% of the normal range of motion in any plane during passive testing, or pain or muscle contraction significant enough to inhibit testing (10).
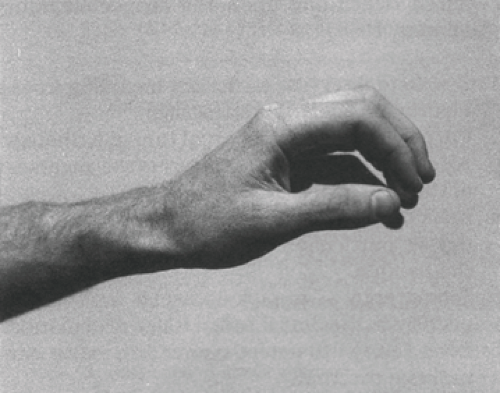
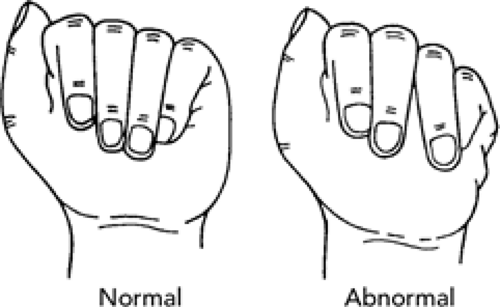
With the wrist in mild dorsiflexion, the curve of the finger is noted. This is referred to as the position of function (see Figure 27.4). In the absence of obvious fracture or dislocation, deviation from the normal semiflexed position suggests a flexor (or less likely, extensor) tendon injury (11). The arm is then pronated with the wrist slightly flexed. An excessive drop may suggest an extensor tendon injury. The patient is then observed while actively flexing and extending the fingers, thumb, and wrist, looking for any deviation from the normal. With gentle flexion, all of the fingers
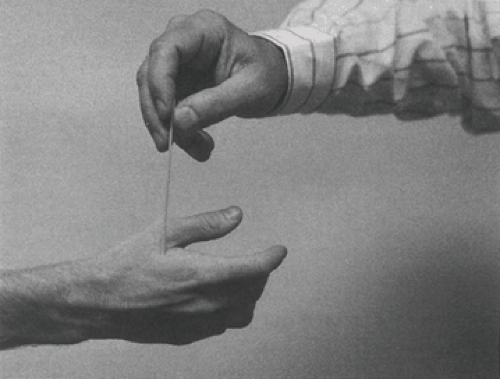
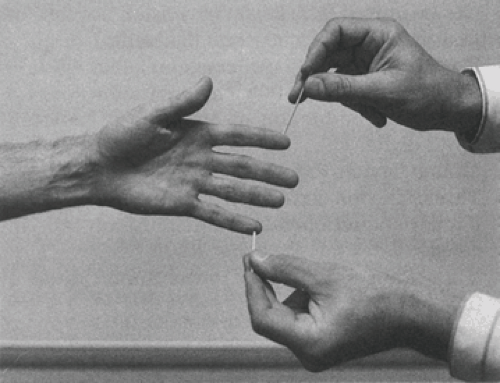
should generally point towards the scaphoid tuberosity (see Figure 27.5). Any deviation suggests a rotational deformity of a phalanx or MC (11). Active flexion and extension may be hampered by a disrupted tendon, ligament, or fracture, and an unstable joint may sublux. Sensation can be tested by asking the athlete to distinguish between the feel of the rough edge of a quarter and a smooth edged coin, or by two-point discrimination. Specific findings are discussed under individual injuries.
should generally point towards the scaphoid tuberosity (see Figure 27.5). Any deviation suggests a rotational deformity of a phalanx or MC (11). Active flexion and extension may be hampered by a disrupted tendon, ligament, or fracture, and an unstable joint may sublux. Sensation can be tested by asking the athlete to distinguish between the feel of the rough edge of a quarter and a smooth edged coin, or by two-point discrimination. Specific findings are discussed under individual injuries.
TABLE 27.1 Normal Rom of The Wrist and Hand | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Neurological Examination of the Hand and Wrist
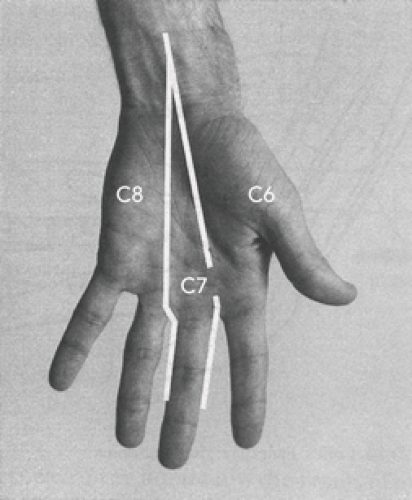
Because there are no distinguishable deep tendon reflexes in the wrists, hands, or fingers, the neurological examination concentrates on motor assessment and sensory testing (see Tables 27.2 and 27.3 and Figures 27.6, 27.7 27.8).
Imaging
Wrist
Initial radiographs for the acutely injured wrist should include at least a posteroanterior (PA) view of the wrist in neutral, and a true lateral view. Additional views, depending on the clinical indication, might involve PA in ulnar deviation and oblique and PA in 45 degrees pronation from neutral. Further imaging techniques may be necessary and are mentioned where indicated under specific injuries. Technetium 99 scintography (bone scan) is a useful study for evaluating suspected fractures not visualized on plain radiography. If there is focal increased uptake on the bone scan, computerized tomography (CT) or tomograms of the area should follow to define small fractures (12). Magnetic resonance imaging (MRI) of the wrist has a high rate of false-positive and false-negative results for many types of instabilities, but can be diagnostic in some cases. Wrist arthrography can be very useful, but decisions on this and other more detailed radiographic imaging techniques for suspected serious injuries are probably best left to the surgical consultant.
TABLE 27.2 Guide to Neurological Assessment Of The Hand | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Hand
Radiographs should be taken for any injury with bony tenderness, angulation, rotation, or instability. Generally, PA and lateral (with splayed fingers) views will suffice.
Treatment Principles
Injuries involving the hand and digits can be difficult problems to manage in athletes. Strict compliance with immobilization is often difficult to achieve with the athlete who perceives an urgent need to return to competition. A certain amount of risk is inherent in returning any athlete to play before complete healing. In the younger, skeletally immature athlete, the decision is easier because no risk should be taken and injuries should be allowed to heal fully. In a college or professional athlete the situation can be more complicated, requiring cooperation among the athlete, physician, trainer, therapist, and orthotist to agree on an acceptable solution. The ultimate decision to return to play is dictated by the individual’s condition, specific sport and position played, and the ability to safely splint/protect the injury.
Three treatment principles apply in the management of most hand injuries: splinting, ice, and elevation. The hand has minimal space to accommodate swelling, and the treating clinician needs to be aware of the devastating consequences of compression injuries from compartment syndromes. Additionally, swelling contributes to increased
pain, and may interfere with fracture reduction or skin closure if open reduction is necessary. In acute cases, splinting or uni- or bivalved casts are acceptable for use instead of circumferential casts to allow further swelling to occur (10). These may be converted or changed to a cast in a week when the swelling has decreased.
pain, and may interfere with fracture reduction or skin closure if open reduction is necessary. In acute cases, splinting or uni- or bivalved casts are acceptable for use instead of circumferential casts to allow further swelling to occur (10). These may be converted or changed to a cast in a week when the swelling has decreased.
TABLE 27.3 Motor Testing of Distal Upper Extremity | |||
|---|---|---|---|
|
Many fractures are nondisplaced and and show normal alignment. These fractures can usually be treated by closed methods as they are generally stable, and early, protected return to sports is usually achievable (13). Fractures that cannot be reduced, or are unstable after reduction, or those that involve displacement of the articular surface, should be referred to an orthopedic surgeon for management.
Common Injuries
Wrist
Distal Radius Fractures
Distal radius fractures represent approximately 17% of all fractures seen in the emergency rooms. There are numerous classification schemes for these fractures, but the “universal” and “modified Mayo” classifications will classify most fractures well (11).
“Universal classification”
Type I: nonarticular, undisplaced
Type II: nonarticular, displaced
Type III: intra-articular, undisplaced
Type IV: intra-articular displaced (see Figure 27.9)
Reducible (stable)
Reducible (unstable)
Irreducible (unstable)
Modified Mayo classification (used to identify distinct variants of intra-articular fractures)
Type I: intra-articular, undisplaced
Type II: intra-articular, displaced involving radioscaphoid joint (“Chauffeur’s” fracture) (Figure 27.9)
Associated with scapholunate tears
Significant dorsal angulation and radial shortening
Type III: intra-articular, displaced involving radiolunate joint
“Die-punch” or lunate load fracture
Irreducible by traction alone
Type IV: intra-articular, displaced involving both radioscaphoid and radiolunate joints
When evaluating distal radius fractures, one should assess for characteristics that render the fracture pattern potentially unstable. These include radial shortening more than 1 cm, angulation (apex volar) more than 20 degrees, and metaphyseal comminution.
Treatment
Most intra-articular fractures should be referred to an orthopedic surgeon for consideration of surgical fixation. An exception may be a nondisplaced intra-articular fracture in a low-demand or arthritic wrist, generally an elderly athlete. The choice on whether to reduce or refer an angulated fracture depends on the comfort level and experience of the treating physician. General guidelines for treating injuries/fractures of the distal radius are discussed in the subsequent text (2).
Nonarticular, Undisplaced or Minimally Displaced (Universal Type I)
Treat with sugar tong splint for 2 to 4 days until swelling subsides and then place in a short-arm cast for 3 to 6 weeks, with weekly follow up. Six weeks in a cast is appropriate for most fractures; however the elderly or those with underlying radiocarpal arthritis should be mobilized earlier to minimize postimmobilization stiffness. A long-arm cast for 3 to 4 weeks should be considered in there is significant pain with forearm supination/ pronation.
Nonarticular, Displaced/Angulated (Universal Type II)
After adequate reduction, these fractures should be treated with a long-arm cast for 3 to 4 weeks, followed up by a short-arm cast for 2 to 3 weeks. Weekly radiographs for 2 to 3 weeks should be taken to assure the fracture does not reangulate.
Intra-Articular, Undisplaced (Modified Mayo Type I)
Elderly patients or those with underlying radiocarpal arthritis can be treated with a long-arm cast for 3 to 4 weeks, followed up by a short-arm cast for 2 to 3 weeks. Younger patients should be referred to an orthopedic surgeon for consideration of anatomic reduction and surgical fixation (14).
Postcast Treatment
Cast immobilization invariably results in joint stiffness and hand/wrist weakness, which is directly proportional to the duration of casting. It generally takes as long as the joint was on cast to regain full range of motion. Weakness and discomfort generally takes as long as four times the duration of casting to resolve.
Home-based treatment with contrast baths for range of motion and theraputty for strength is quite effective (8). For contrast baths the patient draws two buckets of water, one at 100°F to 105°F and the other less than 50°F. Range of motion and stretching is performed in the warm water for 3 to 4 minutes, followed by soaking in the cold water for 1 minute. This cycle is performed four times, ending by bathing the joint in cold water.
Distal Radius Fractures in Children
Children have softer bones that frequently “buckle” rather than break (Torus or “buckle” fracture). A critical distinction must be made between this benign buckle fracture and the more concerning “greenstick fracture.” The buckle fracture involves buckling of one cortex, with the opposite cortex remaining intact. A greenstick fracture involves flexible immature bone breaking like a tree sapling. The tension side splinters whereas the compression side (opposite) undergoes plastic deformation, leaving a permanent bend unless it is reduced. Simple reduction is often not effective and this “incomplete” fracture must be completed to allow for correct realignment.
A torus or buckle fracture can be treated with a short-arm cast for 3 to 4 weeks, followed up by splinting for at-risk activities for another 3 to 4 weeks. Greenstick fractures angulated more than 10 degrees should generally be reduced (14). A minimally angulated greenstick fracture should be treated with a long-arm cast in full supination for 4 weeks followed up by a short-arm cast until healed. Parents should be counseled at the onset that these have a propensity to angulate even in a cast and these should be followed up by weekly radiographs through the cast for 3 weeks.
Dorsal Compaction Epiphysitis is a common sports-related issue facing skeletally immature athletes. Gymnastics and related sports that involve weight-bearing while balancing on the upper extremity with the wrist in extreme extension can result in chronic wrist pain and insult to the distal radial epiphysis. The well-being of the young athlete by protecting the status of the distal radial epiphysis is paramount. Hand/wrist straps are commonly used to achieve some protection by limiting wrist extension. Control of inflammation with cold therapy, even prophylactic icing, is the mainstay of treatment. Relative rest from this weight-bearing activity is usually necessary. Because long bone growth is at stake here, the condition needs to be monitored after diagnosis until closure.