, Antonio Cesarani2 and Guido Brugnoni3
(1)
“Don Carlo Gnocchi” Foundation, Milano, Italy
(2)
UOC Audiologia Dip. Scienze Cliniche e Comunità, Università degli Studi di Milano, Milano, Italy
(3)
Istituto Auxologico Italiano, Milano, Italy
Abstract
Whiplash is an acceleration–deceleration mechanism of energy transfer to the neck, and whiplash injury can be defined as a noncontact quick (50 ms) head–neck trauma with involvement of the spine as a whole. Whiplash injury sometime causes a labyrinth concussion with a consequent otoconia displacement. In these cases, a whiplash-associated benign paroxysmal positioning vertigo (WA-BPPV) may be induced. Whiplash-associated balance disorders (WABDD) not due to a recognizable BPPV derive from different combinations of different mechanisms. The key impairment is the biomechanic disruption of head-to-trunk and lumbar-to-gait coordination. Rehab treatment must be pointed to restore spine mobility as a whole with special regard to atlo-occipital joint and lumbosacral region and thus to (1) reorganize self-perception of posture, (2) reorganize proprioceptive information from the neck and the pelvis and (3) restore visual field stabilization during gait and movement.
The term “whiplash” has been used to describe a mechanism of injury and the various clinical manifestations as a consequence of the injury [1]. In 1995, the Quebec Task Force (QTF) on whiplash-associated disorders (WADs) adopted the following definition of whiplash: “whiplash is an acceleration-deceleration mechanism of energy transfer to the neck. It may result from rear-end or side-impact motor vehicle collisions, but can also occur during diving or other mishaps. The impact may result in bony or soft-tissue injuries (whiplash-injury), which in turn may lead to a variety of clinical manifestations called Whiplash-Associated Disorders” [2].
Whiplash injury can be defined, in a most wide interpretation, as a noncontact quick (50 ms) acceleration–deceleration head–neck trauma [3, 4] with involvement of the spine as a whole. This interpretation explains how the WADs comprehend symptoms variably combined:
Orthopaedic, such as neck pain and functional limitation of cervical and lumbar movements
Neurological, such as paraesthesias
Audiological, such as tinnitus and hypoacusia
Otorhinolaringological, such as dysphagia and disphonias
Equilibriometric, such as vertigo and dizziness
Odontoiatric, such as temporomandibular joint disorders
Whiplash injuries vary from minor to severe, and, generally, the evolution of the whiplash is divided into three phases:
The onset phase, involving local reactions with release of neuromediators, such as serotonin, histamine, bradykinin and classical inflammation
The recovery phase, locally characterized by synthesis of new collagenous fibres
The remodelling phase in which the body as a whole modifies its posture and movement strategies in order to restore normal daily life activities
Whiplash patients can be classified according to the severity of signs and symptoms. The QTF-WAD classification system consists of five levels:
0, no complaints or physical signs
I, neck complaints but no physical signs
II, neck complaints and musculoskeletal signs (such as a decreased range of motion or muscle tenderness)
III, neck complaints and neurological signs
IV, neck complaints and fracture/dislocation
The most common presenting symptoms following an acute motor vehicle collision are neck pain (88–100 %) and headache (54–66 %). Other symptoms are neck stiffness, shoulder pain, arm pain/numbness, paraesthesia, weakness, dysphagia, visual and auditory symptoms and dizziness. In most cases, WAD resolves quickly; 47 % of injured people return to normal activities within 4 weeks, and only 2 % continue to be absent from pre-accident activities 1 year after injury [5].
Whiplash injury sometimes causes a labyrinth concussion with a consequent otoconia displacement. In these cases, a benign paroxysmal positioning vertigo (BPPV) is provoked: whiplash-associated BPPV (WA-BPPV).
Most cases of WA-BPPV can be treated using physical therapy (see Chap. 8), by means of Epley’s [6] canalith-repositioning procedure (CRP) in the case of canalolithiasis and Semont’s [7] liberatory manoeuvre in the case of cupulolithiasis.
Although both manoeuvres have been shown to have therapeutic benefits, they require sequential procedures involving moving the patient’s head and body into unnatural positions, making them sometime unsuitable for WAD patients with cervical or back disorders, especially for older patients.
In WA-BPPV patients, it is thus better to use more conservative procedures like the supine to prolonged lateral position (SPLP) [8] or the rolling over manoeuvre (ROM) [9].
The pathogenesis of whiplash-associated balance disorders (WABD) not due to a recognizable BPPV is still debated:
Mechanical compression with dynamic stenosis of the vertebral arteria or arteriae
Sympathetic abnormal stimulation
Proprioceptive disorder especially from cervical and lumbar regions
Central vestibular system disorder
Probably, WABD derive from different combinations of different mechanisms. The kinematics of the acceleration–deceleration is different, for example, for the driver who is usually opposite to the trauma by means of her/his arms being on the wheel and the passenger who usually receives completely and passively the impact forces. Differences can be observed if the patient wore or not the safety belts during the impact: with safety belts, the movement of the head and the neck is not sagittal but torsional with a torsion having the mid-thoracic vertebrae (T7–8) as fulcrum. The direction of torsional component is different: counterclockwise for the passenger and clockwise for the driver. Furthermore, rarely the impact is caused by a straight rear-end collision, while, very often, the impact causes a rotational acceleration of the vehicle. Torsional and angular accelerations cause brain microlesions in different parts, and this can lead to different combinations of signs and symptoms [10, 11].
Following whiplash, either for mechanical lesions on cervical dynamic or for central dysfunctions, some modifications of patient posture are usually observed:
The head modifies its position according to an antalgic flexion.
The head reduces its rotational and lateroflexion movements.
During normal movements, rotation of the body is along the trunk and not the neck.
The trunk is ipsilaterally rotated with respect to the side of lesion.
The pelvis is rotated according to head antalgic position.
The position of centre of gravity (CoG) is modified.
Generally speaking, WABD may be considered as the result of desynchronization of the proprioceptive interaction between the so-called special proprioception (from the labyrinths) and general proprioceptions (from spine muscles, ligaments, joints, etc.) [12, 13].
Pathogenesis may be interpreted also under a phylogenetic point of view. The specific posture of the human being is the bipedal upright position with a maintenance of dynamic equilibrium as an inverse pendulum on a relatively restricted support surface area. This kind of posture represents a biomechanical evolution strictly correlated to the evolution of high-level cognitive processes specific for the human beings [14]. In adulthood, maintaining stance is perceived as an easy action to be performed, at least in normal conditions on steady surfaces, but it requires a very high level of sensorimotor control in order to allow a low-effort antigravity alignment of the different body segments [15].
The possibility to increase the perception of the environment is the main positive aspects of a bipedal upright posture: in the horizontal plane, the atlo-occipital joint allows the head to extend the exploration possibilities of the eyes [16]; furthermore, the relatively strict base of support allows rapid turns of the body in order to control also the environment at our back; in the vertical plane, the evolution of the lumbosacral spine allows the extension of the head and the trunk in order to explore, also for a long time, the environment over our head [17]. Thus, we can state that human posture is an evolution of the quadrupedal motion with very high possibilities of exploration of the environment all along the three-space axis.
The implementation of bipedal posture on quadrupedal motor control is relatively recent in the phylogenesis, and it can be retraced observing how the child fights against gravity force in her/his early months of life [15].
This concept may explain the pathogenesis of whiplash-associated disorders (WADs) that very frequently cause impairments not proportionate to the intensity of the impact. The relatively low energy transferred to the body during the accident acts specifically at the two most innovative parts of the humans: the atlo-occipital joint and the lumbosacral spine. In this way, whiplash immediately decreases the ability of the subjects to rotate the head and to extend the head and the trunk; in other words, whiplash brings backs the humans to a primate.
Thus, the key impairment is the biomechanic disruption of head-to-trunk and lumbar-to-gait coordination.
Treatment must be pointed to restore spine mobility as a whole with special regard to atlo-occipital joint and lumbosacral region and thus to:
Reorganize self-perception of posture
Reorganize proprioceptive information from the neck and the pelvis
Restore visual field stabilization during gait and movement
12.1 Exercises in the Gymnasium
12.1.1 First Week
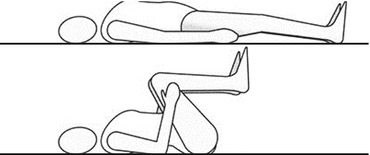
1.
2.
3.
The patient lifts her/his pelvis simultaneously extending the arms over her/his head. She/he then repositions the arms along the body lowering her/his pelvis (Fig. 12.3).
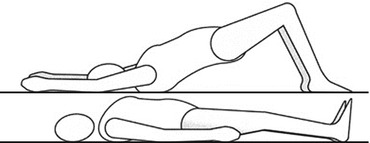
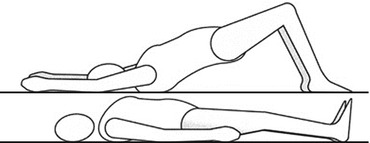
Fig. 12.3
Patient lifts the pelvis and extends the arms. He then returns to the resting position (Originally published in Cesarani and Alpini [21] published by Springer © 1999)
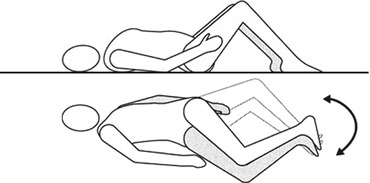
4.
In the quadrupedal position, the patient simultaneously extends the right arm and the left leg and then repeats the exercise with the left arm and the right leg (Fig. 12.4).
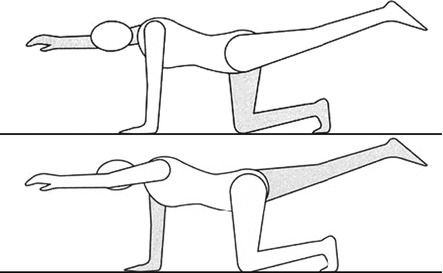
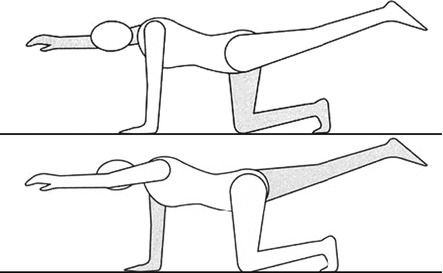
Fig. 12.4
Alternating extension of one arm and the opposite leg (Originally published in Cesarani and Alpini [21] published by Springer © 1999)
5.
In the prone position, the patient lifts her/his left arm and the right leg, holding the forehead over the bed. She/he then repeats with the right arm and the left leg (Fig. 12.5).
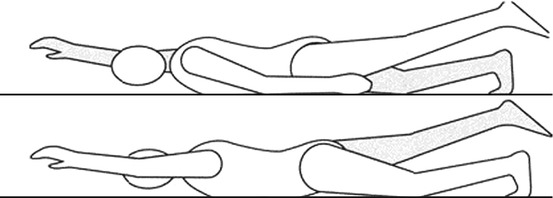
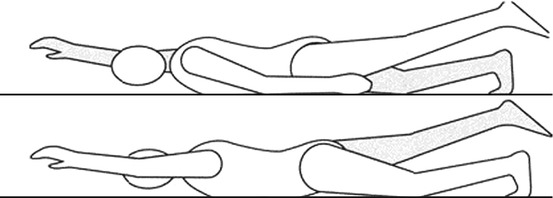
Fig. 12.5
In the prone position, simultaneous extension of one arm and the opposite leg (Originally published in Cesarani and Alpini [21] published by Springer © 1999)
6.
The patient repeats the exercise as above but simultaneously also lifting her/his head.
7.
The patient inhales. Exhaling, she/he bends forward holding her/his head on the right knee. She/he waits 10 s. Inhaling, she/he returns to sitting position. Exhaling, she/he bends forward taking her/his head on the left knee. She/he waits 10 s, and then inhaling, she/he returns to sitting position (Figs. 12.6 and 12.7).
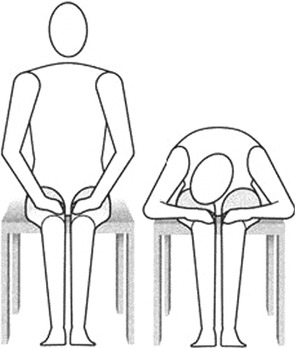
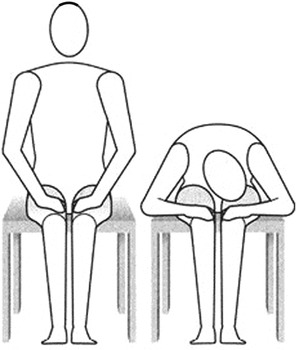
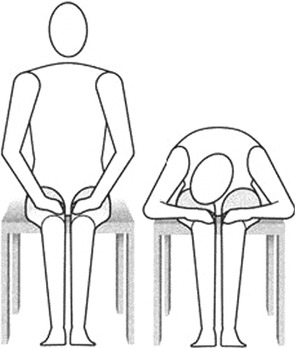
Fig. 12.6
Bending the trunk (Originally published in Cesarani and Alpini [21] published by Springer © 1999)
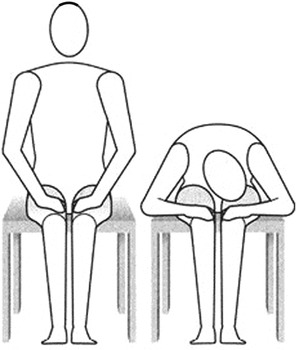
Fig. 12.7
Bending the trunk (Originally published in Cesarani and Alpini [21] published by Springer © 1999)
8.
Get Clinical Tree app for offline access

On a balance board:
(a)
The patient steps on the board with the feet centrally positioned and concentrates on a proper posture using a mirror to see her/his reflection. With eyes open, she/he transfers her/his weight from one foot to the other with a smooth flowing motion maintaining a correct postural alignment of the head and the trunk. In this case, feedback is visual, provided by the mirror.
(b)




The patient repeats the exercise but with eyes closed. The therapist controls the patient’s movements in order to avoid falls. The therapist is behind the patient helping her/him to maintain correct postural alignment of the trunk. In this case, feedback is somatosensorial, provided by the hands of the therapist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree