WHEELCHAIRS
Canes, walkers, crutches, manual wheelchairs, power wheelchairs, and scooters are examples of mobility assistive equipment (MAE). Power wheelchairs and scooters are referred to as power mobility devices (PMDs). The first section of this chapter reviews the basic components of manual wheelchairs, power wheelchairs, and scooters. Included in this discussion are criteria used when prescribing a mobility device and documentation requirements. Also discussed are the types of wheelchairs used by patients who have had a stroke, spinal cord injury (SCI), or amputation; those who are obese; as well as pediatric patients with cerebral palsy.
In order to prescribe the most appropriate MAE, a physician needs to know the key elements of the patient’s medical history, past medical history, social history, current functional status, and recent changes in the medical condition. Equally vital components of the decision-making process are the cognitive status of the patient and his or her ability to use the equipment. The amount of assistance needed for transfers, activities of daily living (ADLs), and mobility within the home are extremely important, as well as whether the patient has assistance from a home health aide or family member. The physician needs to fully examine the patient and assess the range of motion and strength in all joints. Joint contractures, spasticity, amputations, joint abnormalities, and weakness affect the patient’s ability to safely transfer, ambulate, and perform ADLs.
An important factor considered by the U.S. Centers for Medicare and Medicaid Services when approving a patient for a PMD is the inability to perform mobility-related activities of daily living (MRADLs), such as toileting, feeding, dressing, grooming, and bathing in the home using a cane, walker, or manual wheelchair. Documentation of functional mobility should include the following information:
Mobility limitations and how they interfere with the performance of ADLs.
Ability to use a cane or walker independently to accomplish all MRADLs in the home in a safe and timely fashion.
Ability to use a manual wheelchair to meet mobility needs in the home.
Changes in the patient’s condition or functional limitations that now necessitate a PMD.
Physical and mental abilities that may prevent safe transfer into, and operation of, a PMD.
Whether the patient is willing and motivated to use a PMD in the home.
Whether the patient’s typical environment supports the use of a wheelchair or PMD.
Before prescribing an MAE or a PMD, a physician must perform a face-to-face examination with the patient, and the date of the examination must be documented. The face-to-face examination should include the patient’s past and present medical history, social history, functional mobility and ADL status, review of systems, and a physical examination. It should also include the weight and height of the patient and whether the patient has the ability to safely propel a manual wheelchair or safely drive a PMD. The physical examination should include documentation of cardiopulmonary, neurologic, and musculoskeletal abnormalities. Range of motion in all limbs and the presence of contractures, swollen joints, or amputations should be described.
The impact of the medical history on the patient’s functional status should be highlighted. The social history should document whether the patient has a wheelchair-accessible home, especially if the patient is applying for a PMD. The number of steps required to enter the home and whether the patient has a wheelchair ramp are extremely important pieces of information.
The patient’s strength and endurance should be assessed and his or her ability to perform ADLs should be documented. Head and trunk control and the ability to sit upright without support should be assessed. A gait analysis should be performed, and the ability to safely stand and transfer should be evaluated and documented. The patient’s cognitive status and ability to safely maneuver a manual wheelchair or PMD should be noted. Patients with severe cardiac or pulmonary disease who experience dyspnea on exertion or at rest may have normal muscle strength; however, they may be unable to propel a manual wheelchair secondary to shortness of breath. These patients may also be unable to safely perform MRADLs in a reasonable amount of time and may benefit from a PMD; this should be so noted in the assessment. Multiple studies have noted that propelling a manual wheelchair increases the energy expenditure in users. Some multiple sclerosis patients with increased tone and decreased coordination may be unable to safely ambulate, push a manual wheelchair, or perform MRADLs and may require a PMD to help maintain their independence. Ataxia, coordination issues, and proprioception problems should be assessed and the effect on mobility and ADLs documented. Documentation of past or present sacral decubitus ulcers and skin integrity should be noted as this information will help to determine the appropriate wheelchair cushion.
In the United States, wheelchair home accessibility requirements vary with each insurance company. Some insurance companies do not require a wheelchair ramp. Others require a wheelchair ramp if there are steps to enter the home or apartment and will automatically deny authorization for a PMD if the patient does not have a wheelchair-accessible home. Still others require a photograph of the ramp at the patient’s place of residence and a home functional evaluation performed by a physical therapist to document the functional need for a PMD. Medicare requires adequate access between rooms, adequate maneuvering space, and surfaces appropriate to operation of a PMD. At present installation of a wheelchair ramp is not covered by most major insurance companies and is a direct cost to the patient. Patients with limited income may apply for a wheelchair ramp though federal, state, and local government resources, such as local agencies on aging (eg, Philadelphia Corporation for Aging), Maximus, or Liberty Resources.
A letter of medical necessity must be written or a functional mobility examination form completed based on the face-to-face examination. The specific documentation requirements vary with each insurance company. Some insurance companies specify a time frame for the completion of required documentation after the face-to-face examination. Medicare requires a seven-element prescription, including the beneficiary’s name, description of item that is ordered, date of completion of the face-to-face examination, pertinent diagnoses or conditions that relate to the need for the PMD, length of need, physician’s signature, and date of physician’s signature.
Medicare requires all documentation to be completed and submitted within 45 days after the face-to-face examination. Some managed care insurance companies, upon review of the initial letter of medical necessity, may request additional documentation, which must be submitted within a certain time frame (usually 15 days). In most cases if the time limit for completion of documentation has expired the patient must be reexamined and the process begun anew.
[PubMed: ICN 006308].
[PubMed: ICN 905063].
Six key measurements are needed to properly fit a patient for a manual or power wheelchair: seat width, seat depth, leg length, seat height, arm height, and back height. All measurements should be obtained with the patient in the seated position. Weight and height should also be recorded.
To determine seat width, the widest area across the thighs or hips is measured, in inches, and 2 inches (5 cm) is then added to the number obtained. The adjusted measurement provides a 1-inch (2.5-cm) space on each side of the seat, between the hips and the armrest skirt guard, that should be sufficient to allow room for a prosthesis, brace, or coat. The examiner should be able to run both hands at the same time vertically along the side of the wheelchair seat and touch the hips and the armrest skirt guard simultaneously. The standard wheelchair seat width is 18 inches (46 cm).
A patient will have difficulty propelling a wheelchair if the seat is too wide. A wide wheelchair may prevent the patient from being able to reach the hand rims on a manual wheelchair, causing him or her to lean toward one side of the wheelchair while propelling and resulting in unequal weight distribution. Patients with poor trunk control need lateral support to maintain a proper upright posture. Insufficient lateral support from a wide wheelchair and truncal instability may lead to the development of scoliosis or contractures due to muscle imbalance. A small, narrow wheelchair seat will be uncomfortable and too tight. A narrow wheelchair seat may cause pressure along the hips and thighs from the armrest guard, which may lead, initially, to skin irritation and, with continued pressure, to a pressure ulcer. Transfers may also be difficult because it will be harder for the patient to stand up if the wheelchair seat is too tight. A small wheelchair may prohibit the use of a prosthesis, brace, or coat.
The seat depth is measured from the posterior buttock to the popliteal fossa, and 1–2 inches (2.5–5 cm) is then subtracted from the number obtained. The examiner should be able to insert 2–3 fingerbreadths horizontally between the edge of the seat and the popliteal fossa. The wheelchair seat should not cause pressure in the popliteal fossa. A standard wheelchair seat depth is 16, 18, or 20 inches (41, 46, or 51 cm) in adults. Longer seat depths require custom orders. If the seat is too long, the edge of the seat will press into the popliteal fossa, causing irritation of the skin and impeding circulation. A long seat may also prevent the patient from sliding back fully into the seat. This will prevent the patient from sitting properly against the wheelchair and will result in a slumped posture. A short wheelchair seat will not provide enough support to the thigh, which will cause more pressure at the ischial tuberosity, increasing the risk of decubitus ulcer. The unusual weight distribution caused by a short wheelchair seat also makes the patient prone to falling out of the wheelchair, especially on uneven surfaces.
The leg length is measured from the knee bend at 90 degrees to the bottom of the heel. A long leg length will result in the footrest not providing support to the leg; additionally, the footrest may bump curbs and other obstacles. The bottom of the footrest is usually 2 inches (5 cm) from the floor. A short leg length will cause extreme flexion of the hip and raise the knee, causing increased pressure on the ischial tuberosity. This positioning will make the patient prone to decubitus ulcers and will lead to hip and knee flexion contractures. The thigh should be parallel to the seat cushion. A raised knee will also impede the patient’s ability to pull the wheelchair underneath a table.
The seat height is the height of the seat platform with respect to the floor. Wheelchair seats are not always level and some patients prefer to have their seat slanted toward the back to provide stability. The seat height is measured from the knee bend at 90 degrees to the bottom of the heel; 2 inches (5 cm) is then added to allow for clearance of the footrest. Next, the thickness of the wheelchair cushion when compressed is subtracted from the previously calculated number. Factors to consider include the height of the wheelchair cushion and the compressibility of the cushion. Foam wheelchair cushions vary in stiffness and density; some foam cushions will compress to half their normal height, whereas others (eg, antidecubitus cushions with a contoured nondeforming foam base) are not compressible.
A seat height that is too low will cause the patient’s feet to drag and raise the thigh and knee, causing increased pressure on the ischial tuberosity. This type of positioning makes the patient prone to decubitus ulcers and contractures at the hip and knee. Additionally, when the seat is too low patients with poor trunk control may exhibit a slumped posture, which could lead to scoliosis. A low seat height will also impair transfers to different surfaces and make reaching for objects more difficult.
Conversely, a seat height that is too high will prevent the feet from touching the floor; consequently, some patients will not be able to use their feet to help propel the wheelchair. Patients may also have difficulty reaching the hand rims for propulsion, and transfers may be impaired. A too-high seat may impair the ability to perform ADLs, reach for objects, and pull the wheelchair underneath a table.
The arm height is measured from the seat to the bottom of the elbow flexed at 90 degrees, and 1 inch (2.5 cm) is then added to the number obtained. The appropriate arm height will provide proper positioning of the upper extremities and give support to the arms and shoulders. If the patient is sitting on a cushion, the arm height should be measured from the top of the cushion. A high arm height will cause the shoulders to be pushed upward, resulting in pressure and pain in the glenohumeral joint. The patient will not be able to comfortably rest the upper extremities on the armrest and the upper extremities will not have support and stability. If the arm height is too low, no support will be provided for the upper extremities. Unsupported upper extremities tend to pull the body forward, causing a slouched posture. The patient may also lean forward, which will result in poor posture, leading to kyphosis or scoliosis and compromised respirations in patients with poor trunk control. Without armrest support for the upper extremities, shoulder subluxation may worsen in stroke patients.
The back height determination is dependent on the patient’s level of functional mobility and the type of wheelchair prescribed. The patient’s balance, coordination, arm strength, the amount of trunk support needed, and the upper extremity wheelchair propulsion ability are important factors to be considered in the back height determination. The backrest should provide support and help to maintain proper posture. For patients with good trunk control and posture, a wide variety of wheelchair back heights is available, ranging from just below the pelvis, as in sports wheelchairs, to the midback height used on a standard wheelchair.
For a manual self-propelled wheelchair, the back height is measured from the seat to the axillary floor with the shoulder flexed at 90 degrees; 4 inches (10 cm) is then subtracted from the number obtained. The top edge of the back upholstery should be slightly below the inferior angle of the scapula. At this height the scapula and shoulder will be free for easier propulsion of the wheelchair. For patients with poor trunk control who require more back support and do not self-propel or those who plan to use a power wheelchair, the back height is measured from the seat to the shoulder. If the wheelchair is a recliner or has a tilt mechanism, a headrest is needed for head support and control. Wheelchair users with kyphosis or scoliosis will need a higher back height to provide lateral support and truncal stability to help prevent progression of the disease.
When measuring the wheelchair back height, it is important to consider the wheelchair cushion thickness because the cushion will affect the seat height and ultimately the back height. A low back height will not provide enough support for the upper trunk. In patients with poor trunk control and muscle weakness, this will lead to poor posture and the development of scoliosis or kyphosis. The patient can easily lean backward over the top of the upholstery, and this weight shift may cause the chair to tip over backward. A high back height will interfere with propelling the wheelchair, because the high back will limit the movement of the upper arm and shoulder and impair scapular mobility. The scapula may also rub against the back of the wheelchair causing irritation.
There are several manufacturers of manual wheelchairs (ie, Pride, Invacare, Drive, Everest and Jennings, and Quickie), with inventory ranging from high-end models to low-end basic wheelchairs. Differences between models reflect the materials used in fabrication, style, design, and the various features available. However, the basic components of manual wheelchairs are similar across all brands. These components include the frame, seat, back, tires, wheels, hand rims, casters, fork and stem, axle plate, axles, headrest, armrest, leg rest, footrest, seat cushions, back cushions, and accessories (Figure 41–1). As previously noted, the standard wheelchair seat width is 18 inches (46 cm), and the standard seat depth is 16, 18, or 20 inches (41, 46, or 51 cm). A seat depth greater than 20 inches (51 cm) is a custom order.
Sling seat—This is the standard option on most wheelchairs and is made of nylon or vinyl. Prolonged sitting in a wheelchair will cause the sling seat to sag.
Solid seat insert—The insert is made of wood and is used to prevent sagging of the sling seat. It provides a good base of support for a wheelchair cushion. The solid seat insert may attach to the wheelchair with clips or be a separate item placed underneath a cushion.
Folding solid seat—This option allows the seat to fold to the side when the wheelchair is folded, permitting easier transport.
Stroke patients with limited mobility would benefit from a solid seat insert and seat cushion to prevent poor posture while sitting in the wheelchair for long periods of time.
The components of the wheel include the type of tire, push rim, tire rim, magnesium wheel or wire spoke wheel, and the hub. A standard self-propelled adult manual wheelchair has two large wheels in the rear and two smaller wheels called casters in the front. Rear wheels are usually 24 inches (61 cm) in diameter and casters are 5 or 8 inches (13 or 20 cm) in diameter, depending on the model. Several types of tires are available for wheelchairs, depending on the activity performed.
Numerous types of tires are available in different widths and tread thicknesses to accommodate functional mobility needs. Thin, smooth tires have less resistance, are easier to propel, and are well suited for sports activities. These tires are designed for speed, maneuverability, and endurance. Thin tires with a small amount of tread are suitable for indoor use. Wide tires with thick tread are more suitable for outdoor use and provide better traction on uneven rough terrain.
Casters are the small wheels in the front of the wheelchair used for steering and maneuvering and are made of aluminum or cast plastic. Caster sizes vary from 2 inches (5 cm) to 8 inches (20 cm) in diameter. Caster tire choices include solid rubber (polyurethane), spoke, pneumatic, and semi-pneumatic. Pneumatic casters provide a more comfortable ride; however, maintenance is required. A standard manual hemi-wheelchair usually has 8-inch (20-cm) solid rubber casters because this size is more suitable for different environments and terrains. A solid rubber caster is maintenance free. Small casters are used on basketball and tennis wheelchairs and are more likely to get caught in elevator doorways and sidewalk cracks.
The fork and stem assembly attaches the casters (small front wheels) to the wheelchair. The lengths of the fork and stem determine the seat-to-floor height. Some wheelchairs have adjustable forks with different positions for wheel attachment; other, standard manual wheelchairs have fixed nonadjustable forks. The stem is available in different lengths and is specific to each type of caster. The fork and stem assemblies adjust the seat tilt and determine the height from seat to floor.
Rear wheels are attached to the wheelchair via the axle plate. Different types of axle plates are available; some are adjustable, allowing the rear wheel to move forward or backward, or the wheel to be raised or lowered, which will affect the height of the wheelchair seat.
A standard axle plate has limited adjustability, depending on the model of the wheelchair. The rear wheels may have a few inches of adjustability either forward or backward, and the seat height may have two variable positions. In a stroke patient, the wheel is placed in a higher axle position to decrease the seat-to-floor height.
The front rigging of the wheelchair consists of the leg rest and footrest. The leg rests are used to provide support to the lower extremities, and the footrest provides support to the feet.
Anti-tippers are devices that attach to manual wheelchair frames to keep patients from tipping the wheelchair over backward or forward (Figure 41–2). Anti-tippers may be fixed or removable, and can be attached to the rear of the wheelchair or to the front rigging.
Wheelchairs are prone to tip backward when patients attempt to stand up from the wheelchair or to propel it up an incline, ramp, or hill. The combination of propelling a manual wheelchair up a hill while simultaneously pushing on the hand rims transfers the center of gravity behind the rear wheels, which can cause the wheelchair to tip backward. Anti-tippers can also be attached to the front of the wheelchair to prevent the wheelchair from tipping forward. Forward tipping is less common but may occur when a patient tries to pick an item up off of the floor by bending forward. Forward tipping can also occur with any activity that causes the center of gravity and weight to shift forward over the casters.
A variety of anti-tipper styles are available to accommodate different wheelchairs. Anti-tippers are optional equipment on most manual wheelchairs except tilt-in-space and recliner wheelchairs. The disadvantage of anti-tippers is that they may interfere with climbing over curbs or other small obstacles. Rear anti-tippers may need to be manually turned upward when tilting the wheelchair backward to traverse curbs. When propelling the wheelchair on uneven terrain, the anti-tippers may contact the ground, preventing the user from making further progress.
Wheel locks keep the wheelchair stationary, preventing it from moving when the patient transfers in or out of the wheelchair, and from rolling inadvertently when stopped on an inclined surface. The type of wheel lock prescribed for a patient is determined by upper extremity strength, hand grip, and functional dexterity.
Hand rims are located on the outside of the wheel and are used to propel the wheelchair. Several types are available with each wheelchair model. Upper extremity strength, hand grip, amputations, contractures, spasticity, and presence or absence of dysesthesia are some of the factors to be considered when selecting the appropriate hand rim.
Armrests provide support for proper positioning of the upper extremities. Several options are available. The type of armrest chosen will depend on the patient’s mobility and his or her ability to perform ADLs. Examples follow:
Adjustable height, full-length, removable armrest—This type of armrest extends from the back to the front of the wheelchair, is removable, and is height-adjustable for proper positioning of the upper extremities. The length of this armrest will prevent a stroke patient from moving close to a table; however, some patients may require the longer length for stability and support during transfers.
Adjustable height, desk-length, removable armrest—This armrest extends from the back of the wheelchair forward to a point about three-quarters the length of the seat. The armrest is removable and has adjustable heights. Desk-length armrests allow the wheelchair to be positioned closer to a table or desk without removing the armrest.
Flip-back, non–adjustable height armrest—This type of armrest flips backward to allow for easier transfers; however, the height is not adjustable. The armrest remains attached to the wheelchair. The flip-back feature is beneficial because some patients have difficulty retrieving wheelchair armrests from the floor once they have been removed from the wheelchair. The patient may not require an adjustable-height armrest if the arm is properly supported.
Flip-back, adjustable-height armrest—This armrest flips backward for increased clearance and easier transfers, and the height is adjustable. Most patients require adjustable-height armrests for proper positioning of the upper extremities.
Space saver armrest (wraparound armrest) —The armrest is curved inward and decreases the overall width of the wheelchair without limiting the seat width.
Elevating arm rests—This style of armrest assists with edema control and proper positioning of the upper extremity. Several different styles are available.
Arm trough—An arm trough can aid hemiplegic patients with upper extremity positioning and prevent the arm from hanging at the side of the wheelchair, which could exacerbate shoulder subluxation.
Trays are available for hemi-wheelchairs that can be used for meals or performing ADLs. Trays provide increased work surface for activities.
Most injuries among electric wheelchair users occur as a result of tipping and falling accidents. Many of these accidents occur when ascending curb cuts, ascending a 45-degree curb, or descending a 5-degree ramp. Research studies have found that leg rests and seatbelts provide restraint and reduce the risk of being ejected from the wheelchair, and increase safety when traversing common obstacles. Seatbelts provide stability and safety to the patient, and the type of seatbelt prescribed is based on patient preference and upper extremity strength and functional ability. Wheelchair seatbelt types include auto, airplane, and Velcro.
More than 40 different types of cushions are available for wheelchairs. Wheelchair cushions are designed for comfort; some also improve pressure distribution and prevent pressure ulcers, or improve pelvic stability. The type of cushion prescribed for a wheelchair user should be based on the patient’s individual needs. Some patients require only a basic cushion for comfort, because they are able to weight shift, transfer, and ambulate. Nonambulatory wheelchair-bound patients who are unable to transfer and stand independently require a more complex seat cushion that will prevent pressure ulcers and provide truncal and pelvic stability.
Basic foam cushions are used mainly for comfort. Skin-protective cushions may be made of foam, air, or gel and are recommended for patients with current skin breakdown or those at high risk for breakdown. Positioning cushions are mainly designed for patients who need support to maintain a proper sitting posture. Combination skin-protection and positioning cushions are designed for patients who have skin breakdown issues and need support to maintain proper positioning in a wheelchair.
The basic foam cushion for a wheelchair is a 2-inch (5-cm) polyfoam cushion with a cover. One example, the Jay basic cushion, is described as a soft molded foam cushion with mild contour to provide posture stability. This cushion has a nonskid bottom with a Velcro attachment and a moisture-resistant cover. This type of cushion is ideal for patients with good functional ability, who can weight shift and have a lower risk for skin breakdown.
Gel-filled cushions range from basic cushions to custom-modified seat cushions for patients at high risk for skin breakdown. One example, the Jay 2 custom cushion, has a firm contoured foam base with more than 2 inches (5 cm) of gel in the gel pack, allowing it to conform to boney prominences. An accessories pack is available, which includes adductor wedges, hip guides, abductor pads, and pelvic obliquity pads. Additional gel packs can be added to the cushion to individualize it to patient needs. Some other examples of skin-protective cushions are the Invacare Matrix, a molded foam cushion with a dual layer of fluid sacs (gel), and the Matrix airflow cushion, which consists of a foam base and air flotation cells on top of the base. Many other options are also available. One example, the Pride Synergy cushion, has a molded foam base with a cutout over the sacral area and is available with the choice of either twin cell–fluid insets or viscoelastic foam inserts. Another protective cushion, the Supracor Stimulite, consists of flexible honeycomb cells, which flatten when compressed to relieve pressure. The cells are perforated to allow airflow and assist with stimulating capillary blood flow.
Patients who need moderate assistance in positioning can benefit from an air cushion with multiple air cells. This type of cushion can be used with or without a contoured silicone foam base that, additionally, provides lateral and preischial contoured support. An example of this type of cushion is the Pride Synergy Spectrum Air. The Jay 2 Deep Contour is an ultra-lightweight cushion containing 3 inches (7.6 cm) of gel arranged in a tripad design covering the coccyx and both buttocks. A 2-inch (5-cm) layer of soft foam lies below the gel pad, and the base is made of precontoured foam, which provides pelvic stability and helps with positioning. A third example of a positioning cushion is the Invacare Matrix Stabilite Contour, which provides pelvic stability and leg support. The cushion is fitted with a “ThinAir” bladder to assist with pressure redistribution.
Many type of cushions in this group provide dual benefits by relieving pressure and maintaining the desired position of patients in a wheelchair, thus preventing deformities. An example is the Jay 2 Positioning and Pride Synergy Solution cushion, which has a contoured foam base with twin cell gel inserts in the ischial area. A modification, the Pride Synergy Solution 1 cushion, consists of a high-density contoured foam base with thin gel overlay. Finally, the Invacare Matrix Flotech cushion is made of a molded foam cushion and a dual layer of fluid sacs (gel).
Many studies have evaluated the effectiveness of different wheelchair cushions on the prevention of sacral decubitus ulcers. One study in elderly nursing home patients found that skin-protective cushions (air, viscous fluid, and foam or gel and foam) lowered pressure ulcer incidence as compared with segmented foam cushions and should be used to help prevent skin breakdown. The inferior surface of the ischial tuberosity receives the greatest subcutaneous stress, and protection of this body part helps prevent pressure ulcers. Another research study noted that foam seat cushions up to 3.2-inch (8-cm) thick were effective in reducing subcutaneous stress to the area of the ischial tuberosity; however, increasing the thickness of the foam cushion beyond 8 cm was ineffective in reducing subcutaneous stress to the ischial tuberosity. Finally, foam inserts (viscoelastic polyurethane foam) such as those used in custom-molded wheelchair seats were found to produce lower peak interface pressures and better pressure distribution than gel inserts.
Several types of backrests are available for wheelchairs and scooters. The standard backrest on a manual wheelchair is a sling back. A sling backrest is usually made of nylon or vinyl upholstery and is lightweight and foldable. This type of backrest provides no lateral support to the trunk to assist with prevention or management of trunk alignment problems. Clinical research has shown that a sling backrest may affect sitting posture and produce kyphosis and posterior tilting of the pelvis, leading to deformities of the spine and pelvis. The sling backrest is prescribed for patients with good trunk control who have the ability to sit upright without support but is not appropriate for patients with poor trunk control.
Patients with poor trunk control may require a more rigid backrest with lateral trunk stability to help maintain proper wheelchair positioning. Rigid backrests range from basic low-cost styles that provide minimal support to semi-custom styles that provide posterior lateral pelvic stability and trunk support. Some styles have lumbar support, lateral support wedges, and posterior lateral support.
Semi-custom rigid backrest cushions are available that provide lateral support, posterior support, thoracic pads, lumbar pads, or sacral pads to accommodate different types of trunk or spinal abnormalities (Figure 41–3). Patients who sit in a wheelchair for long periods of time may also benefit from a more supportive backrest because prolonged wheelchair sitting with a sling backrest will cause the backrest to sag, especially if patients are obese.
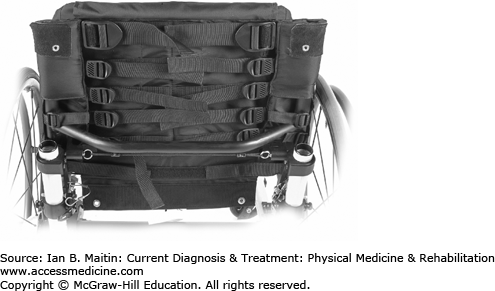
Adjustable-tension backrests consist of three to eight horizontally positioned adjustable straps for the thoracic, lumbar, and sacral regions (Figure 41–4). Tension is adjusted to the patient’s preference. This backrest provides more support than a standard sling backrest with limited lateral trunk support.
In addition to the basic standard wheelchair, several specialized wheelchairs are available, ranging from hemi-wheelchairs to heavy duty, and from sport to special-use categories, to suit the needs of specific patient populations. The prescription of a wheelchair for a patient involves the careful evaluation of the person who will use it to ensure the best match of a device with the individual’s functional abilities and planned activities. A brief survey of the main types of wheelchairs, and patients for whom they might be most beneficial, follows.
Stroke patients with hemiplegia or hemiparesis can benefit from the use of a hemi-wheelchair. Manual wheelchair propulsion requires the use of both upper extremities or of one arm and one leg for wheelchair maneuverability. The wheel axle on a hemi-wheelchair is set lower to the ground, which decreases the seat-to-floor height and allows the patient’s foot to touch the ground. A hemiplegic patient usually propels a manual wheelchair with one arm and one foot on the ground. The foot helps steer the direction of the wheelchair. A hemi-wheelchair can be constructed of standard aluminum or lightweight aluminum.
Stroke patients who are unable to push a standard hemi-wheelchair might be able to push a lightweight wheelchair. A lightweight wheelchair is lighter and easier to propel than a standard wheelchair. A lightweight wheelchair is made of aluminum, and the weight of this chair varies between 24 and 36 lb (11 and 16 kg), depending on the model, manufacturer, and optional equipment. The weight capacity is up to 250 lb (113 kg). Most lightweight wheelchairs have nylon upholstery to decrease the weight of the wheelchair. Some models are customizable regarding seat width, seat depth, casters, and wheel options to fit a variety of patients with different heights, body sizes, and disabilities. Ideally, patients with significant weakness should have a wheelchair evaluation to determine whether they are will be able to push a lightweight wheelchair or an ultra-lightweight wheelchair.
An ultra-lightweight wheelchair (high-strength lightweight) is the lightest of all manual wheelchairs and is manufactured by most wheelchair companies. The wheelchair is made of aluminum or titanium, a higher quality of aluminum. Titanium wheelchairs are more costly and often not covered by insurance companies. Ultra-lightweight wheelchairs have a high degree of adjustability and are customizable. This type of wheelchair can be easily adjusted to fit a stroke patient who requires a lower floor-to-seat height. The weight of the wheelchair varies from 14 to 26 lb (6 to 11 kg), and the weight capacity is up to 265 lb (120 kg) in some models. The frame choice for ultra-lightweight wheelchairs includes nonfolding and folding models. Nonfolding ultra-lightweight wheelchairs are popular with wheelchair users who want increased response and maneuverability and are willing to sacrifice the ease of portability for decreased weight.
Rigid ultra-lightweight wheelchairs are lighter in weight, without the folding mechanism and additional hardware. Folding models are easier to transport in an automobile but are heavier because of the folding mechanism and hardware. Some models are appropriate for patients with severe weakness who are unable to propel a lightweight wheelchair. Others are designed for very active patients. Wheelchair users report that ultra-lightweight wheelchairs are more comfortable and have better ergonomics than lightweight wheelchairs. Medicare reimburses the cost of this wheelchair only for individuals who engage in frequent activities that cannot be performed with a standard wheelchair or a lightweight wheelchair, or patients who require a seat width, seat depth, or seat height that cannot be accommodated in a standard or a lightweight wheelchair. The home environment is also important, because increased surface resistance, such as high carpet pile, decreases wheelchair velocity. The weight of the wheelchair also decreases self-selected wheelchair velocity and increases the resistive forces.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree