Weil Osteotomy and Dorsal Approach Plantar Plate Repair
Lowell Weil Jr
Lowell Scott Weil Sr
Second metatarsophalangeal (MTP) instability is a common problem associated with metatarsalgia (1,2) (Fig. 11.1). The development of this instability is due to a number of factors, of which plantar plate pathology is most critical (3, 4 and 5). The earliest description of the plantar plate can be credited to Cruveilhier (6), who described the plantar plate as a static structure that served to “protect” the lower portion of the lesser metatarsophalangeal joint (MTPJ) while increasing joint space area. More recently, authors theorized that the plantar plate serves as both a static and dynamic structure having attachments to the deep transverse intermetatarsal ligament, the lateral collateral ligaments, and the plantar fascia.
The plantar plate is one of the main stabilizers of the lesser MTPJ along with the collateral ligament complex (7, 8 and 9). It maintains stability in sagittal and transverse planes, and insufficiency may lead to MTP dislocation. Sectioning of the plantar plate will decrease the amount of force necessary to dislocate the MTP by an average of 30%, while sectioning of the collateral ligaments will decrease the amount of force needed to dislocate the MTP by 45%. Sectioning of both structures will decrease the amount of force needed to dislocate the MTP by 79%. It stands to reason, therefore, that pathology of the plantar plate needs repair in order to restore stability to the lesser MTP. This concept is similar to that of a Broström procedure for lateral ankle stabilization. When the primary stabilizing structure of a joint undergoes repair, the joint becomes more stable.
Plantar plate pathology can be responsible for symptoms in the region of the lesser MTPJ and metatarsalgia (Fig. 11.2). Patients may be misdiagnosed with other conditions, such as MTP capsulitis or neuroma. In a recent cadaveric study we found that 80% (16 of 20) of randomly selected specimens had plantar plate tears.
Symptoms of a plantar plate tear include pain in the ball of the foot that persists despite changes in shoes and activities, a second or third toe that appears to be changing position over time, and a neuroma that is unresponsive to treatment. As the lesser toe deformity progresses, greater positional changes will be appreciated in both the transverse plane and sagittal plane (Fig. 11.3). Hammer toe deformity will occur as the deformity progresses with crossing of the second toe over the hallux (crossover toe) and ultimately MTP dislocation.
INDICATIONS AND CONTRAINDICATIONS
Plantar plate repair is indicated in patients with clinical symptoms of plantar plate insufficiency (10). This is almost accompanied with a subtle or not so subtle elongation of the affected metatarsal (see Fig. 11.1). Plantar plate repair alone without the correction of underlying metatarsal may not provide lasting success. It is often necessary to correct the underlying deformity by shortening the metatarsal. Without metatarsal shortening, soft tissue correction will often fail over time. Not correcting the
metatarsal in this situation is much like addressing a posterior tendon dysfunction solely by repairing the tendon without changing the structural component with appropriate procedures.
metatarsal in this situation is much like addressing a posterior tendon dysfunction solely by repairing the tendon without changing the structural component with appropriate procedures.
 FIGURE 11.1 Anteroposterior (AP) foot radiograph shows a short first metatarsal and relatively long second metatarsal. This can contribute to metatarsalgia of the second. |
Plantar plate repair is not indicated for patients who have general or local conditions that preclude operative treatment such as skin ulceration, local or remote infection, or dysvascular foot, or for patients who are unable to comply with required postoperative immobilization and protected weight bearing. Neuropathy is a relative contraindication. The patient’s chronologic age is not as important a factor as physiologic age in considering this procedure. Patients with arthritic changes to the affected MTP may require a modification of the procedure where a partial metatarsal arthroplasty may need to be combined with the plantar plate repair rather than an osteotomy.
PREOPERATIVE PLANNING
Planning for a dorsal approach plantar plate repair includes a history, examination of the foot, general health evaluation, radiologic interpretation, and consideration of expectations. An ideal patient for a plantar plate repair describes the symptoms in realistic terms and has appropriate expectations.
A thorough clinical examination can suggest the possibility of plantar plate pathology. Patients will typically present with pain to the ball of the foot that is progressive in nature. They may complain of some numbness in the area, which could be related to localized swelling. The toe may change position over time by becoming more dorsally malaligned or valgus or, more commonly, by a varus deviation. There can be concomitant first ray pathology such as hallux valgus or hallux rigidus, but this is not always present.
In the most severe cases, there may be a crossover toe deformity or MTP dislocation (see Fig. 11.3). Hammer toe deformities may or may not be present. In early manifestations of disease, swelling at the plantar aspect of the MTP may be present. However, in the situation of complete tear, this may be absent. There will be pain at the plantar aspect of the MTP or distal aspect of the metatarsal head. A modified drawer test (Fig. 11.4) may yield instability in comparison to the contralateral foot or in comparison to the expected normal when bilateral disease is present. A drawer test will be painful in the patient with an incomplete tear but often painless with complete tear. There may be weakness of plantarflexion of the affected toe.
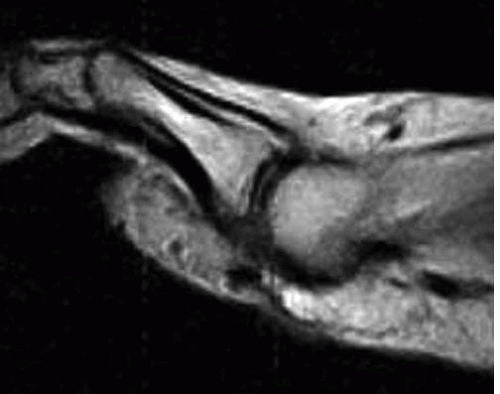
X-ray findings of bilateral weight-bearing films will often show an altered metatarsal pattern with the second metatarsal being slightly longer in comparison to the contralateral foot (see Fig. 11.1), transverse plane deviation of the digits, splaying of the digits, and a subtly increased metatarsus adductus angle (11). Interestingly, 60% of our patients had splaying of the second and third digits, and did not have an interdigital neuroma. In the past, advanced diagnostic studies were inconsistent at best. Magnetic resonance imaging (MRI) studies of an MTPJ rarely provided more than one or two sections through the joint, and visualization of the plantar plate was inadequate. More recently, MRI techniques have allowed a much higher level of appreciation of the MTPJ and plantar plate (see Fig. 11.3) (12,13). We looked at MRI correlation to intraoperative findings of plantar plate pathology. The overall accuracy of MRI in determining plantar plate pathology was 96%. This study also revealed a sensitivity of 95%, a specificity of 100%, positive predictive value of 100%, and negative predictive value of 67%. The MRI technique did not involve IV contrast or intra-articular contrast material.
We also looked at diagnostic ultrasound in comparison to MRI findings and intraoperative findings. The early results suggest that ultrasound evaluation of the plantar plate is highly technician dependent. Although the ability of the ultrasound and technician to detect the presence of plantar
plate pathology is relatively high (75%), the ability to accurately detect the location of the plantar plate pathology is very low (31%).
plate pathology is relatively high (75%), the ability to accurately detect the location of the plantar plate pathology is very low (31%).
 FIGURE 11.4 Dorsal drawer test of the second MTP joint is shown, with one hand securing the metatarsals and the other translating the phalanx dorsally. |
The specific surgical technique is in part dependent on the pathology of the plantar plate that is observed. Plantar plate pathology can be confirmed with direct visualization of this structure (10).
Grade I attenuation: Distinguishing features: Color changes of plantar plate, loss of pearly white color, more yellowish in appearance. Surgical treatment: Depending on overall laxity, attenuation may necessitate complete advancement.
Grade II button hole: Distinguishing features: Longitudinal tear at level of maximum weight bearing. Surgical treatment: This can repaired with side-to-side suture technique with Lasso.
Grade III partial tear: Distinguishing features: The most common tear (either medial or lateral) and usually occurs at the attachment of the plantar plate to the proximal phalanx. Often associated with deviation of the digit in the opposite direction of the tear and may have a concomitant collateral ligament tear or capsular injury. Surgical treatment: A complete tear of the plantar plate must be created and the plantar plate advanced and repaired.
Grade IV complete tear: Distinguishing features: Often associated with severe degeneration and infiltrative fibrosis of the plantar plate. Surgical treatment: This may necessitate plantar plate repair with concomitant flexor tenodesis augmentation.
SURGICAL TECHNIQUE
Peripheral block anesthesia is usually administered. The patient is positioned supine on the surgical table. A 4-inch rubber Esmarch bandage is applied around the foot and ankle for exsanguination and an ankle tourniquet is elevated to 250 mm Hg for hemostasis.
Approach
A linear incision (Fig. 11.5A) overlying the extensor apparatus is made extending from the distal one third of the metatarsal shaft to the midshaft of the proximal phalanx centering over the MTPJ.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree