Volar Plating of Distal Radius Fractures
John J. Fernandez
Philipp N. Streubel
DEFINITION
Distal radius fractures are defined by their involvement of the metaphysis of the distal radius.
They are assessed on the basis of fracture pattern, alignment, and stability:
Articular versus nonarticular
Reducible versus irreducible
Stable versus unstable
Irreducible or unstable fractures require surgical reduction and stable fixation.
Volar plating historically has been the method of choice for volar shear-type fractures.
Fixed-angle plates have become the preferred method of fixation for most types of distal radius fractures.
ANATOMY
The distal radius serves as a buttress for the proximal carpus, transmitting 75% to 80% of its forces into the forearm.
The remaining 20% to 25% of force is transmitted through the distal ulna and the triangular fibrocartilage complex (TFCC).
Thickness of distal radius articular cartilage is 1 mm or less.16
Dorsally
The distal radius is the origin for the dorsal radiocarpal ligament.
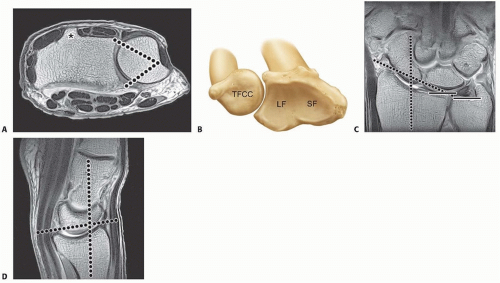
It is the floor of the fibro-osseous extensor tendon compartments and includes Lister tubercle, assisting in extensor pollicis longus function (FIG 1A).
The extensor tendons are in immediate contact with the dorsal surface of the distal radius.
Volarly
The distal radius is the origin for volar extrinsic ligaments of the wrist, including the radioscaphocapitate ligament and long and short radiolunate ligaments.
It also is the origin of the pronator quadratus.
The flexor tendons are separated from the distal radius by the pronator quadratus.
Ulnarly
The distal radius is the origin for the triangular fibrocartilage (see FIG 1A).
It also contains the sigmoid notch, which articulates with the head of the distal ulna, allowing forearm rotation.
Distally
The surface is divided into a triangular scaphoid fossa and a square lunate fossa articulating with each respective carpal bone (FIG 1B).
The distal articular surface is inclined approximately 22 degrees ulnarly in the coronal plane and 11 degrees volarly in the sagittal plane (FIG 1C,D).
The metaphysis is defined by the distal radius within a length of the articular surface that is equivalent to the widest portion of the entire wrist.
The dorsal cortical bone is less substantial than the volar cortical bone, contributing to the characteristic dorsal bending fracture pattern of distal radius fractures.
PATHOGENESIS
The mechanism of injury in a distal radius fracture is an axial force across the wrist, with the pattern of injury determined by bone density, the position of the wrist, and the magnitude and direction of force.
Most distal radius fractures result from falls with the wrist extended and pronated, which places a dorsal bending moment across the distal radius.
Relatively weaker, thinner dorsal bone collapses under compression, whereas stronger volar bone fails under tension, resulting in a characteristic “triangle” of bone comminution with the apex volar and greater comminution dorsal.
Other possible mechanisms form a basis for some fracture classifications such as the one proposed by Jupiter and Fernandez.6
Bending
Axial compression
Shear
Avulsion
Combinations
Articular involvement and its severity are the basis of some fracture classifications, such as the AO Orthopaedic Trauma Association (AO/OTA)10 and Melone12 classifications.
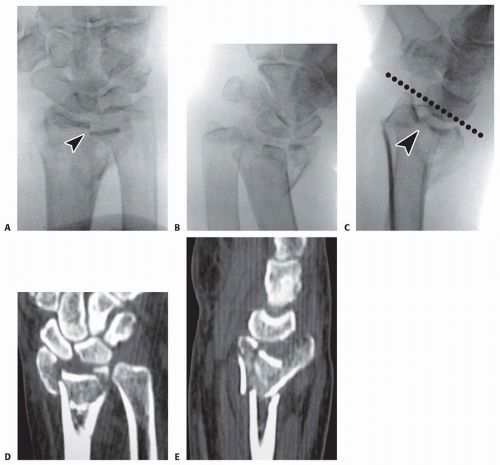
Articular involvement splits the distal radius into distinct fragments separate from the radius shaft (FIG 2):
Scaphoid fossa fragment
Lunate fossa fragment. With comminution of this fragment may be separated into two impacted articular fragments, involving the dorsal ulnar corner and the volar rim.11
NATURAL HISTORY
Clinical outcome usually, but not always, correlates with deformity.
Variable residual deformity can be tolerated best by individuals with fewer functional demands.
As wrist deformity increases, physiologic function is progressively altered.
The incidence of associated intracarpal injuries increases with fracture severity. Such injuries can account for poor outcomes. These injuries often are not recognized at first, leading to delayed treatment.4, 18
TFCC tears
Scapholunate and lunotriquetral ligament tears
Chondral injuries involving the carpal surfaces
Distal radioulnar joint injury
Distal ulnar fractures
By predicting the stability of a distal radius fracture, deformity and its complications can be minimized. Several risk factors have been suggested by LaFontaine et al8 and others. The presence of three or more indicates instability:
Dorsal (or volar apex) angulation greater than 20 degrees
Dorsal comminution
Intra-articular extension
Associated ulnar fracture
Patient age older than 60 years
PATIENT HISTORY AND PHYSICAL FINDINGS
The mechanism of injury should be sought to assist in assessing the energy and level of trauma.
Associated injuries are not uncommon and should be carefully ruled out.
Injuries to the hand, carpus, and proximal arm, including other fractures or dislocations
Injuries to other extremities or the head, neck, and torso
Establish the patient’s functional and occupational demands.
Document coexisting medical conditions that may affect healing such as smoking or diabetes.
Determine possible risk factors for anesthesia and surgery, such as cardiac disease.
The physical examination should document the following:
Condition of surrounding soft tissues (ie, skin and subcutaneous tissues)
Quality of vascular perfusion and pulses
Integrity of nerve function
Sensory two-point discrimination or threshold sensory testing
Motor function of intrinsic muscles, including thenar and hypothenar muscles, of the hand
Examination of the distal ulna, TFCC, and distal radioulnar joint should rule out disruption and instability.
Reliable physical examination of the carpus often is difficult, making radiographic review even more critical and followup examinations important.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Imaging establishes fracture severity, helps determine stability, and guides the operative approach and choice of fixation.
Plain radiographs should be obtained before and after reduction: posteroanterior (PA) (with the forearm in neutral rotation), lateral, and two separate oblique views.
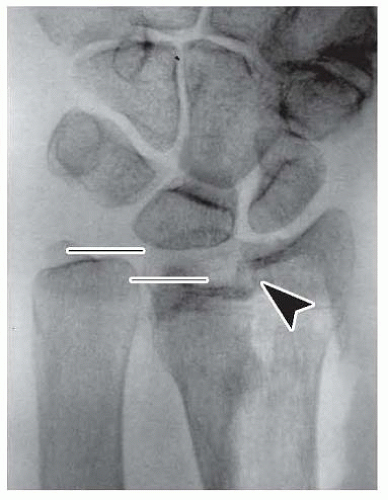
Oblique views, in particular, help evaluate articular involvement, particularly the lunate fossa fragment (FIG 3A,B).
The lateral view should be modified with the forearm inclined 15 to 20 degrees to best visualize the articular surface (FIG 3C; see TECH FIG 5B,C).
Fluoroscopic evaluation can be useful because it gives a complete circumferential view of the wrist and, with traction applied, can help evaluate injuries of the carpus.
Computed tomography (CT) helps define intra-articular involvement and helps detect small or impacted fragments, which may not be apparent on plain radiographs, particularly those involving the central portion of the distal radius (FIG 3D,E).
DIFFERENTIAL DIAGNOSIS
Diagnosis is directly confirmed by radiographs.
Associated and contributory injuries should always be considered.
Pathologic fracture (eg, related to tumor, infection)
Associated injuries to the carpus (eg, scaphoid fracture, scapholunate ligament injury)
NONOPERATIVE MANAGEMENT
Nonoperative treatment is reserved for distal radius fractures that are reducible and stable based on the criteria previously discussed.
The goal of nonoperative treatment is to immobilize the wrist while maintaining acceptable alignment until the fracture is healed.
Goals for treatment9
Radial inclination greater than 10 degrees
Ulnar variance less than 3-mm positive
Palmar tilt less than 10 degrees dorsal or 20 degrees volar
Articular congruity with less than a 2-mm gap or step-off
Patients are immobilized in a short-arm cast for 6 weeks. Radiographic follow-up is performed on a weekly basis for the first 2 to 3 weeks to identify fracture displacement that may warrant reduction.
SURGICAL MANAGEMENT
The goal of operative treatment is to achieve acceptable alignment and stable fixation.
Various methods of fixation are available: pins, external fixators, intramedullary devices, and plates (volar, dorsal, fragment specific).
Preoperative Planning
Preoperative medical and anesthesia evaluation are performed as required.
Discontinue blood-thinning medications (anticoagulants and nonsteroidal anti-inflammatory drugs, especially acetylsalicylic acid).
Request necessary equipment, including fluoroscopic and power equipment.
Confirm the plate fixation system to be used, and check the equipment before beginning surgery for completeness (ie, all appropriate drills, plates, and screws).
Have a contingency plan or additional fixation (external fixator, bone graft, or bone graft substitute).
Review and have previous radiographic studies available.
Consider use of a regional anesthetic for postoperative pain control.
Positioning
Place the patient in the supine position with the affected extremity on an arm table.
Apply an upper arm tourniquet, preferably within the sterile field.
Incorporate weights or a traction system to apply distraction across the fracture (FIG 4).
The surgeon is seated so that the elbow is pointing toward the patient’s torso and the dominant hand works toward the fingers of the patients.
The assistant is seated opposite the surgeon.
The fluoroscopy unit is brought in from the end or corner of the table.
Approach
Dorsal exposure allows for direct visualization of the articular surface when necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree