Hand Viva Alistair Hunter, Elliot Sorene and Max Horwitz 1. Clinical picture of a swan neck deformity. Describe the deformity, the underlying pathology and its classification. How will you manage this patient? Describe: – Hyperextension at the PIPJ – Flexion of the DIPJ Pathoanatomy: One of the common primary lesions is a lax volar plate, allowing producing hyperextension at the PIPJ from – Trauma – Rheumatoid arthritis – Generalised joint laxity Secondary lesions arise from an imbalance of forces at the PIPJ, from – volar subluxation of the MCPJ – Laceration or transfer of FDS (unopposed extension at PIPJ) – Intrinsic contracture (excessive extensor forces through the PIPJ), assess with Bunnell test – Mallet finger (extension of DIPJ extension force to the PIPJ) Classification (Nalebuff) and Treatment:

Type | Description | Treatment options |
I | PIPJ completely flexible | Splinting with double ring splints DIPJ fusion if mallet deformity significant Consider spiral oblique retinacular ligament reconstruction (SORL) |
II | PIPJ flexion limited in certain positions (tight intrinsics) | Lateral band translocation (Littler) Intrinsic release if necessary +/- MCPJ reconstruction |
PIPJ flexion limited in all positions | Dorsal release FDS tenodesis or lateral band translocation | |
IV | PIPJ stiff with radiographic changes | Arthrodesis – consider for index and middle finfers if stablitiy is important Arthroplasty |
Describe the deformity: what is the diagnosis?
What are the associations?
Name the different types of cord.
How would you manage this patient, and which incision(s) would you use?

Clinical picture of Dupuytren’s:
– Describe deformities, bands and cords
Epidemiology/associations:
– Northern European and Celtic descent (likely autosomal dominant with variable penetrance)
– Diabetes mellitus
– Epilepsy: controversial
– Alcoholic/smoker (controversial)
– Hypercholesterolemia
– HIV
Aetiological theories and associations:
– Genetic- increased incidence in relatives
– Traumatic: micro trauma
– Neoplastic
– Inflammatory
Associations:
– Ledderhose disease (plantar fascia, 5% of patients)
– Peyronie’s disease (Dartos fascia of the penis, 3% of patients)
– Garrod’s disease (knuckle pads)
Anatomy:
– Core of pathology is central palmar aponeurosis thickening
– Fascial involvement (bands) become pathologic cords
– Myofibroblast is the offending cell
– Increased levels of cytokines- IL/TGF/PDGF/FGF etc seen
Cords:
– Pre-tendinous cord: flexes MCPJ
– Central cord
– Lateral cord
– Spiral cord: from pre-tendinous band/spiral band/lateral digital sheet/Greyson’s ligament (pass deep to NV bundle- chance of injury during surgery, it displaces the neurovascular bundle)
– Natatory cord: cause web space contractures
– Abductor digiti minimi cord
– Commisural cords: dorsal/palmar- 1st web contractures
Clinical features:
– Cords – MCP flexed by pretendinous cord, PIP by central, spiral and lat cord
– Pits
– Nodules
– Garrod’s pads dorsally
– MC in ring and little fingers
– Inability to lay hand flat on a table i.e. failure of Huestons table top test.
Management:
Non-operative:
– Observe if good function or minimal contracture
– Nice Guidelines from 2010 have described radiotherapy but this is not a common treatment method
Operative:
Indications:
– Reduced function
– MCP >30 degrees
– PIP >15 degrees
Treatment of choice:
Partial fasciectomy
– 15% recurrence
– PIP not as successful as MCP
– Can result in residual contracture or fixed flexion deformity
– If >70 degree – very unlikely to achive full correction, and may need variable releases
– Incisions: Brunner, longitudinal with a Z-plasty
– Wounds in the palm can be left open: McCash open palm technique
Complications:
– Infection
– Delayed wound healing
– Incomplete correction
– Recurrence (30-50% at 10 years, (Bulstrode et al., 2005, Tonkin 1984)
– Neurovasular injury
– CRPS
– Amputation
Postoperative Management:
– Carefully applied bulky dressing providing compression
– Elevation
– Some advocate avoiding finger extension immediately from excessive tension on the wound
– Early wound check and initiation of active range of movement exercises
– May need extension splint at night
– Follow up for recurrence or involvement of other digits
Other procedures:
– Collagenase injections – sited directly into the cord and manipulation takes place the following day
– Percutaneous fasciotomy – in simple pretendinous palmar cord (45% recur)
– Segmental fasciectomy
– Total fasciectomy – not advocated at present
– Dermofasciectomy + skin graft – if recurrence with skin involvement. The full thickness skin graft is taken from the forearm or the groin (hair free) after excision of the diseased tissue and skin (‘fire-break’). Some surgeons advocate this as their main method of treatment.
– McCash open palm technique – the wound is left open and allowed to heal by second intention
3. Clinical picture of tendon transfer
What are the underlying principles of tendon transfer?
What are the transfers for ulnar, radial and median nerve injuries?
Principles:
1) Full passive joint range of movement of the joint
2) Sensation should be intact distally
3) Normal or near normal (grade 5) power in the donor
4) The donor should have good excursion
5) Synergistic muscle activity in the donor
6) No scar tissue in the operative field
7) The tendon lost should be expendable
Tendon Transfers
There are many tendon transfer procedures described for each pathology. Those mentioned below are a few of the most common.
Ulnar claw
– Aim to prevent hyper-extension at the MCPJs, thus allowing the extrinsic extensors to extend DIPJs and PIPJs
– One of the methods of bringing the MCPJ into flexion is by passing the FDS volar to the A1 pulley and suturing it back on itself (Zancolli Lasso proceure)
– MCPJ capsulodesis
Ulnar nerve palsy
– Thumb adduction: split insertion of middle finger FDS/BR to adductor pollicis brevis
– Index abduction: EIP or AbPL to first dorsal interosseus
– Wartenberg deformity: EIP to EDM
High ulnar lesion (loss of FCU and FDP)
– Suture FDPs to functioning index and middle FDP
– In addition, transfers for low lesion
Radial nerve palsy
– Wrist extension: pronator teres to ECRB/ERCL
– Finger extension: FCR or FCU to EDC
– Thumb extension: Palmaris longus to EPL
Median nerve palsy
Low lesion:
– Aim to regain opposition (loss of APB)- FDS ring/Abductor digiti minimi/PL to AbPB
High lesion:
– Thumb IP flexion (loss of FPL) – BR to FPL
– Index and middle flexion – side to side tenodesis of FDP to functioning FDP ring and little
– In addition, transfers for low lesion
4. Plain radiograph of scaphoid fracture 8 weeks old
How will you manage this patient?
How would you manage a non union?

Management:
– History for patient’s age, handedness, mechanism of injury, activity level, expectations, is there a delayed presentation?
– Assess the stability (Herbert classification, Herbert and Fischer, 1984)
– If there is doubt as to the configuration of a fracture or the presence of displacement, a CT scan should be requested.
– A displaced fracture is defined as more than 1 mm of displacement, >60 degrees of scapholunate, or 15 degrees of lunocapitate angulation
Herbert Classification
A | Acute, Stable | A1 | Tuberosity |
A2 | Incomplete fracture through waist | ||
B | Acute, Unstable | B1 | Distal oblique fracture |
B2 | Displaced fracture through waist | ||
B3 | Proximal pole fracture | ||
B4 | Trans-scaphoid perilunate fracture dislocation of the carpus | ||
Comminuted fractures | |||
C | Delayed Union |
| Widening of the fracture line, cyst development and density of proximal fragment |
D | Non-union | D1 | Fibrous unionRelatively stable with little or no deformity, likely to progress to pseudarthrosis, surgery is normally required |
D2 | Sclerotic non union (pseudarthrosis)Usually unstable, progressive deformity, leading to development of OA, surgery is normally required |
Non operative Management:
– If stable at plain radiography, apply short arm thumb spica for further 4 weeks explaining risks and benefits. If no signs of union at 12 weeks, operative intervention should be considered
Operative Management:
– If unstable fracture pattern
– If there is a delayed presentation
– Dias et al. (2005) advised early aggressive conservative management, whereby fracture healing is assessed by plain radiographs or CT at 6 to 8 weeks, and internal fixation with or without bone grafting if a gap is identified at the fracture site (95% union rate). They did not find any clear overall benefit in early operative intervention for non-displaced or minimally displaced fractures.
– McQueen et al. (2008) showed in a randomised controlled trial comparing conservative management versus percutaneous screw fixation for acute undisplaced fractures, that operative management gave significantly better results with lower rate of non-union and short times to return to work.
Difficult to come to firm conclusions given the wide variety of defining a non-union.
Percutaneous Technique:
– Dorsal approach requires a small open incision from risk to tendons and nerves. The wrist must be in flexion which can displace the fracture. Used in proximal pole fractures
– Volar approach can lead to increased prevalence of later scapho-trapezial degenerative joint disease, though usually asymptomatic
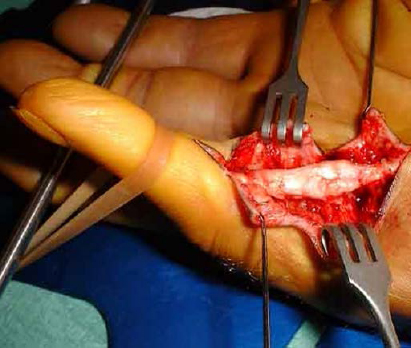
Non-union:
– Define the pathology with imaging (CT or MRI)
– Is there a Scaphoid Non-Union Advanced Collapse (SNAC)?
– Historically the Inlay (Russe) bone graft was indicated if there was no adjacent carpal collapse or humpback (flexion) deformity of the scaphoid (92% union rate). Otherwise, the Interposition (Fisk) graft was designed to restore scaphoid length and angulation when there was adjacent collapse or a humpback deformity of the scaphoid (72-95% union rates).
The modern approach uses a corticocancellous wedge graft from the iliac crest and a compression screw
– The wrist is extended and the two fracture fragments are gently distracted with spreaders
– The fracture surfaces are prepared with an osteotome or curette.
– The size of the graft can be calculated on the preoperative CT scan
– The graft is taken from the iliac crest with an osteotome (not an oscillating saw to avoid thermal necrosis of the graft)
– The graft is inserted on the palmar surface and the compression screw inserted, avoiding rotation of the graft with a supplementary K-wire
– Punctate bleeding at the proximal pole fracture site is the most reliable sign for a vascular proximal pole. If bleeding is obvious, the union rate is 92%, but if there is no bleeding the rate is 0%.
– Vascularised bone graft from the radius is harvested from the dorsal aspect of the distal radius, based on the 1,2 intercompartmental supraretinacular artery. Can be used when treating non-union in the face of AVN or revisions.
– A wrist denervation is a useful adjunct to treatment
– A limited radial styloidectomy can be added to the reconstruction if secondary radiocarpal OA has ocurred.
– Salvage procedures for advanved non union with collapse (SNAC) include a four corner fusion, proximal row carpectomy and wrist arthrodesis
5. Clinical picture of finger tip injury.
How will you manage this patient?
Discuss the options for soft tissue flaps.

The principle is to provide a sensate, well healed tip, and to preserve length (allowing bony support for the nail).
Can be divided into:
1) Soft tissue loss without bone exposure:
– Fingertip lacerations or avulsions of the substance smaller than 1 cm2 will heal by second intention, especially good in children. Some argue that wound contraction will lead to a hook nail deformity, but tight primary closure wound closure (drawing the nail bed over the tip) will lead to the same outcome and must be avoided.
– For wounds extending for more than 1 cm2, a local flap may be needed to cover the defect
2) Soft tissue loss with bone exposure:
– Exposed bone is not a satisfactory bed for healing. Even if they heal, skin at the tip is poor quality and easily broken down, leading to a chronic ulcer.
– If bone is exposed, the prominence must be shortened with excision back to rounded edges and primary, tension free, soft tissue closure performed. Bear in mind the need for bony support of the nail bed.
– If excessive bony debridement is required to achieve closure, soft tissue coverage is indicated.
Soft Tissue Coverage Choices:
– Advancement flap from the same finger has the advantages of rapid healing, maintenance of sensation and limited morbidity.
– The aim is to free the skin from the septae anchoring it to bone, whilst retaining the nerves and vessels, allowing a tension free advancement.
1) Options for straight or more dorsal tissue loss:
– Volar V-Y advancement (Atasoy)
– Double lateral V-Y advancement flap (Kutler)
2) Options for more volar tissue loss:
– Cross finger flap, but scars the adjacent finger
– A rectangular flap is raised from the three sides of the dorsal surface of the middle phalanx of the adjacent digit.
– The flap is normally based on the lateral side of the adjacent digit and swung on its pedicle and sutured in place.
– The flap is divided within two weeks to avoid stiffness of the fingers.
– Thenar flaps can be considered, are well tolerated in children, but can lead to PIP joint stiffness in adults.
3) There are more complex advancement flaps but these should be performed by experienced surgeons
Terminalisation:
– Indicated for a severely crushed distal phalanx
– The level is through the DIPJ, trimming the condyles of the middle phalanx
– Aim to preserve the FDS and achieve tension free primary closure
– Digital nerves are transected as proximally as possible
– A volar skin flap is created and the wound is closed dorsally
6. Plain radiographs of Madelung deformity of the distal radius.
What is the diagnosis, and how does the condition arise?
Discuss the management of this condition.

The deformity results from premature fusion of the ulnar and volar aspect of the distal radial epiphysis. As the child grows, the distal radius develops increased radial inclination and volar tilt, and ulnar-carpal impaction.
Presents more frequent in females, those with a positive family history and is often bilateral.
Causes:
– Usually idiopathic
– Congenital dysvhondrosis
– Post traumatic
– Dysplastic (Ollier’s disease, achondroplasia, multiple epiphyseal dysplasias)
– Genetic (association with Turner’s syndrome and Leri-Weill dyschondrosteosis).
Clinical manifestations:
– Insidious onset of wrist pain (radioulnar impaction)
– Development of prominence of the dorsal ulnar head
– Bowing of the distal radius
– Limitation of forearm rotation.
– Determined by the degree of deformity, the degree of closure of the growth plate (? progressive) and the severity of the symptoms.
Nonoperative management:
Monitor patients without pain
Operative management:
Aims to either correct deformity or relieve pain and improve function (or both):
– Prevent further deformity if the growth plate is open, with epiphysiodesis, and a closing wedge osteotomy to correct the deformity
– Release of the Vickers Ligament, a tethering structure
– Include ulnar shortening if it is long and sypmtomatic and distal ulnar epiphysiodesis if the growth plate is open
– Alternatively one can include radial lengthening.
– For symptomatic relief, a Sauve-Kapandji procedure will decrease ulnar sided wrist pain and increase range of movement, or consider Darrach’s procedure (though risks instability).
– For adults with severe pain and instability, a wrist arthrodesis is suitable.
7. Plain radiographs of fractures of the 4th and 5th metacarpal shafts.
What is the management of these fractures?
How will you undertake open reduction and internal fixation?
What is your approach?
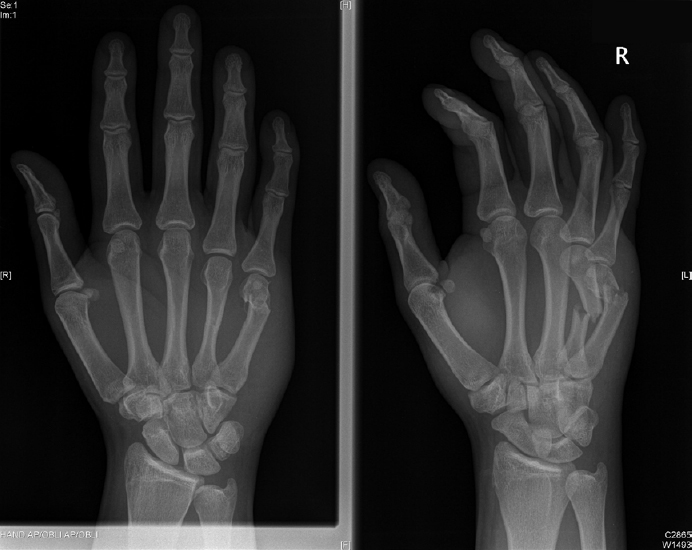
– The displacement of metacarpal fractures is normally reduced by the intermetacaral ligaments, the intrinsic muscles and the adjacent metacarpal, but the border metacarpals are not supported as stably as the middle and ring metacarpals.
– This anatomical splinting is lost in this fracture pattern; therefore, there is a lower threshold for fracture fixation.
– In addition, with shortening of the metacarpals comes loss of extension (with each 2 mm of shortening there is a 7 degree extensor lag at the MCPJ (Strauch et al., 1998) from changes in the relationship between flexors and extensors.
Ensure:
– There are no associated soft tissue injuries (fight bite) that need to be addressed
– The soft tissues overlying the fractures are intact
– Any rotational deformity is noted preoperatively
– There is no dislocation of the 4th or 5th CMCJs, clinically or radiologically
– There is no other associated phalangeal fracture
Management:
Open reduction and internal fixation with dorsal plating is the method of choice:
– Dorsal longitudinal incision between 4th and 5th metacarpals
– Retract the tendons over either fracture
– Decide whether a lag screw (1.7 mm) with a neutralisation plate is appropriate or amini-fragment DCP (2.0 mm). Hand locking plates are also available.
– For screw only fixation, the ratio of the length of the oblique or spiral to the diameter of the bone must be at least 2:1. The screw must also pass though the spike in an area that is more than 3 times the width of the screw to avoid comminution
– Plate fixation on the dorsal side of the metacarpal allows a tension band effect.
– Prebending the plate just beyond the normal metacarpal bow avoids opening of the volar apect of the fracture
– At least six cortices proximally and distally
– Always re-evaluate rotation one final time before closure
– Postoperatively, early active motion to avoid finger stiffness and tendon adhesions to the plate (though less frequent than in phalangeal fractures).
8. Draw incisions for the hand and explain the underlying principles.
Surgical scars contract and in the palm can cause fixed flexion deformities of the fingers.
A good incision should:
– allow for extensile exposure
– provide well vascularised skin flaps
– allow for lengthening of the wound
– should cross flexion creases transversely or obliquely
Three incisions commonly used in the hand give excellent exposure.
The Z-plasty:
– A straight, midline, longitudinal incision is made
– When z-plasty flaps are transposed, there is lengthening in the longitudinal axis and shortening in the transverse axis (McGregor, 1967)
– Increasing the Z-plasty angle increases the amount of lengthing
– A standard Z-plasty of 60 degrees gives a longitudinal lengthening of 75%.
– When planning, the transverse limb after transposition should lie in a flexure line, both in the digit and the palm
– A continuous multiple Z-plasty should be planned for longer incisions
Drawing the Z-plasty:
1. Draw the longitudinal incision
2. Draw a perpendicular dotted line perpendicular to the incsion at the skin crease
3. Draw two parallel lines at 60 degrees to the incision that meet at each of the lateral borders of the dotted line
4. The flaps marked then cross over, with the parallel lines then meeting at the dotted line
Brunner Incision (Brunner, 1967):
– A zig-zag volar incision with the apex at the finger flexor crease
– The skin flaps are full thickness
– The angle should be no less than 60 degrees to avoid necrosis at the apex
– The neurovascular bundle is vulnerable at the apex of the incisions
The Mid-axial Incision:
– The site for the midaxial incision is marked by flexing the finger and marking the point at each joint where the flexion crease ends. The dots are then connected.
– The digital artery and nerve lie approximately 2 mm volar to the margin of incision, so preserve the fat on the volar flap
– On the radial side of the index and middle and the ulnar side of the ring and little fingers there is a dorsal branch of the digital nerve that should be preserved
9. Plain radiographs of osteoarthritis of the CMC joint.
What is the management of this condition?
What is the evidence for excision vs arthrodesis vs arthroplasty?

Non-operative Management:
– For mild symptoms this is the first line treatment
– Splints can be used (thumb spica)
– NSAIDS
– Activity modification
– Injections – Heyworth (2008) showed in a prospective, randomised, double blinded trial that steroid, hylan and saline were all equally effective at reducing pain and increasing thumb function at three months
Operative Management:
Trapeziectomy +/- further procedure:
-Trapeziectomy (excision arthroplasty)
Concerns with thumb weakness from shortening
Modifications to this technique were developed:
-Trapeziectomy with palmaris longus interposition (interposition arthroplasty)
-Trapeziectomy with ligament reconstruction and tendon interposition (50% FCR) (LRTI). The aim is to support the base of the first metacarpal and prevent thumb shortening.
The evidence:
– Davis et al. (2004) radomised 162 women with 183 procedures over 9 years with Eaton Grade II to IV to one of the above three procedures.
– Three months postoperatively, pain had significantly improved in all groups, with further improvement by one year, with no difference between groups.
– No difference in thumb-key and tip-pinch strength or grip strength between groups
– However, all patients were immobilised with a K-wire for four weeks, which is not standard practice, and may have increased the stability of the pseudarthrosis in the trapeziectomy alone group.
– Longer term outcomes may be different.
Arthrodesis:
– A choice in younger patients and manual workers with isolated CMCJ arthrosis
– The aim is to provide good pain relief, stability of the thumb and maintenance of thumb length
– The thumb is fused in a clenched fist position to allow maintenance of better grip strength. However, the operation is technically difficult with only a small area for bony union
– In addition there is loss of movement and the procedure does not address STT symptoms.
The evidence:
– It is difficult to assess whether arthrodesis is superior to other methods given lack of good quality evidence
– In a systematic review, the non-union rates ranged between 8 and 21%, with are high rate of complications and revision operations with this procedure (Vermeulen, 2011).
Joint Replacement Arthroplasty:
The evidence:
– Total joint replacement has shown in one study to have faster convalescence, better strength and patient comfort compared to trapeziectomy and LRTI, but the follow up was only one year (Ulrich-Vinther et al, 2008)
– There are concerns about longer term survival with loosening and dislocation.
Osteotomy:
The evidence:
– Abduction-extension osteotomy can provide good results for early disease (Stage I and II OA), but patients with Stage III did better with an LRTI in a retrospective study (Atroshi et al., 1998).
Overall:
– There is no hard evidence that one technique is superior to another in a systematic review (Vermeulen et al., 2011)
– A good result is achieved in 80-90% of patients
– The stage of the disease, the rehabilitation time, the daily demands of the patient and the surgeon’s experience are considerations in chosing the technique.
10. Clinical picture of flexor tendon injury in zone 2.
Describe the flexor tendon zones.
How would you manage this injury and what are the post operative regimes.
Draw the flexor pulleys. How will you reconstruct them?

An injury to the flexor tendons is described according to the the Zone of Injury:
Zone | Site | Description of Injury |
Zone I | Distal to FDS tendon insertion | Rugby-jersey finger |
Zone II | FDS insertion to A1 pulley | Bunnell’s ‘No man’s land. This zone is unique in that FDP and FDS are enclosed in the same tendon sheath |
Zone III | Palm | Often associated with a neurovascular injury, carrying a worse prognosis |
Zone IV | Carpal tunnel | Often complicated by adhesions |
Zone V | Proximal to carpal tunnel | Often associated with a neurovascular injury, which carries a worse prognosis |
Thumb | FPL insertion to A2 pulley | Outcome is different to finger flexor tendon repairs. Early range of motion protocols do not improve long term outcomes There is a higher re-rupture rate than in finger flexor tendon repairs |
T II | A2 pulley to distal A1 pulley | |
T III | A1 pulley to carpal tunnel |
Principles:
– Repair if laceration greater than 60% of tendon width (Al-Qattan, 2000)
– Repair as early as possible, definitely within three weeks, as tendon retraction complicates the procedure
– Incision should allow lengthening and cross flexion creases obliquely or transversely
The technique:
– The strength of the repair is dependent upon the number of core strands crossing the repair site in a linear relationship
– Four core strands are required for early active motion (Strickland, 1995)
– Use a 3,0 non-absorbable suture
– Circumferential suture uses a 6,0 non absorbable suture that reduces tendon gapping
– It is essential to preserve the A2 and A4 pulleys
Postoperative Regime:
Principles:
– Mobilize early to prevent adhesions and to allow increased tendon excursion
– Postoperative controlled mobilisation has been the major factor in improved outcomes
– Tendon healing has three phases (inflammatory, fibroblastic and remodelling) and the repair is weakest at Days 6-12 postoperatively
– Active (Belfast) and Passive (Kleinert, Duran, Mayo) protocols
– Children are immobilized postoperatively
Belfast:
– Dorsal blocking splint is used with the wrist in 20 degrees and MCPJ in 70 degrees of flexion.
– ‘Place and hold’ exercises
Kleinert:
– Elastic bands allow attached to distal phalanx crossing the volar aspect of the wrist allow dynamic splint assisted passive flexion but active extension.
Draw the pulleys:
– Odd numbers are at the level of the joints
– Even numbers are at the level of the phalanx
Pulley | Level |
A1 | MCPJ |
A2 | Proximal phalanx |
A3 | PIPJ |
A4 | Middle phalanx |
A5 | DIPJ |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







