, Antonio Cesarani2 and Guido Brugnoni3
(1)
“Don Carlo Gnocchi” Foundation, Milano, Italy
(2)
UOC Audiologia Dip. Scienze Cliniche e Comunità, Università degli Studi di Milano, Milano, Italy
(3)
Istituto Auxologico Italiano, Milano, Italy
Abstract
Bilateral vestibular hypofunction (BVH) produces a variety of clinical problems, including impaired balance control, inability to maintain stable blood pressure during postural changes, difficulty in visual targeting of images and disturbances in spatial memory and navigational performance. The cardinal symptoms are motion-dependent postural vertigo with unsteady gait and stance, particularly in darkness and on uneven ground (vestibulospinal functional impairment), together with oscillopsia and blurred vision when walking or moving the head (impairment of the vestibulo-ocular reflex). The key impairments are head dynamic instability with oscillopsia, postural instability with unsteadiness and cognitive (navigation) problems. Recovery is strictly dependent on compensation and thus rehab plays the major role in the therapeutic planning. Rehab with gait and balance training helps the patient adapt to the functional deficit by maximizing the potential for visual and sensorimotor compensation. Treatment must be pointed to (1) increase dynamic head stabilization, (2) increase antigravitary paravertebral tone, (3) restore correct ankle–hip strategies dynamic, (4) restore eye–head coordination, (5) decrease oscillopsia and (6) avoid disorientation
Bilateral loss of vestibular inputs affects far fewer patients than unilateral inner ear damage [1]. Bilateral vestibular hypofunction (BVH) produces a variety of clinical problems, including impaired balance control, inability to maintain stable blood pressure during postural changes, difficulty in visual targeting of images and disturbances in spatial memory and navigational performance. The cardinal symptoms are motion-dependent postural vertigo with unsteady gait and stance, particularly in darkness and on uneven ground (vestibulospinal functional impairment), together with oscillopsia and blurred vision when walking or moving the head (impairment of the vestibulo-ocular reflex). Patients with BVH are typically symptom-free when sitting or lying.
BVH involves circumscribed atrophy of the hippocampus with impairments of spatial memory and navigation and is the most frequent cause of motion-dependent postural vertigo in older patients.
There are many possible causes of BVP; the three most frequently identified are:
Ototoxic aminoglycosides
Bilateral Menière’s disease [2]
Meningitis
Antibiotic treatment with aminoglycosides is the most frequently determined cause of bilateral vestibulopathy. This class of drugs should therefore be used very sparingly, particularly since their ototoxic effect has a latency of several days.
One connection between BVH and degenerative cerebellar diseases has now been clearly established as cerebellar ataxia, neuropathy and vestibular areflexia syndrome (CANVAS) [3].
CANVAS comprising BVH in combination with sensory axonal polyneuropathy, cerebellar ataxia and oculomotor disturbances is responsible for around 30 % of the cases previously classified as idiopathic [4].
Despite a multitude of visits to the doctor, BVH is usually diagnosed too late, which amplifies the patient’s symptoms.
The key impairments are head dynamic instability with oscillopsia, postural instability with unsteadiness and cognitive (navigation) problems.
Recovery is strictly dependent on compensation and thus rehab plays the major role in the therapeutic planning. Experiments in animals have shown that non-labyrinthine inputs to the vestibular nuclei are rapidly amplified following the onset of BVH, which may explain the recovery of postural stability and orthostatic tolerance that occurs within 10 days. However, the loss of the vestibulo-ocular reflex and degraded spatial cognition appear to be permanent in animals with BVH. Current concepts of the compensatory mechanisms in humans with BVH are largely inferential. Translation of animal studies of compensation for BVH into therapeutic strategies and subsequent application in the clinic is the most likely route to improve treatment [5].
In addition to physical therapy, prosthetic devices have been proposed to treat individuals with bilateral loss of vestibular inputs. The relative efficacy of this treatment paradigm, and whether it can be combined to facilitate recovery, is yet to be ascertained [6].
Rehab with gait and balance training helps the patient adapt to the functional deficit by maximizing the potential for visual and sensorimotor compensation. Treatment must be pointed to:
1.
Increase dynamic head stabilization
2.
Increase antigravitary paravertebral tone
3.
Restore correct ankle–hip strategies dynamic
4.
Restore eye–head coordination
5.
Decrease oscillopsia
6.
Avoid disorientation
7.1 Exercises in the Gymnasium
7.1.1 First Week
1.
Relaxation exercises such as control of breathing with improving consciousness of abdominal or thoracic breathing. A simple exercise consists of deep inhalation followed, after few seconds, by a forced exhalation pronouncing the word “one”. This exercise is repeated 8–10 times.
2.
In the quadrupedal position, the patient inhales and arches her/his back (hyperkyphosis). She/he then exhales and rotates her/his pelvis in hyperlordosis. A small laser pointer (Fig. 7.1) is fixated on the patient’s head; during both phases, the head is maintained straight in order to point the laser spot on a target placed on the wall.


Fig. 7.1
A low-cost laser pointer easy to fixate on the patient’s head through a Velcro band
3.
A small laser pointer is fixated on the patient’s head. From supine position, the patient shifts to sitting position, pointing the laser spot on a target straight in front of her/him (Fig. 7.2).
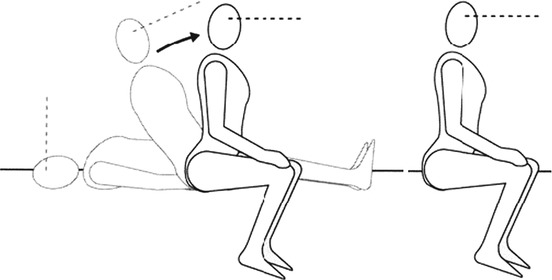
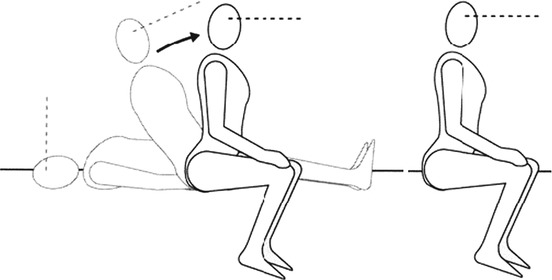
Fig. 7.2
From the supine to sitting position fixating a target (Originally published in Cesarani and Alpini [15] published by Springer © 1999)
4.
In the sitting position, the patient grasps a stick with both hands and takes the stick behind her/his shoulder, positioning the stick at the level of the cervico-dorsal junction. In this position she/he pushes the stick against her/his back, exhaling and inhaling rhythmically and slowly. She/he then repeats the exercise, moving the stick forward on the sternum at the level of the sterno-clavear joint. The patient grasps the stick with the hands frontally positioned. The patient maintains the fixation of a target placed on the wall, wearing pinhole glasses.
5.
The patient is standing on both legs and wearing pinhole glasses. The patient fixates her-/himself in a mirror. The therapist helps the patient to align her/his position correctly. She/he must maintain equilibrium for 1 min with eyes open and then close her/his eyes, visualizing her/his correct position while remaining in this position for at least 1 min.
6.
The patient is standing on one leg, wearing pinhole glasses. The patient fixates her-/himself in a mirror. The therapist helps her/him to align her/his position correctly. She/he must maintain equilibrium for session of at least 10 s each. After 5–7 repetitions on one leg, the same exercise is performed with the patient standing on the other leg.
7.1.2 Second Week
The following exercises have to be performed during TENS cervical stimulation, placing the electrodes on the paravertebral muscles of both sides and magnifying lenses (Fig. 7.3) to obtain visual image magnification [6].
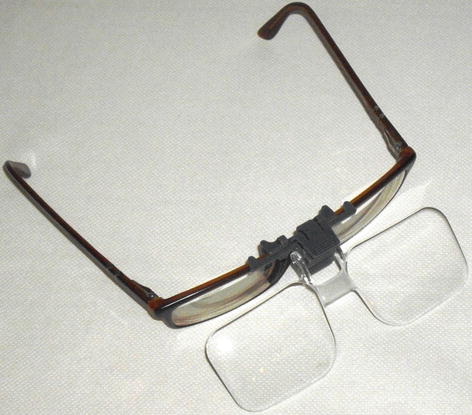
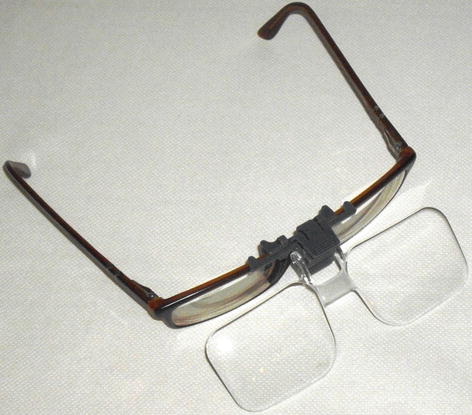
Fig. 7.3
Magnifying lenses to be applied to the patient’s glasses or to a neutral lens glasses
1.
The patient is standing on a soft mattress and fixates her-/himself in a mirror. The therapist helps her/him to align her/his position correctly. She/he must maintain equilibrium for 1 min with eyes open and then close her/his eyes, visualizing her/his correct position while remaining in this position for at least 1 min.
2.
Get Clinical Tree app for offline access

The patient fixates her-/himself in a mirror (Fig. 7.4a). Then she/he oscillates right and left (Fig. 7.4b), around her/his pelvis. She/he then resists the therapist’s attempts at destabilizations (Fig. 7.4c) and maintains equilibrium by crossing the legs (Fig. 7.4d).
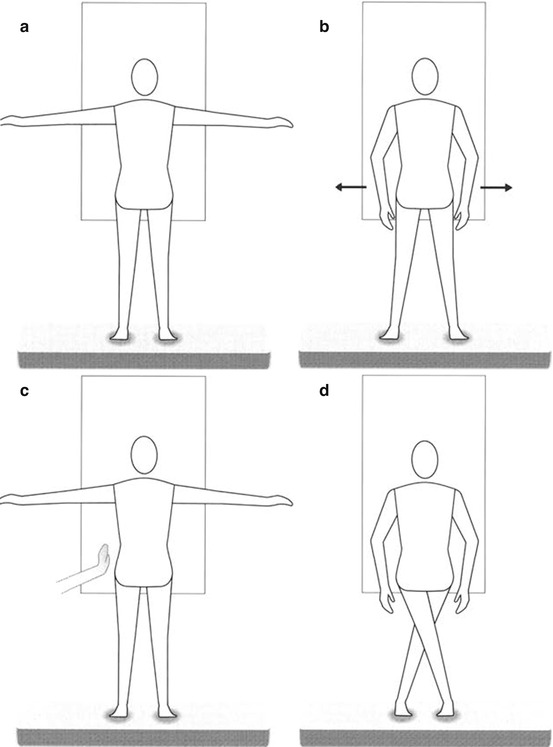
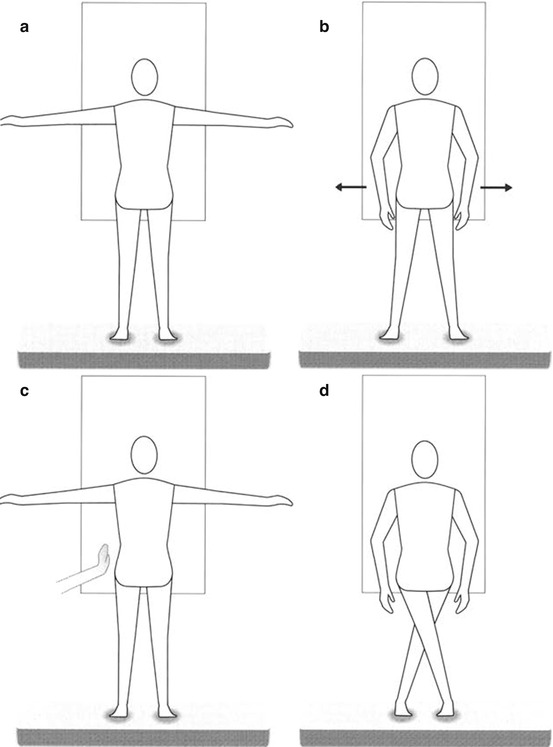
Fig. 7.4




The patient aligns himself looking at a mirror (a), then he oscillates (b), then resists when the therapist destabilizes him (c) or he maintains equilibrium by crossing the legs (d) (Originally published in Cesarani and Alpini [15] published by Springer © 1999)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







