Vertebral Column Resection for Severe Rigid Spinal Deformity through an All Posterior Approach
Michael P. Kelly
Lukas P. Zebala
Lawrence G. Lenke
DEFINITION
Posterior vertebral column resection (VCR) entails the removal of the anterior, middle, and posterior columns of the vertebra(e) through a posterior-alone approach.
VCR is often performed at the apex of a deformity for severe, rigid scoliotic and kyphotic spinal deformities.
ANATOMY
A thorough understanding of the anatomy of the vertebral segment and spinal cord is needed to safely perform this procedure. This includes understanding the peculiarities of rotated vertebral segments in severe scoliotic deformities. The morphologic and iatrogenic changes of the posterior elements must be appreciated, as must the course of the spinal cord and nerve roots.
PATHOGENESIS
The origins of these deformities are multiple and varied, including congenital, idiopathic, neoplastic, traumatic, and iatrogenic causes.
NATURAL HISTORY
The natural history of the diseases leading to severe scoliotic, kyphotic, or combined deformities are variable.
Those that do progress to severe, rigid deformities may present with intolerable deformity, severe pain, decreased ability to perform activities of daily living, myelopathy/spinal cord compression, and pulmonary dysfunction.
Those fixed deformities that are asymptomatic (ie, a well-balanced patient without complaint) may be managed non-operatively. However, one must obtain careful follow-up to assess for possible deformity progression over time.
PATIENT HISTORY AND PHYSICAL FINDINGS
The overall coronal and sagittal plane balance should be observed with the patient standing upright.
The deformity should be assessed for any flexibility by placing the patient prone and supine on the examination table. Several minutes of supine positioning will allow one to assess the flexibility of a kyphotic deformity. Often, we will have the patient lie supine on the examining table, turn the lights off, and return in 15 to 20 minutes for repeat evaluation.
The history should include a careful assessment of current pain medication usage as preoperative narcotic usage may complicate the perioperative care. Additionally, any medications that may confer a risk of increased bleeding (eg, aspirin) should be noted and the patient cautioned to stop them prior to surgery.
The use of nicotine-containing products, particularly cigarettes, is a relative contraindication to this procedure as the risk of pseudarthrosis is increased as well as perioperative complications.
Those patients with diabetes mellitus must have well-controlled blood glucose levels before surgery as uncontrolled blood glucose levels are associated with increased risk of perioperative infection.
A patient’s nutritional status should be assessed and optimized prior to surgery. In addition, a bone density test should be performed to diagnose presence of osteoporosis and initiate preoperative treatment of any deficiencies.
The patient’s gait should be assessed for evidence of myelopathy (eg, wide based, shuffling gait).
A detailed neurologic examination must be performed and documented, including examination for pathologic reflexes such as asymmetric abdominal reflexes, Babinski response, and sustained clonus. Pathologic reflexes must alert the surgeon to possible intraspinal pathologies (eg, Chiari II, syrinx, tethered cord) that may need to be addressed prior to the deformity correction.
Preoperative examinations by a primary care physician, a cardiologist (including stress testing as indicated), and an anesthesiologist is mandatory to mitigate any risks of perioperative morbidity and mortality.
A review of systems should include a review of the respiratory system and any history of respiratory compromise or distress. Preoperative pulmonary function tests should be obtained in all patients with a deformity severe enough to be considered for a VCR procedure.
IMAGING AND OTHER DIAGNOSTIC STUDIES
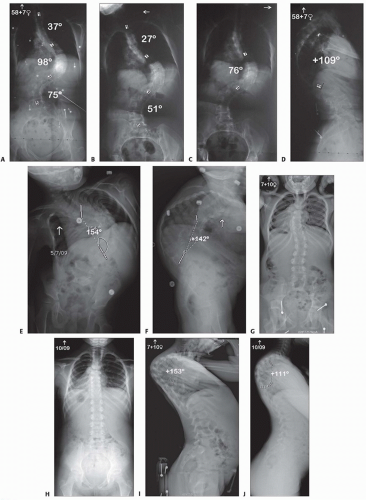
A radiographic spinal deformity series is obtained, which includes standing anteroposterior (AP) and lateral long-cassette radiographs, left and right side bending, full AP, and lateral supine or prone images (FIG 1).
Flexibility radiographs include push-prone and axial traction x-rays and help assess coronal plane rigidity.
Hyperextension radiographs (bolster placed at apex of kyphosis) and hyperflexion radiographs (bolster at apex of lordosis) help assess sagittal plane rigidity.
A three-dimensional (3-D) computed tomography (CT) scan is obtained to evaluate the entire anterior and posterior spinal column. This aids in the identification of important vertebral landmarks (FIG 2).
Skull to sacrum magnetic resonance imaging (MRI) is necessary to evaluate the entire neural axis (eg, Chiari malformation, syringomyelia, tethered spinal cord) (FIG 3).
DIFFERENTIAL DIAGNOSIS
Severe scoliosis
Global kyphosis
Angular kyphosis
Kyphoscoliosis
Fixed coronal and sagittal imbalance syndrome (eg, status post-Harrington rod instrumentation)
NONOPERATIVE MANAGEMENT
Patients with static deformities and only mild pain or physical impairment should be managed with a trial of nonoperative therapy.
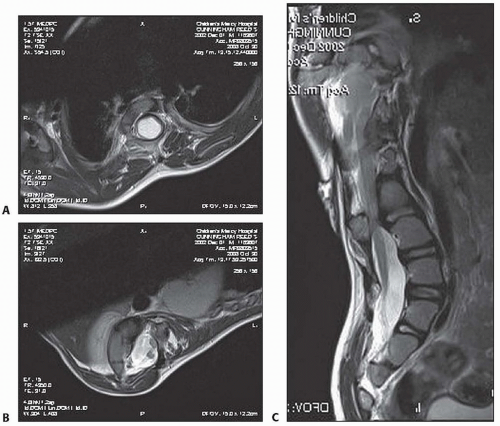
FIG 3 • A-C. Case 2. Patient’s total spine MRI demonstrated a syringomyelia, diplomyelia, and a tethered spinal cord.
This includes a directed physical therapy program, to include cardiovascular conditioning, postural training, and abdominal strengthening.
For those patients with moderate to severe pain, a referral to a pain specialist, most notably for those patients with complaints of pain not consistent with their presenting pathology or other signs of nonorganic causes of pain
As with nerve root compression, epidural and transforaminal steroid injections offer a less invasive, potentially diagnostic and/or therapeutic intervention.
SURGICAL MANAGEMENT
Classically, rigid deformities were treated with staged anterior and posterior procedures to resect and reconstruct the spine through the rigid segment.2, 3, 4 The posterior VCR allows a similar correction of deformity, with the benefits of shorter total operative time and lower blood loss.6
Location of the deformity often determines whether a VCR (thoracic) or pedicle subtraction osteotomy (lumbar) will assist in correction of sagittal imbalance. For less severe and flexible deformity with mobile disc spaces, multilevel Ponté/Smith-Petersen osteotomies may be adequate for deformity correction.1
Flexibility films will help determine whether a three-column osteotomy is needed versus posterior column osteotomies alone. Posterior column osteotomies may on average correct 10 degrees of kyphosis per level of osteotomy dependent on the spinal level being osteotomized. For large, angular deformities, a three-column osteotomy allows for greater correction in the coronal and sagittal planes.
We perform VCR in place of anterior and posterior procedures, electing to perform the correction through one single approach.
The VCR is almost invariably performed at the apex of the deformity.
Preoperative Planning
A multidisciplinary team approach is often necessary in the treatment of patients with complex deformity that requires a VCR.
Preoperative assessment of the patient’s cardiovascular, pulmonary, nutritional, hematologic, and metabolic systems is required to maximize the patient’s preoperative reserve.
Careful examination of the preoperative CT scan should alert the surgeon to areas of bony deficiency in the posterior elements to prevent incidental durotomies (see FIG 2C,D).
Positioning
The patient is positioned prone on an OSI Jackson frame with six pads, which are placed strategically to allow the abdomen to rest free, reducing intra-abdominal pressure and intraoperative bleeding.
We prefer to place a halo or Gardner-Wells tongs with 5 to 15 pounds of traction that allows for rigid positioning of the skull with the face free.
The arms are placed in a 90-90 position with care to position the axillae free and elbows well padded to decrease the risk of brachial plexopathy or ulnar nerve neuropathy.
Pressure areas are carefully padded as the length of the procedure increases the risk of position-related complications (eg, skin macerations, plexopathies).
The hips are gently extended and the knees slightly flexed with the use of multiple pillows.
Spinal cord monitoring leads are placed to monitor the sensory and motor function of the lower extremities.