and François Moutet2
(1)
Marseille, France
(2)
Grenoble, France
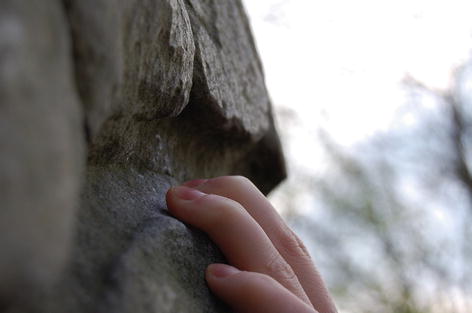
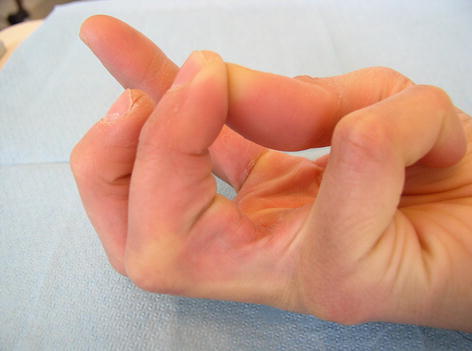
Photo 3.1
Slope grip
3.1 Tendon Injuries
3.1.1 Tendinopathy
3.1.1.1 Tendinitis
Introduction
Tendinitis is an inflammation of a tendon and its sheath. The clinical symptoms involve a pain, a specific or diffuse swelling, and a difficulty in the movement.
The tendon looks like a rope and is made of smooth and resisting fibers. So just like a rope, the tendon is subject to several changes starting from simple fraying to eventually the final rupture. Repeated movements, intensive efforts, a bad posture or a long-term identical position, vibrations, and a physical stress are a few examples of what may lead to an alteration in the tendon. Any change in the tendon results in an inflammatory reaction, that is to say, a local reaction in the tissue after a lesion. Throughout time, inflamed tendons become irregular, getting thicker and battered. In order to get back to normal and to avoid chronic fragility of the tendon, a break is highly advised.
The three following signs reveal the weakness of a tendon:
Firstly, the pain blurs away during the warm-up.
Secondly, the pain is more persisting.
Thirdly, the pain is omnipresent even during rest periods.
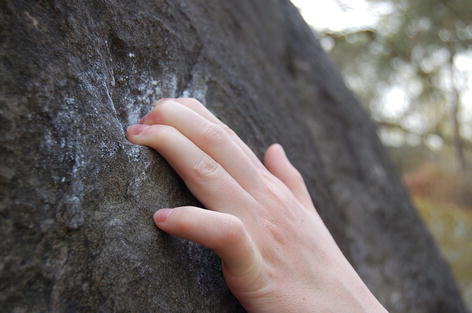
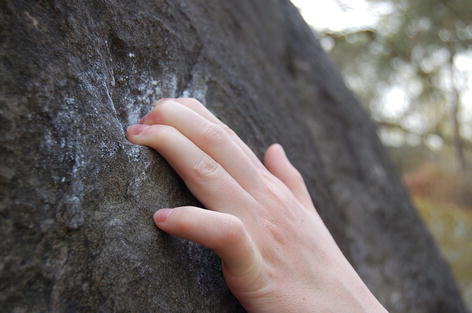
Photo 3.2
Three-finger grip open hand posture
Tendinitis Factors
Several causes are responsible for tendinitis. People don’t react the same way according to the intensity or effort required in climbing; this is why training has to be personalized. Tendinitis appears after a too much repeated or exaggerated work. Bearing that in mind, avoiding injuries is consequently possible as long as training main principles are respected (cf. part Training and Back to Training).
To start well, a training practice has to begin with a general warm-up before focusing on precise muscles. The intensity may vary according to the climber’s capacities, but the most important is to adjust the practice to the present physical condition and level of the climber. To finish, it’s a priority to stretch the muscles – get back to a relaxed posture before any effort – to reduce the tension.
What really matters is to listen to one’s body and learn how to deal with the body signs telling people to emphasize, maintain, or reduce the intensity of any effort. In case of a persisting pain after the warming-up, it’s a priority to stop the ongoing practice and consult a doctor.
In climbing, several factors may account for tendon traumas:
An overexaggerated repetition of the same movement
Holds with stiff edges
Too small holds preventing a precise grip or the use of all fingers
Crimp grip
A bad posture in climbing up
Finger reception during a grip after a dynamic movement or a dyno which is quite traumatizing for the tendon in contact with the hold
But one of the main causes of tendinitis is dehydration, which damages the resilience of the tendon tissue (cf. part Assessment and Safety). The lack of water is very common; this is why the climber has to learn how to drink before, during, and after the effort.
Another cause of tendinitis is a too high-protein diet. Indeed, proteins tend to enhance the volume of urea and uric acid which are extremely toxic for the tendons. High-protein diets may also cause muscular hypertrophy which might damage the tendon that has not undergone the same changes and still remains less resilient and less strong.
A chronic dental infection is also another factor for tendinitis, since tendons are extremely sensitive to that phenomenon. Consequently, a good dental hygiene and a regular dental checkup are a good way to avoid tendinitis not resulting from a usual practice.
So it is important to bear in mind that a bad dental hygiene may lead to a slight moderate infection, which might be nonetheless quite toxic for tendons.
Localizations
The feeling of a pain on the injured part of the body is the clinical sign of tendinitis problems.
In climbing, a hand tendinitis is most of the time located on finger flexor tendons, but muscle flexor tendons may also be injured. The finger superficial flexor is the most frequently wounded part. The pain is then located in the P2 and P1 phalanges area – due to the constant strain resulting from the crimp grip posture – more particularly in the middle and the ring finger.
Clinical Data
Typical physical signs of a tendinitis can be revealed after a medical exam:
A painful feeling on the injured part
A possible swelling
A red blotch on the wounded area
A reduced mobility
Of course, all these symptoms may not appear at the same time, but one of them can be the sign of a tendon lesion.
According to the seriousness of the tendinitis, the pain is first felt before the warming-up and gradually disappears as the warming-up starts, squeezing a ball in one’s hand for instance.
The clinical exam has to be bilateral and comparative to detect surely and precisely the location and the gravity of the lesion. The former one includes several steps: checkup, contraction against resistance, passive stretching, and palpation.
The checkup is just a way to get superficial details about the tendons, such as the volume, the outline of the soft lateral parts, and the muscle’s general condition.
Contrary to the checkup, the contraction against resistance exam is a fundamental key of the clinical tests. Indeed, as regards tendinitis and to confirm a proper diagnosis, it is a priority to find out if pain is felt after contraction against resistance.
The second most important exam is the passive stretching, which sometimes may be painful or with a small limitation in the amplitude of the movement. Those exams can be easily performed as long as the people concerned have a small knowledge in anatomy and physiology.
As regards the palpation exam, it has to be meticulously done, since it is a means to detect different anomalies such as:
A spontaneous pain felt by the patient
A locally increase in temperature
Localized or spread friction
A painful moderated or voluminous nodule
Most of the time, the pain is gradual, but it can be quite sudden in some areas. In fact, a direct shock, just like a usual physical activity or training, sometimes more intense or totally new, may cause, aggravate, or start up the pain again. A change in the training habits, in the technique, or in the equipment used may also trigger new pains.
Treatment and Behavior
After a painful feeling in one part of the hand, obviously, the wisest solution is to stop the practice. The most efficient and immediate treatment is to stop any activity and to put some ice or use any other cryogenic method – the use of very low temperatures. The complete stop of any practice implies the obligation not to use the inflamed limb. It is highly advised not to grip any objects with the injured finger. Pain killers can be prescribed by doctors to ease the pain.
Several icing techniques are available. One of them consists of, first, applying ice on the lesion for 10 min, then waiting for 20 min to let the blood circulate and drain the injured part, and finally icing again for ten more minutes. This operation needs to be repeated three times a day for 3 days. Cryogenics is very efficient in inflammation cases, and the topic will be thoroughly dealt with in the Chap. 6.
According to the seriousness of the lesion, several additional creams can be used to ease the pain. Nonsteroidal anti-inflammatory creams (NSAI) such as Ketum®, Nifluril®, or Voltarene® are quite efficient once locally applied. But to cure the most serious cases, cryogenics, electrotherapy (treatment using the electric current), and mesotherapy (locally simultaneous injections of anti-inflammatory drugs) are necessary. According to the injections, infiltrations can soothe the pain (pain-killer effect) or fight against inflammation (anti-inflammatory effect).
Therefore, no strain has to be undergone by the injured limb which is not healed yet even if the pain has been killed, that is why infiltrations are not recommended for finger lesions.
Other means are available to help tendon healing. The deep transverse massage (DTP) is a to-and-fro motion which “irritates” the tendon and consequently improves vascularization. This massage consists of making small movements transversally to the tendon or on the edge of the tendon-bone insertion. After a while, if the strain is tolerated, the pressure will be enhanced, and instead of using the finger pulp, the edge of the flexed index medium joint will be used.


Photo 3.3
Transverse massage
A tendon is part and parcel of a chain reaction, which can be slightly disturbed by a dysfunction in the vertebra, back muscle, or anything else. Any small change in the tendon axis can lead to torsion and consequently to rubbing of the tendon in its sheath. Therefore, in case of serious fall in lead category, when a climber has been “spot” by a bilayer, or in bouldering, a fall on the back, the coccyx, or outside the crash pads, it is highly recommended to consult a specialist to check the integral rachidian system of the different muscular chains, in order to detect any even harmless lesions connected to climbing risks. Therefore, a potential fall at high-level climbing has to be considered, because it can have harmful side effects on other parts of the body.
After a tendinitis, full sports practice has to be interrupted for 2 weeks; nonetheless, it is highly recommended not to go back to training as long as the pain persists.
Medical Scanning
X-rays are not really helpful as regards tendon injuries contrary to MRI and scanning which are more relevant to give a proper diagnosis.
Schema 3.1
Tenosynovitis ultrasonography
3.1.1.2 Tenosynovitis
Introduction
Tenosynovitis is an inflammation of the synovial sheath surrounding the tendons. The function of this sheath is to ease the sliding of the tendon especially during a change of direction. An oily liquid – synovia – is secreted by the walls of the synovial sheath. Some factors such as microtraumas due to constant rubbing or repeated shocks can lead to a dysfunction in the lubrication system. An inflammation and a swelling of the synovial sheath can result from the constant rubbing between the tendon and the synovial sheath. When the normal sliding is hampered, a pain and a “crepitus” – friction – are felt while in action.
This injury is often quite sudden and has to be treated immediately in order to avoid the weakness of the tendon, its adhesion to the synovial sheath, or any other more harmful problems.
Tenosynovitis Factors
Joint strain is often one of the causes of tenosynovitis especially when a move is currently repeated leading to microtraumas. This tendon lesion happens when tendons are overstrained during an effort highly above one’s capacities in order to go over one’s limits.
Safety precautions about tendinitis have also to be taken to avoid tenosynovitis.
Localization
A tenosynovitis usually affects the finger flexor muscles, but it may also affect the extensors, though that lesion is much less common. The pain results from a long and intense rubbing especially during the crimp grip and is generally felt in the area of the P1 phalange. The pain may eventually spread over the palm up to the forearm.
Clinical Data
When a pain is suddenly felt in the area of the P1 phalange, a precise diagnosis has to be made to find the appropriate treatment and not to take this injury as a rupture of the pulley.
Treatment and Behavior
The first thing to do is to get treated, and the second step to take is stopping climbing practice. The finger needs some rest and has to be joined to the next finger. It is advised to ice the injured finger several times a day (cf. Chap. 6).
It is also highly suggested to see a hand specialist or a sports doctor who will prescribe the right treatment. As regards tenosynovitis, one has to bear in mind that infiltrations are to be avoided.
After a tenosynovitis, full sport practice has to be interrupted for 2 weeks; nonetheless, it is highly recommended not to go back to training as long as the pain persists.
Medical Scanning
Schema 3.2
Tenosynovitis ultrasonography. FDS flexor digitorum superficialis, FDP flexor digitorum profundus, P1 proximal phalanx
Tendinopathy Recap
Symptoms
A painful feeling in the lesion area
A possible swelling or red blotch
A sudden sore
Treatment
Icing three times a day
Anti-inflammatory gels prescribed by doctors
Rest Period
About 2 weeks up to 6 weeks
Behavior
Immediate stop in climbing practice
No more practice as long as the pain is still felt
See a doctor
3.1.2 Synovial Cyst
3.1.2.1 Introduction
A cyst is an abnormal swelling filled with liquid matter and most of the time connecting to a precise joint. In climbing, as far as fingers are concerned, the tendon sheath synovial liquid can prevent finger flexion and consequently hamper hold gripping.


Photo 3.4
Synovial cyst (into the digital sheath) at proximal index level
3.1.2.2 Synovial Cyst Factors
The excessive use of a joint is one of the main factors of synovial cysts. The sheath inflammation may cause a nodule to occur.
3.1.2.3 Clinical Data
It is a swelling on the flexor tendon located at the basis of the finger. This swelling may be painful when touched or when involved in a movement.
As time goes by, the swelling may grow bigger and is perfectly recognized with its well-limited outline and the elasticity and the hardness of the cyst.
3.1.2.4 Treatment and Behavior
A treatment is not always necessary for the sportsman because this cyst may change and eventually disappear spontaneously. A period of rest may help, and surgery may be involved in case of long-term troubles. Other side treatments such as punctures are hardly used due to the inevitability of a recurrence. In surgery, the swelling and its basis are entirely retrieved. And usually, the results imply no problems of stiffness, even if a recurrence is always possible.
3.1.2.5 Medical Scanning
Schema 3.3
MRI: synovial cyst
3.2 Pulley Injuries
3.2.1 Introduction
In climbing, the intensive training has led to the appearance of new lesions such as pulley rupture – with or without bow stringing.
This trauma is one of the most feared by climbers since it implies a complete stop in climbing practice. Besides, very few preceding signs can be detected. And most of the time, this microtrauma affects high-level climbers. Surgery is not systematic; nonetheless, when it has to be done, 80 % of climbers go back to normal – sometimes they even achieve higher capacities.
Schema 3.4
Bow stringing effect (Illustration inspired by Chevrot (A.), Clinical Imaging wrist and hand,1998 Masson)
3.2.2 Pulley Rupture Factors
Most of the time, this kind of lesion occurs during intensive training in CG, especially during a repeated work on a difficult route. Having great expectations, the majority of top climbers keep practicing, repeating on and on the same movements, and consequently straining or putting pressure on a finger or a pulley. Besides this, pressure is enhanced by a limited time to get rest between each attempt, reinforcing the strain and the weight undergone by the same finger structure. So the numerous tries before going through a difficult route successfully are responsible for localized pulley lesions. The breaking of the pulley usually happens in crimp grip during a dyno or a repeated difficult route.
In crimp grip posture, the finger joint is easily torn off. The climber’s weight and the number of fingers used are factors which make the tearing complete. Whatever the cases, all the pulley breaking follows the same pattern; the PIP is suddenly and violently extended when the fingers are flexed in the PIP area.
Particular training sessions on hangboard or campus board are also quite straining for the pulleys and are the cause of lesions. During these trainings, the grip depends only on the finger strength and the climber can’t use his legs to get “some relief.” The body movements from one grip to another, especially in dynamic actions, cause violent shocks on the pulleys.
The lack of warming-up and an inappropriate hydration indirectly lead to lesions.
3.2.3 Clinical Data
The third- and fourth-finger pulley A2 and A3 seem to be the most affected by this trauma. Indeed, these pulleys are constantly used in rock climbing, especially in grips with one-finger pocket or two-finger pocket, when flexors are overused. But only the pulley tends to be injured, whereas the tendon flexor remains intact.
The symptom is always the same, a vivid sore with an audible cracking. Surgery is decided only if a bow string is visible during a crimp grip.
The other signs of this lesion are the following:
A pain on the pulley during palpation
A soreness when flexing/resisting P2 over P1
A located edema
An incapacity in mobility and the presence of a bow string according to the seriousness of the injury
3.2.4 Treatment and Behavior
The climber has to stop immediately any practice to prevent any worsening of the injured pulley or the other ones. Then icing has to be done three times a day until the hand specialist’s visit. Meanwhile, the sportsman can also bandage his finger joining it to the next one – finger knitting. In any case, no strain has to be endured by the injured finger.
If there’s no bow stringing, the preventive treatment is essentially based on a thermally molded protective ring. Physiotherapy and ultrasounds may complete the treatment. The rigid protective ring has to be maintained for about 45 days, and of course a complete cessation of activity is the key to accelerate the healing process. No weight loading has to be undergone. This latter behavior is probably the most difficult to accept by top competitors.
The hand specialist has to detect the presence of a bow string – bilaterally and in crimp grip. The test is positive when the doctor feels the flexor sticking out under the skin as he is auscultating the patient. When in doubt, the diagnosis will be more precise with a scanning or an MRI.