Chapter 6 Use of Fresh Osteochondral Allograft for Chondral and Osteochondral Defects in the Knee
Introduction
Increasing demand for allografts has been met with advancements in tissue procurement and increased availability of fresh donor tissue from commercial entities as opposed to university-based specialized transplantation centers, which in the past had limited availability to orthopedists in the community.1–3
The advantage of fresh osteochondral allografting is the transplantation of mature hyaline cartilage with viable chondrocytes,4 which survive hypothermic storage and transplantation while maintaining their metabolic activity and sustaining the surrounding collagen matrix.5 Investigations have focused on extending the storage interval of fresh human osteochondral allograft tissue. Ball et al6 compared the effects of different storage media on human osteochondral allograft tissue when stored hypothermically in either lactated Ringer’s solution or a standard culture media containing amino acids, glucose, and inorganic salts. The standard culture media demonstrated superior storage properties as measured by chondrocyte density, viability, and metabolic activity. Biomechanical properties of the matrix remained relatively intact in both media. Chondrocyte viability essentially remained unchanged from baseline for as many as 14 days in the standard media, at which time viability was 90.5% in standard media versus 80% in lactated Ringer’s solution.
Graft procurement and storage
Recovery, processing, and testing of donor tissue follow guidelines established by the American Association of Tissue Banks (AATB)7,8 and is under the authority of the U.S. Food and Drug Administration (FDA).9 Most tissue banks have a 24-hour time limit for retrieval of tissue from refrigerated cadaveric donors in a sterile operating room environment following strict sterile technique. Donors between the ages of 15 and 40 years are generally considered for inclusion in the donor pool if their articular surfaces pass direct inspection for cartilage quality.
It is the policy of tissue banks to hold transplants for a minimum of 14 days to allow completion of microbiologic and serologic testing prior to release. Hence the actual surgical implantation is delayed by 3 and to 6 weeks after procurement compared to university center clinical practice of implanting allografts usually within 1 week of harvest. Although results using this traditional fresh tissue protocol have been good even in mid-term follow-up,10 the effects of prolonged allograft storage on clinical outcomes have not yet been determined.
Use of fresh-frozen grafts improves graft availability, reduces immunogenicity, and may be appropriate for bulk allografting in major osseous reconstruction as encountered in musculoskeletal tumor cases. However, deep freezing of chondrocytes within their extracellular matrix (usually at −80° C) practically eliminates all viable chondrocytes in the articular cartilage portion of osteochondral grafts. Furthermore, clinical experience indicates that the articular matrix in frozen allografts deteriorates over time, presumably because insufficient surviving cells are present within the matrix to maintain tissue equilibrium.11,12 However, retrieval studies have demonstrated that with fresh, cold-stored osteochondral allografts, viable chondrocytes are present and mechanical properties of the matrix are maintained many years after transplantation.13,14
Safety and risk of disease transmission
Osteochondral allografts are aseptically procured, which reduces but does not eliminate the risk of graft contamination during recovery via postmortem invasion by gastrointestinal flora or occult infection in the donor. Any transplantation of allogeneic organs or tissue is associated with a residual risk of transmission of infectious disease, despite donor screening and testing, and rare allograft-associated bacterial infections have been reported. Advances in serologic testing for human immunodeficiency virus, hepatitis, and other diseases have improved safety, but a measurable risk does remain. The surgeon and the patient should be well aware of the possibility of risk for transmission of serious diseases when fresh allograft tissue is used, making the discussion of the risk of bacterial or viral disease transmission part of the informed consent.15
Immunology
Small-fragment allografts are not human leukocyte antigen (HLA) or blood-type matched between the donor and recipient. Although hyaline cartilage appears to be relatively immunoprivileged,16 fresh unmatched osteochondral allografts elicited a variable immune response in one study of fresh osteochondral allografts, and 50% of individuals generated serum anti-HLA antibodies.17 The presence of anti-HLA antibodies correlated with an inferior appearance of the graft–host interface on magnetic resonance imaging (MRI) studies. Poor MRI incorporation also has been correlated with inferior clinical results10 and may be a result of immunologic mechanisms. The issue of immune behavior ultimately may become clinically relevant, and it is clearly an area where more knowledge is necessary in order to improve outcomes of the use of fresh osteochondral allografts.
Indications
Specific conditions that are most amenable to allografting in clinical practice include osteochondritis dissecans,18 osteonecrosis,19,20 and posttraumatic defects, such as those occurring after periarticular fractures about the knee.21 A particularly troublesome condition to manage is posttraumatic tibial plateau fracture, which is especially suitable to management by fresh osteochondral allograft.22 Allografts have also proved valuable for the salvage of knees for which other cartilage resurfacing procedures, such as microfracture, autologous chondrocyte implantation (ACI), and transfer of autologous osteochondral plugs.
Common to all allografting procedures is matching donor with recipient on the basis of size.23 In the knee, an anteroposterior radiograph with a standardized magnification marker is used, and the mediolateral dimension of the tibia, just below and parallel to the joint surface, is measured. The measurement is accurately adjusted for magnification, and the tissue bank makes a direct measurement on the donor tibial plateau. Alternatively, a measurement of the affected condyle can be performed. A match is considered acceptable within 2 mm.
Surgical techniques
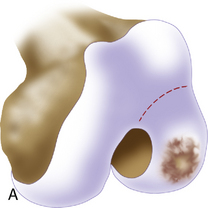
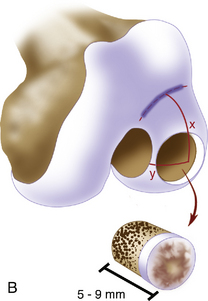
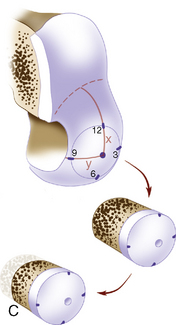
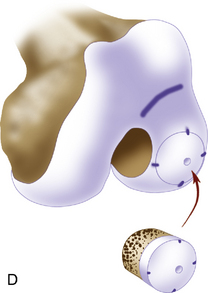
Surgical transplantation of a fresh osteochondral allograft requires a medial or lateral arthrotomy. Occasional meniscal takedown for very posterior lesions with possible patellar eversion may be necessary. The lesion then is inspected and palpated with a probe to determine its extent, margins, and maximum size. Two techniques commonly used for preparation and implantation of osteochondral allografts are the press-fit plug (dowel) technique (Figure 6–1) and the shell graft technique (Figure 6–2). Each technique has advantages and disadvantages. The press-fit plug technique is similar in principle to autologous osteochondral transfer systems. It is optimal for contained condylar lesions between 15 and 35 mm in diameter. Fixation is generally not required because of the stability achieved with the press fit. Disadvantages include the fact that many lesions, such as very posterior femoral, tibial, patellar, and trochlear lesions, are not accessible to a circular coring system. In addition, the more ovoid the lesion, the more normal cartilage must be sacrificed at the recipient site in order to accommodate a circular donor plug. Shell grafts are technically more difficult to perform and typically require fixation. However, depending on the technique used, less normal cartilage may need to be sacrificed. Also, certain lesions are more amenable to shell allografts because of their location.