Fig. 15.1
A 19-year-old collegiate volleyball player with right elbow pain for 5 months. He attempted two courses of 4 weeks of rest with return of symptoms before diagnosis of distal humeral stress fracture. (a) Unremarkable anteroposterior (AP) radiograph of the right elbow. (b) Unremarkable lateral radiograph of the right elbow. (c) Coronal STIR image demonstrating increased edema within the distal humeral diaphysis indicative a stress reaction
Treatment
The treatment for spiral stress fracture of the humerus is primarily nonsurgical, with very few reports of open reduction and internal fixation performed. There have been two cases reported of ORIF, one due to displacement of the fracture [7] and the other due to failure to maintain closed reduction [4]. Conservative treatment consists of a minimum 4 weeks’ absence from aggravating activity with [2, 4, 6] or without immobilization [5, 14–16], and gradual resumption of activity over the next 4 weeks [18]. If immobilization is chosen, this can be achieved with a cuff and collar for 1 week with subsequent transition into a humeral fracture brace for 3 weeks [6, 19].
Prognosis
Patients treated for spiral stress fracture of the humerus have returned to play in as little as 3 weeks, but more typically take 8–12 weeks [5, 6, 14]. Even after delayed union, athletes are eventually able to return to sport though it can take up to 9 months [16]. Prevention of recurrence is important, and mitigating poor mechanics and enhanced strength training are both important factors. For throwing athletes returning from stress fractures, a good throwing program should be initiated beginning 3 months before the start of preseason training. For tennis players, athletes should work closely with coaches and analyze their mechanics diligently. They should specifically look at knee flexion and rotation of the trunk and upper limbs during the preparation phase of service and forehand strokes. The most common finding is poor leg drive motion during the preparation phase of each stroke [14]. Recognition of this flaw and adequate coaching to change the mechanics can lead to a presumed mitigation of the risk for recurrence by lessening the stress on the upper body while still maintaining adequate power [13, 14].
Transverse Stress Fractures
Mechanism
Transverse stress fractures of the humerus occur in the proximal and middle portions of the humerus and are rare, with very few case reports existing in the literature. Transverse stress fractures of the humerus are common in weight lifting with the injury being reported in a body builder [20] and in a competitive weight lifter [21]. Flat bench press seems to exacerbate the symptoms with the most pain being felt during this exercise. During the bench press exercise, the humerus effectively proceeds through an arc of shoulder extension, followed by shoulder flexion—with virtually no rotation of the humerus. Thus the rotational actions of the pectoralis major muscle must be countered by the other muscles of the shoulder girdle, including the deltoid and rotator cuff muscles [22]. The muscular tissues are able to dynamically redistribute the forces across the supporting skeleton, allowing the bone to effectively endure more load or stress, a phenomenon known as stress shielding [21]. A transverse stress fracture can occur with increased bending load across the bone, which is often the sequela of muscle fatigue that leads to the compromise of stress shielding [21, 22].
Presentation
In the reported cases, presentation involved significant pain localized to the proximal, anterior aspect of the affected arm, occurring during bench press and persisting for hours after the exercise. These symptoms were present for at least 4–6 weeks prior to diagnosis [20, 22]. Each patient tried a period of rest from bench press and other aggravating activities such as incline press, pectoral fly, biceps, and overhead exercises [20, 21]. Inevitably after the period of rest in which the pain subsided, ranging 1–6 weeks, a flare of the same pain occurred on their return to flat bench or other previously mentioned activities. One weight lifter progressed to a complete fracture and experienced an audible snap, with his arm giving way, on the second set of his normal weight lifting routine [22]. All of the patients denied the use of anabolic steroids.
Diagnosis
In most cases, the physical examination revealed tenderness to palpation in the region between the bony insertions of pectoralis major and anterior deltoid [20, 21]. There can be mild pain on manual resistance of shoulder movements, especially internal rotation and abduction [20]. Strength and range of motion of the shoulder and elbow usually does not show any deficits. Plain radiographs can show a transversely oriented radiolucency with surrounding periosteal reaction and sclerosis. Bone scans can confirm the diagnosis of stress fracture by showing abnormal focal increased uptake in the cortex of the affected mid-humerus.
Treatment
A period of 6–8 weeks free from all weight lifting activities involving the upper extremities, followed by gradual resumption of training is usually the first course of treatment for a transverse humeral stress fracture [20, 21]. If displacement or complete fracture has occurred, ORIF can be performed. Usually no bracing or immobilization is necessary.
Prognosis
These fractures typically respond quite favorably to a period of rest and a return to previous levels of competition can be expected once the fracture is completely healed, usually by 4 months. Progressing to full activities too quickly can lead to minor relapses in symptoms [20, 21]. If surgery is performed, return to sport can be unpredictable.
Olecranon
Four types of olecranon stress fractures have been reported in the literature. Two types tend to occur in skeletally mature athletes, and include fractures of the olecranon tip and oblique fractures through the midportion of the olecranon [23, 24]. The other two types tend to occur in skeletally immature athletes, and include transverse fractures, and osteochondroses [25, 26].
Presentation
These fractures present with dull aching and localized tenderness around the olecranon, worsened with activity, usually without recall of an acute injury [27, 28]. Symptoms evolve over a variable time frame which can be anywhere from a few weeks up to a year. These injuries are common in throwing athletes who will describe posteromedial elbow pain during the acceleration and follow-through phases of throwing [23, 24]. Very few athletes report pain at rest or while performing daily activities [29]. Clinically, tip fractures are more likely to present with a painful elbow after a particularly strong throw, whereas other stress fractures in the olecranon are more likely to present with a longer history of pain that lessens with rest and recurs when they resume throwing [28].
Diagnosis
Physical examination often reveals decreased arc of motion at the elbow, with flexion contractures that are common in the throwing population often present [30–33]. There is marked tenderness to palpation along the posteromedial aspect of the olecranon. In certain cases a milking maneuver may be positive, which could indicate a concomitant MCL injury [30]. The diagnostic modalities for each are similar, with plain radiographs often missing the diagnosis of stress fracture early in the process. Thus for the most accurate diagnosis to be made, bone scan or MRI must be considered [24, 27, 29]. The mechanisms, specific imaging findings, treatment, and prognosis will be discussed separately for each stress fracture in the remainder of this section.
Proximal-Third (Tip) Fractures
Mechanism
Olecranon tip fractures involve the proximal third of the olecranon and are classically described in javelin throwers [24], but have also been described in baseball pitchers [28, 30, 34] and gymnasts [26, 27, 35]. There is a component of repetitive abutment of the olecranon into the olecranon fossa causing osseous hypertrophy that is combined with traction from triceps activity during the deceleration phase of throwing [23, 24, 32, 33]. Olecranon tip fractures can occur more acutely than other olecranon stress fractures and as such are often diagnosed in the acute phase of injury [28].
Diagnosis
Plain radiographs can routinely confirm the diagnosis of an olecranon tip fracture [28]. Plain radiographs may show either the fracture itself, or the conditions that predispose to it, those being an increase in cortical thickness of the humerus (which produces a corresponding decrease in the available space within the olecranon fossa) and cubitus valgus (which exacerbates the potential impingement between the olecranon and the narrowed fossa) [33]. If plain radiographs are negative, they should be followed by a bone scan or MRI to make the most accurate diagnosis [24, 29].
Treatment
Fractures of the olecranon tip are prone to delayed unions, nonunions, or the formation of loose bodies. As such these fractures are frequently treated by surgical methods, including open reduction and internal fixation or tip excision [23, 34], though satisfactory results have been attained with rest and immobilization as well [23, 28]. Excision of loose bodies can lead to faster return to play for athletes [34].
Prognosis
Operative intervention can often lead to a faster return to play. Hulkko et al. compared return to play after both conservative and operative treatment. Both athletes returned to play with optimal healing; however the conservatively treated athlete returned after 18 months, and the operatively treated athlete returned after 2 months [23]. Six months is a reasonable expectation for return to play with conservative treatment. Earlier surgical intervention offers the possibility of earlier return to play, as well as a decreased risk of delayed unions, nonunions, and formation of loose bodies [35].
Middle-Third (Oblique) Fractures
Mechanism
Oblique stress fractures of the olecranon usually result from impaction of the medial olecranon on the medial wall of the olecranon fossa during valgus extension forces, which happens commonly during the acceleration phase of throwing [24, 33]. At the same time, the lateral aspect of the coronoid impinges against the intercondylar notch [30]. These two points of impingement provide the necessary stress to produce an oblique stress fracture. Oblique fractures of the olecranon have been classically described in baseball pitchers [24, 29, 30, 34] and javelin throwers [23].
Diagnosis
Physical examination reveals tenderness to palpation over the posteromedial elbow, and pain is reproduced on valgus stress testing, or forced hyperextension of the elbow. Extension lag in the affected extremity is also common [24, 30]. Plain radiographs are often negative or show subtle findings of periosteal reaction over the medial olecranon. In the setting of an acute stress reaction, MRI shows poorly defined, patchy areas of low signal intensity in the proximal posteromedial olecranon on T1-weighted images and areas of high signal intensity in the posteromedial olecranon on T2-weighted images, consistent with bone edema and hyperemia. In the setting of a more discrete, incomplete stress fracture, MRI shows more focal linear areas of intermediate signal throughout the cortex and subjacent cancellous bone of the articular surface [29] (Fig. 15.2).
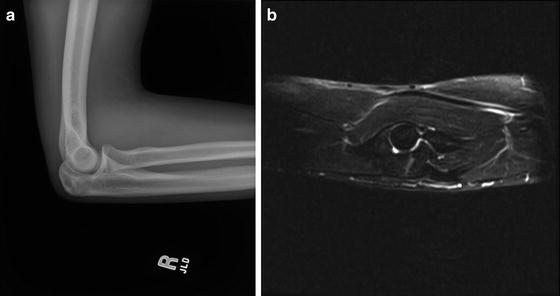
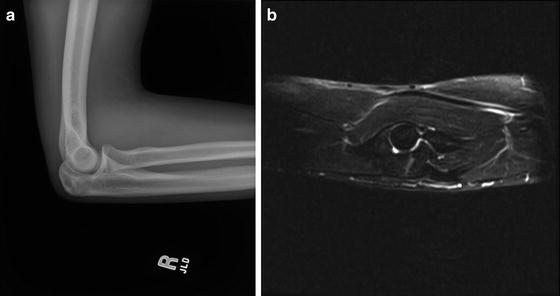
Fig. 15.2
A 15-year-old baseball pitcher with 2-month history of elbow pain. (a) Lateral radiograph of the right elbow demonstrating linear bone sclerosis at the olecranon. (b) T2 sagittal MRI image demonstrating transverse stress fracture of the olecranon
Treatment
Treatment involves a period of rest and avoidance of valgus stress (especially throwing) for at least 6 weeks, with some authors recommending restriction from sports for up to 6 months [24]. Some authors also advocate for an orthosis to limit full extension in the initial 4 weeks, as well as an interval-throwing program at 8 weeks before allowing return to play at about 12–14 weeks [29]. Though most respond to conservative management, occasionally operative management is required if there is no clinical or radiographic improvement [29, 30]. The recommendation for operative treatment of the oblique stress fracture pattern of the olecranon is using a tension-band type construct though other constructs have been shown to be effective [44].
Prognosis
Conservative treatment usually offers satisfactory results with a short period of rest and partial immobilization followed by gradual increased range of motion and rehabilitation. Schickendantz et al. showed professional baseball players managed conservatively returned to play at an average of 12–14 weeks and remained active in their sport in follow-up ranging from 2 to 7 years [29]. There have been reports of delayed surgical intervention in patients who showed a lack of healing after a 6 week course of conservative therapy. These patients were treated with a single screw and iliac bone pegs and were able to return to full activities within 4–6 months [30].
In summary, conservative therapy is the first-line treatment option and usually allows athletes return to play by 3 months [29]. Surgical intervention is reserved for the setting of failed conservative management.
Physeal (Transverse) Fractures and Osteochondroses
Mechanism: Transverse Fractures
Transverse fractures occur in skeletally immature patients and are caused by an overload of extension forces at the physis which is the weakest area of the olecranon [24, 32]. This typically results from traction and shearing forces on the olecranon acting at two sites: the insertion of the triceps tendon into the olecranon and the olecranon physis itself [26].
Mechanism: Osteochondroses
When the olecranon epiphysis is not fully ossified, traction forces may cause disturbance of blood flow and result in localized areas of avascular necrosis with disturbed ossification and fragmentation—better known as traction apophysitis or olecranon osteochondritis [32]. When the epiphysis is more mature (but not yet fused), these same traction forces can produce a Salter Harris type I stress fracture through the growth plate [26, 36, 37].
Presentation and Diagnosis
These injuries have been reported in young gymnasts [25–27, 38], adolescent baseball pitchers [25, 39, 40], wrestlers [41], and competitive adolescent divers [42, 43]. The stress fracture usually manifests as either a traction apophysitis with a more gradual onset or an avulsion of the physis which presents more suddenly. Physical examination can reveal an extension lag at the elbow that may worsen with continuation of the offending activity [41]. Plain radiographs can be normal in the setting of early disease, and a high degree of suspicion should be maintained in the adolescent athlete. Comparison radiographs of the contralateral elbow can be helpful. Radiographs later in the process reveal a widened physis, often with fragmentation of the olecranon apophysis [25, 38, 41]. A confirmatory sign is the presence of an irregular band of ossification within the growth plate, which results from disordered mineralization [38]. In the setting of negative radiographs, the use of bone scan or MRI can confirm the diagnosis [24, 27] (Fig. 15.3).
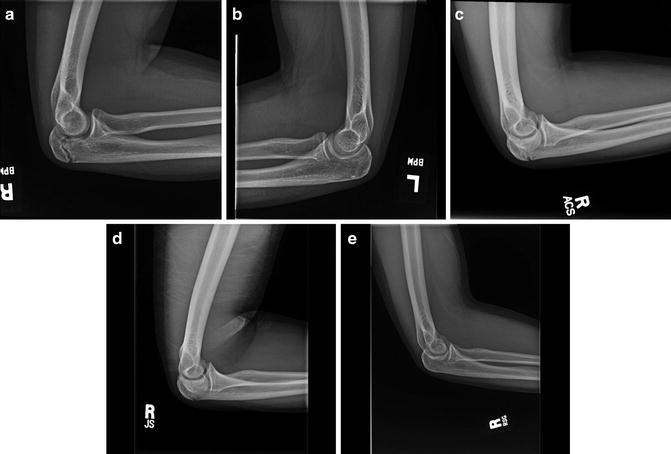
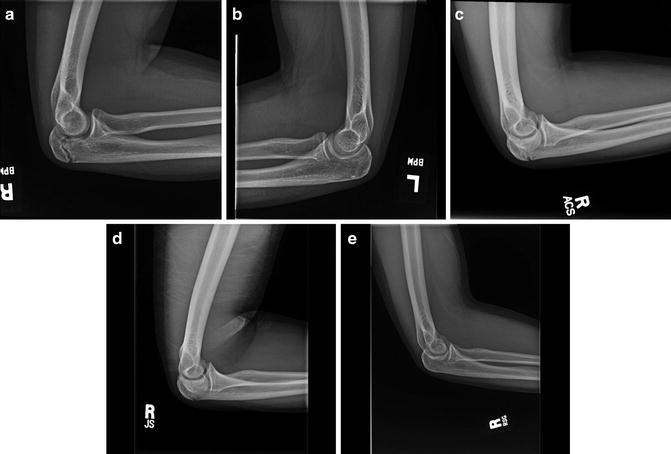
Fig. 15.3
A 14-year-old baseball pitcher with 2 months of right elbow pain. (a) Lateral radiograph of the right elbow showing widened, irregular olecranon apophysis. Notice the difference when compared to the contralateral elbow (b). A period of complete rest was initiated. (b) Lateral radiograph of the left elbow obtained at the same time as (a) showing fused olecranon physis. (c) Lateral radiograph of the right elbow obtained after a 2-month period of complete rest. Notice the progressive closure of the apophysis. (d) Lateral radiograph of the right elbow taken after 3 months of complete rest demonstrating continued closure of the olecranon apophysis. (e) Lateral radiograph of the right elbow at final follow-up 8 months after presentation showing complete closure of the apophysis. The athlete began a throwing program after a 3-month period of rest from initial presentation
Treatment
Once the diagnosis is made, nonoperative treatment consisting of rest and avoidance of aggravating activities should be initiated immediately. In patients not responding to this therapy or who wish to return to competitive activities more quickly, surgical intervention can be discussed [40]. If a nonunion develops, the treatment involves open reduction and internal fixation with bone grafting of the growth plate to promote fusion [36]. The options for fixation technique for the transverse stress fracture pattern of the olecranon include screw compression [23, 36, 39, 40] or tension band fixation with Kirschner wires [27, 40, 41]. The use of screw fixation is preferable, and has been shown to be more stable than tension band-only constructs [44]. Screw fixation also minimizes the potential need for hardware removal which can be common with tension band constructs [39, 45, 46].
Prognosis
Though conservative treatment of transverse fractures to the olecranon is recommended, it carries the inherent risk of nonunion [26, 27, 41]. Conservative management consists of rest with or without immobilization and usually returns the athlete to sport by 6 months. Surgical intervention is necessary in the setting of a nonunion, or can be considered if the athlete desires a speedier return to activity. Though no studies to date have confirmed a more rapid return to play with early surgical intervention, convention dictates it to be true [40].
Ulna
Mechanism
Stress fractures of the ulna have been reported in a variety of athletes, including tennis players [47–51], baseball and softball pitchers [52–55], weight lifters [56–58], a body builder [59], riflemen [60], a volleyball player [54], a baton twirler [61], a cheerleader [62], an honor guard participant [63], a bowler [64], a golfer [65], a polo player [66], and a kendo player [67]. Though there are reports of stress fractures occurring proximally [52, 54, 64], distally [47, 50, 65], and even in the ulnar styloid [67], the middle one-third of the ulna has the smallest cross-sectional area as well as the most triangular (least circular) shape, making it the least resistant to torsional stress. The majority of cases described involve the middle one-third of the shaft [48, 49, 51, 53, 55–63, 66]. The torsional stress in the diaphysis of the ulna usually occurs between the origin of the flexor digitorum profundus and the outcropping muscles [49].
In throwing athletes, an ulnar shaft stress fracture may occur more proximally in the diaphysis as the mechanism is similar to that described for humeral stress fractures. During the acceleration phase there is internal humeral rotation and rapid extension of the elbow, which generates tremendous valgus forces about the medial aspect of the elbow joint and valgus extension forces posteriorly [4]. These stresses are transmitted primarily to the medial collateral ligament complex of the elbow, the flexor carpi ulnaris, and the medial flexor-pronator muscles, and thus load the proximal ulnar diaphysis [52, 54].
Presentation
Across each sport, presentation was very similar. Athletes presented with an insidious onset of pain in the ulnar shaft exacerbated by activity. The time before presentation ranged from weeks to months. In many cases, a recent increase in the length, intensity, or demands of training was noted [48–50, 54, 57, 58, 60–62, 66, 68]. Some athletes tried symptomatic treatment, which included anti-inflammatories, physiotherapy, and ice, none of which was significantly helpful. Rest from the offending activity tended to lessen the pain, with a classic flare on return to sport noted [51, 56–59, 62]. The location of the pain was reported anywhere from the proximal ulna into the elbow, down to the distal ulna into the wrist, and corresponded well with the location of the stress fracture.
Diagnosis
There is tenderness to palpation in the area of the stress fracture. Often resisted wrist flexion and extension or resisted pronation and supination of the forearm can reproduce the pain [48, 50, 54, 55, 57, 64, 66, 67]. Plain radiographs are often negative if performed within the first few weeks of injury. MRI or bone scan should be performed if radiographs are negative or equivocal.
Treatment and Prognosis
Ulnar shaft stress fractures should be managed non-operatively. Immobilization can be used for comfort, with immediate and total cessation from the offending activity. Often a 4–8 week period of rest from sport and/or immobilization is needed. Upon radiographic evidence of healing, or subsidence of symptoms, therapy can be begun if needed [47, 58, 65]. Most athletes are able to return to a pre-injury level of activity by 6–8 weeks after the initiation of conservative therapy.
Radius
Mechanism
Stress fractures of the radius in athletes have been described primarily in gymnasts [69–73], though case reports also exist in racquet sport athletes [74, 75], a basketball player [76], a pool player [77], an adolescent cyclist performing “wheelies” [78], and a field gun runner [79]. The epiphysis of the radius is the least resistant portion of the bone to shear and torsional forces [80], and this portion of the bone is particularly vulnerable when at its thickest, as seen during the growth spurt [81, 82]—placing adolescent athletes at higher risk. In all cases, repetitive torsional or axial loading forces on the radius eventually lead to the development of a stress fracture. The vast majority of these fractures occur in the distal one-third of the radius.
Tumbling and vaulting in gymnastics tends to produce an impact angle of 60–90° to the wrist which places increased stress on the radius [71]. In twisting (Tsukahara) vaults, one wrist is removed from the ground first, leaving the remaining (fulcral) wrist to suffer much of the twisting. This explains why in many gymnasts with radius stress fractures the injury usually occurs in their fulcral wrist [71]. The use of very soft mats also exaggerates the amount of dorsiflexion of the wrist again placing increased stress on the radius [73]. In beam and tumbling workouts, the hands may be fixed in a particular position while the forearms are undergoing torsion in the direction of pronation and supination. These torsional forces may, with time and repetition, affect the epiphysis of the radius [73].
Stress fractures of the radius in a tennis [75] and badminton player [74] have similarly been reported in the adolescent population. In the case of the basketball player, the stress associated with “dunking” of a basketball repeatedly (with striking of the forearms on the metal rim of the basket) was believed to have contributed to the injury [76]. In the case of the pool player, putting excessive “English” (side spin) on the ball generated repetitive torsional forces to the radius that eventually lead to a stress fracture [77]. In the case of the adolescent cyclist performing “wheelies,” the terminal motion of coming back down to the ground with a hard, jarring force to the forearm seemed to be the offending motion [78]. This patient’s stress fracture was closer to the mid-distal one-third diaphyseal junction of the radius. Lastly, in the case of the field gun runner, repeated unaccustomed heavy loading of the 900 lbs. muzzle of the gun barrel to his forearms was believed to have incited the stress fracture [79].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








