25 Upper and lower limb disorders in children
Cases relevant to this chapter
Essential facts
1. Congenital upper limb anomalies may be part of the VACTERL syndrome.
2. Many trigger thumbs recover spontaneously.
3. Approximately 400 cases of obstetric brachial plexus palsy (OBPP) occur annually in Britain; 50% recover by 2 years and 40% regain useful function, but muscle imbalance may cause shoulder dislocation.
4. Management of OBPP by physiotherapy prevents joint contractures; if the biceps do not recover by 3 months, investigation by neurophysiological testing and X-ray is indicated.
5. Persisting muscle imbalance and dislocation of the shoulder in OBPP require surgery.
6. Congenital talipes equinovarus is the most common birth deformity of the foot, especially in boys and in identical twins.
7. Tiptoe walking may develop at walking age; most children are neurologically normal.
8. Referred pain from the hip to the knee may be due to Perthes’ disease, a slipped upper femoral epiphysis (especially in adolescents) or hip dysplasia.
9. In later childhood and adolescence, ligament tears are more likely than fractures as the skeletal attachments of ligament become stronger.
10. In neonates, rapid detection and treatment is required for hip instability and septic arthritis; delay leads to deformity, stiffness, dislocation and osteoarthritis.
Polydactyly
Polydactyly may be associated with other conditions and is the second commonest hand anomaly. The duplication is either postaxial (of the little finger) or preaxial (of the thumb; Fig. 25.1). The extra digit may be a soft-tissue tag or may comprise partial or complete bony and soft-tissue duplication of the digit. Treatment involves surgical deletion of the extra digit.
Obstetric brachial plexus palsy
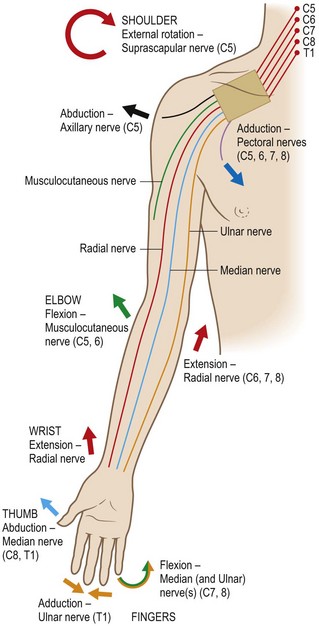
The injury affects the roots of the brachial plexus, most commonly the upper ones (Fig. 25.2). The outcome depends largely on the severity of the lesion, which is described by the Narakas classification (Table 25.1).
Table 25.1 The Narakas classification
| Narakas Group | Roots and Muscles Affected | Outcome |
|---|---|---|
| Group 1 | C5, C6. Biceps and deltoid | 90% recover fully |
| Group 2 | C5, C6, C7. All except long finger flexors | 65% recover fully; the rest have permanent deficit |
| Group 3 | C5, C6, C7, C8, T1. All except slight finger flexion | 1–2% recover fully; the rest have significant permanent deficit |
| Group 4 | C5, C6, C7, C8, T1 and Horner’s. All muscles and sympathetic function | None recovers fully; all have severe permanent deficit |
Failure of biceps recovery by 4 months also heralds a poor result.
Paediatric foot and ankle
Presentation of foot deformities at different ages
Birth
At birth, during infancy and when the child is a toddler, variations from normal may be encountered (see Chapter 24).
Congenital talipes equinovarus (clubfoot or congenitally inverted foot)
This is the most common significant deformity of the foot encountered at birth (Fig. 25.3). It is more likely to occur in boys. A family history is often identified, reaching its peak with identical twins when the condition is seen in 33% of siblings. Milder forms of the deformity may result from tight uterine ‘packaging’, including oligo-hydramnios. The more structurally severe feet have been shown to have neurological, vascular and other soft-tissue abnormalities.
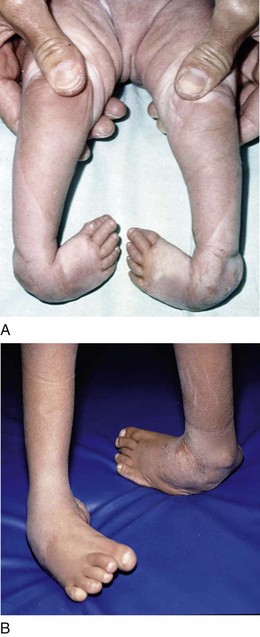
FIGURE 25.3 Congenital talipes equinovarus (clubfoot). (A) In the infant; (B) as an established deformity in childhood
Childhood
Pes cavus
1. Weakness of soleus and gastrocnemius, with over-action of the long toe flexors
2. Weakness of ankle dorsiflexion resulting in over-action of the long toe extensors
3. Weakness of the intrinsic muscles
4. A weak peroneus brevis muscle with overactive peroneus longus.
The neurological conditions responsible include cerebral palsy, poliomyelitis, Friedreich’s ataxia, myelomeningocele and other abnormalities of the spinal cord, such as spinal dysraphism or syringomyelia, and peripheral neuropathies. The commonest cause of this in the UK is hereditary sensory and motor neuropathy (HSMN) type 1 (Charcot–Marie–Tooth disorder or peroneal muscular atrophy; see also Chapter 26). This autosomal dominant progressive local demyelinating disorder produces an initially correctible and then a rigid deformity associated with painful calluses. Hammering of the toes and hindfoot varus are also present.
• Soft-tissue surgery (releases and tendon transfers)
• Osteotomies (first metatarsal, midfoot, calcaneum)
The toes are often clawed, requiring flexor tendon releases or tendon transfers. Orthoses will help to reduce local pressure over the metatarsal heads.
Tiptoe walking
This gait pattern may develop at walking age or a little later in childhood. In some cases this is due to mild spastic diplegia (see also Chapter 26). The majority of children with the condition seem to be neurologically normal, so the term ‘tight heel cords’ or ‘ballerina syndrome’ is used. Stretching by physiotherapy or casting is usually effective, but may have to be repeated. Lengthening of the Achilles tendon is avoided whenever possible because it is the calf muscle rather than the tendon that is pathologically shortened.
Early adolescence
Flat foot, pes cavus and toe deformities
Tarsal coalition
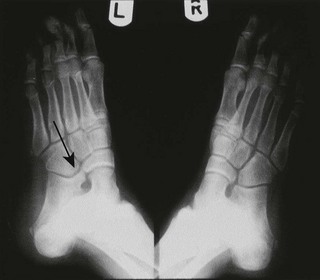
This produces a rigid structural flat foot and the normal appearance of a medial arch is absent if the child stands on tiptoe. Normally the embryonic mesodermal segments separate to form the different tarsal bones. A coalition represents a failure of complete segmentation, most commonly at the calcaneo-navicular site laterally (Fig. 25.4) and less frequently between the talus and the calcaneum medially. Other coalitions (for example, calcaneo-cuboid) have been described and they may occur at several sites in the same foot. The condition is often bilateral and hereditary. Symptoms develop in early adolescence as the cartilaginous bar ossifies and becomes rigid. Excision of the bar is worthwhile if conservative measures fail. Many cases of tarsal coalition remain asymptomatic or cause minimal stiffening.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree