Medial or lateral compartmental osteoarthritis or osteonecrosis
Age >50 years old
Weight <124.7 kg
Minimal pain at rest
Range-of-motion (ROM) arc >90° with <15° flexion contracture
Angular deformity <15° that is passively correctable to neutral
Although there are restrictions with regard to BMI, it should be noted that a recent study showed no correlation between BMI and revision rates at 5 years [21]. Further research is warranted in this area.
In addition to the above physical exam findings, a thorough preoperative workup is necessary. Radiographs including a weight-bearing anteroposterior (AP), lateral, stress, and patellar views should be obtained to help determine whether the patient is an appropriate candidate for UKA.
7.3.2 Medial UKA
Recent literature regarding medial UKA (MUKA) has investigated additional criteria which have expanded the ideal patient to include the younger population as well as created some specific indications such as intact ACL and a deformity that corrects ≤10° for a varus knee and ≤5° in a valgus knee [22–24].
The recent literature has continued to emphasize that regardless of the patient’s age, thorough preoperative evaluation is imperative. This includes thorough history and physical exam. With the strict inclusion criteria, a missed contraindication can have catastrophic results. The current trends that differ from the “older patient” criteria seem to favor full-thickness cartilage in the opposite compartment, intact ACL, and full extension (Table 7.2).
Unicompartmental involvement (Ahlback stage narrowing greater than or equal to 2) |
100° ROM |
Full extension |
Absence of patellofemoral joint (PFJ) involvement 30°, 60°, 90° flexion views |
Total correction of deformity in coronal plane on stress x-rays |
Full-thickness cartilage in lateral compartment |
Intact ACL (verified with MRI if needed) or ability of the surgeon to perform a reconstruction |
It is worth mentioning that there has been evidence against performing a MUKA in a knee with less than severe arthritic change. Niinimäki et al. [26] reported a series of 113 MUKAs with a mean follow-up of 63 months and examined the reoperation rates as they related to a number of factors. They determined that reoperation rates were dependent on the joint space preoperatively. When the thickness of the medial joint space was >2 mm, the revision rate was six times higher and eight times higher when the medial space was >40 % of the thickness of the lateral space.
In summary, the criteria for MUKA are extremely rigid and require that a surgeon be well versed in patient selection to ensure proper preoperative discussions and consistent outcomes.
7.3.3 Lateral UKA
The indications for lateral UKA (LUKA) have been extrapolated from Kozinn and Scott [18] and narrowed. There is a lack of studies including younger patients. For example, Pennington et al. [27] and Smith et al. [28] reported an average age of 68 years old and 64.8 years old, respectively. Their indications were as follows:
1.
Diagnosis of noninflammatory arthritis
2.
At least 90° of knee flexion
3.
Intact ACL
4.
Flexion contracture of ≤10°
5.
Maximum valgus deformity of 20° that can be corrected to <7° of valgus (with the knee in maximum extension)
Pennington et al. also included patients with arthrosis secondary to trauma, weight >180 lbs., and osteophytes or chondrocalcinosis seen on radiographs. The authors used intraoperative examination of the other two compartments in their decision-making process. If the uninvolved compartment and the patellofemoral joint contained Outerbridge grade 2 or less, they proceeded with LUKA.
The key to LUKA is understanding the mechanics of the lateral femoral condyle on the tibia as the knee progresses through its range of motion. Pennington et al. [27] used these principles to place the tibial component in 10–15° of internal rotation corresponding to knee mechanics driving the femur into internal rotation of approximately 20° on the tibia at full extension.
7.3.4 Patellofemoral Arthroplasty
Original designs for patellofemoral arthroplasty (PFA) resurfaced only the patella; however, the second-generation designs incorporated a trochlear component due to the persistence of knee pain after patella resurfacing. PFA is ideal for a patient with arthritis as a result of patellofemoral dysplasia without maltracking. Any medial or lateral joint line tenderness should be a strict contraindication to PFA with consideration made for other more extensive treatment options. The indications for PFA are listed in Table 7.3.
<60 years old |
Chondromalacia grade I or II |
Q-Angle <20° in women and <15° in men (unless corrected prior to PFA with anteromedialization of the tibial tubercle) |
Lack of medial or lateral joint line pain |
Absence of patellofemoral maltracking or malalignment |
7.4 Controversies
7.4.1 Deficient ACL in Young Patients
7.4.1.1 Medial UKA
There has historically been controversy surrounding the extent to which an ACL deficiency is a contraindication to MUKA. In a cadaveric kinematic study, Suggs et al. [30] demonstrated a larger anterior translation of the tibia on the femur in ACL-deficient static-bearing MUKA. The authors speculated that this instability would create an environment in which further lateral and patellofemoral compartment wear would ensue. The mechanics of the Suggs study were tested by Argenson et al. [31] who found that when an ACL-deficient MUKA was in extension, the femur had a posterior contact position on the tibia. They also observed a paradoxical anterior translation of the femur on the tibia, which is also thought to play a role in accelerated wear of the polyethylene bearing.
Despite the above studies and their findings, some studies have suggested that good to equivocal results and survivorship could be expected in ACL-deficient knees [32–34]. One of the criteria for such outcomes was that the tibial component had to be positioned at <7° slope. These studies were not specifically focused on younger patients nor their expected increased activity level and demand on durability.
The ambiguity in whether or not to include ACL deficiency as a contraindication for UKA seems to swing from controversial to absolute in the younger population if the ACL instability is not addressed as well. In a recent study, Biswas et al. [7] offered ACL reconstruction at the time of their UKA in patients with ACL-deficient knees who were candidates for UKA. Results at a 2-year follow-up estimated a survival of 96.5 % at 10 years. Given the younger patient’s expected higher activity level and life expectancy, unaddressed ACL deficiency as a contraindication seems consistent among the studies related to UKA in younger patients [3, 19, 25, 7, 15, 35].
Given the above data, we recommend an algorithm based on Weston-Simmons et al. [36]. This stems from understanding the pathologic process of medial compartment osteoarthritis (MCOA) and its etiology. If arthritis is the primary pathology, it will extend from an anterior to posterior direction leading to progressive ACL destruction. As this is a chronic process, by the time the ACL is damaged, the MCL and lateral compartment are affected, thus precluding the use of a UKA. If ACL deficiency is the primary pathology, the arthritic changes begin posteriorly as a result of the posterior femoral subluxation in relation to the tibia. If a patient with the later pathologic process presents to clinic, the decision to treat both the ACL and MCOA in a single procedure is based on their primary complaint. If instability is the primary complaint, an ACL reconstruction is performed first. Should the primary complaint be pain, both an ACL reconstruction and UKA can be performed (see Fig. 7.1). With the use of this algorithm, the implant survival has been 93 %, with a patient satisfaction of 98 % [36].
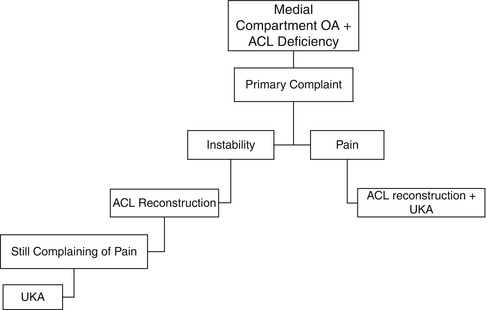
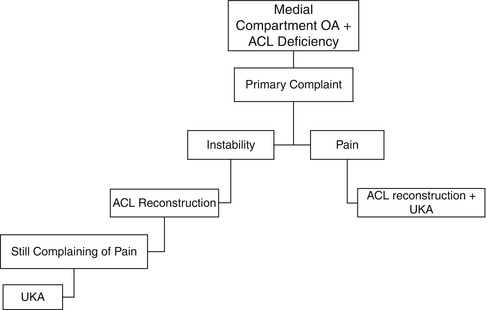
Fig 7.1
Algorithm for treatment of medial compartment OA with ACL tear
7.4.1.2 Lateral UKA
LUKA in an ACL-deficient knee has been contraindicated in all patient populations due to the increased motion of the lateral compartment particularly in regard to anteroposterior translation. This has been shown to have a higher rate of failure in static and mobile-bearing prostheses in ACL-deficient knees [13]. There is a paucity of data with regard to LUKA with ACL repair at the time of surgery and thus no recommendations as to the potential use of such surgical management.
Regardless of the patient, ACL reconstruction at the time of UKA should be reserved for the surgeon well experienced in both UKA and ACL reconstructions. Although the literature has supported UKA in ACL-deficient knees if they lack clinical or intraoperative instability, ACL reconstruction in clinically ACL-deficient patients who are candidates for UKA may also be an outcome supported surgical option.
7.4.2 Asymptomatic PFJ Arthritis
Typically PFJ arthritis has been a contraindication to UKA, especially in the young patient. Concerns for incomplete relief of pain or progressive arthritic change in the years postoperatively following the partial knee replacement have led to this contraindication. Recently the swing has been for the surgeon to use physical exam as a guide of inclusion for a patient with PFJ arthritis, namely, does the patient have anterior knee pain [25]. Symptomatic PFJ arthritis is thought to be a contraindication to surgery and not necessarily as dependent on radiographic findings.
7.4.3 Mobile Versus Static Bearing
The challenge with reviewing the literature addressing fixed versus mobile bearings is that some of the published research involves components with older designs and issues for which the manufacturer has made substantial corrections. For example, in a retrospective review, Emerson et al. [37] reported a 99 % survivorship for the Oxford (Biomet, Warsaw, IN) meniscal-bearing design and 93 % for the Robert Brigham fixed-bearing design (Johnson & Johnson Orthopaedics, Raynham, MA), based on component loosening and revision. Concerns with this study include the author’s choice of compared implants occurred during two different time periods and therefore may not account for changes in the technology or advances in the surgeon’s skill and experience. Contrast that finding to one earlier on in the development of the Oxford, which showed mobile-bearing revision to be twice that of fixed-bearing revisions. The most common reason for revision was for dislocated poly [13].
Keeping this in mind, there are arguments to be made for both bearing options, and as the current literature is reviewed, the difficulties of both types are heavily technique dependent.
7.4.3.1 Pros
Mobile
The concept behind mobile-bearing surfaces is the reduction of shear forces due to the fully congruent and unconstrained design, thus giving the implant reduced wear rates. Studies suggest that due to the congruent nature of mobile bearings as well as the lack of constraint, there is minimal wear and shear forces and thus decreased chance of loosening of the tibia baseplate. Twenty-year in vivo wear rates have been reported to be as low as 0.4 mm with a 0.02 mm/year wear rate [38].
Static
One of the earliest static-bearing designs was the Marmor prosthesis (Smith & Nephew, Memphis, TN). The tibial component was cemented on cancellous bone within the cortical rim as an inlay prosthesis resulting in high levels of subsidence and failure. Metal backing was introduced in the 1980s in order to evenly distribute the forces across a wider area. With the modularity that the metal-backed components provide, femoral component implantation became easier and also allowed for an isolated poly exchange should the patient require it. Static bearings also eliminated concerns for spin out of the bearing and dislocation of the poly insert.
7.4.3.2 Cons
Mobile
The most commonly cited issue with mobile-bearing designs is the worry for poly dislocation. This is seen in both medial and lateral UKA patients. Gunther et al. [39] saw an increased risk in lateral UKA when compared to MUKA in a series of fifty-three patients. There was a 10 % rate of bearing dislocation and a 21 % failure rate at 5 years postoperatively. Although techniques and implant design have improved dislocation, it still remains a concern that needs to be considered when choosing a mobile bearing. Some designs such as the LCS (low contact stress) component (DePuy, Warsaw, IN) use a dovetail track to lower the chances of poly dislocation [13]. A meta-analysis of the Oxford UKA showed a dislocation rate of 0.4 %, which has been considered acceptable [40]. The difficulty with bearing dislocation in UKA is that it often is due to poor positioning of the implants, and thus, a full revision may need to be done in order to prevent future dislocations.
Static
Despite the advantages, the metal-backed design brings some disadvantages as well. A dichotomy between thinner poly and larger tibial bone cut is created, whereas the surgeon must take multiple factors into consideration when deciding on an implant. Studies have shown that the greatest success for fixed-bearing devices has come from round-on-flat or slightly dished geometries [13]. Concerns for increased wear of the poly due to higher constraint in static bearing designs have also been published. Increased wear in the second decade of patients under 60 years of age with fixed-bearing (Miller–Galante) UKA has been noted and should be taken into consideration when potentially recommending these designs to younger, active patients [41].
7.4.3.3 Outcomes
Recent literature has shown that mobile-bearing UKA in patients under 60 years has a similar rate of failure as in those over 60 years of age, including a survival of 97 % at 10 years [42]. There have been several studies showing the long-term benefit of fixed- and mobile-bearing UKA designs. Berger et al. [20] recently reported results of a modular fixed-bearing, metal-backed tibial component. The authors noted that their thinnest polyethylene was 5.7 mm and was used in more than half of their patients. They showed a survival of 96 % at an average of 12-year follow-up (minimum 10-year follow-up) with 92 % of patients having excellent or good outcomes. The average age was 68 years (range 51–84). The authors emphasized their strict patient selection (Kozinn and Scott) and surgical technique as reasons for their success.
Similarly, Price et al. [43] reported a survival of 93 % at 15 years with 91 % of patients having good or excellent results with a mobile bearing. The authors argued that the decreased polyethylene contact stresses resulting from the mobile bearing’s congruent design allowed them to implant polyethylene liners as thin as 3.5 mm with no change in clinical outcome or failure rate. The clinical relevance of the thin polyethylene liner is that it allows for a smaller tibial bone cut and increased preservation of native bone to allow for more options at the time of a revision.
In a recent study, a comparable 20-year survivorship rate was found between the two bearing types with slight differences observed between the United Kingdom, North America, and Europe [44]. This is also supported by a paper that looked at revision rates between the two bearing types at 15-year follow-up. The authors considered revision for any reason to be an end point and showed 12 of 77 (15 %) UKAs were revised (for aseptic loosening, dislocation, and arthritis progression) in the mobile-bearing group and 10 of 79 (12 %) in the fixed-bearing group (for wear and arthritis progression) [45].
There has only been one prospective, randomized controlled study comparing mobile and static bearing [46]. The authors compared the AMC mobile-bearing component (Alphanorm, Quierschied, Germany) with the Allegretto fixed-bearing component (Centerpulse, Baar, Switzerland). At a mean 5.7-year follow-up, there was no statistically significant difference between the groups with regard to revision rates or clinical outcome scores.
Radiographically, the number of overcorrections and the number of radiolucencies tend to be statistically higher in the mobile-bearing group (69 % vs. 24 %); however, this doesn’t seem to make a difference in revision rates [41].
Kinematic analysis has shown that the mobile-bearing UKA has normal kinematics at 1 and 10 years. Static UKA kinematics are normal at 1 year, but at 10 years, the kinematic profile deteriorates to that of a TKA [44]. The mean Knee Society function and knee scores were comparable in a recent study comparing the two types of bearing surfaces at 15 years [41].
7.4.3.4 Summary
Regardless of the bearing type selected by the surgeon, advances in technology as well as surgeon comfort level in dealing with not only the primary procedure but each complication associated with its given bearing type need to be thoroughly considered. The complications of each bearing result typically from component malposition. We recommend either bearing type as long as the surgeon is comfortable with component implantation and understands the kinematics of each implant design.
7.5 Unicompartmental Knee Arthroplasty Outcomes
7.5.1 Medial UKA
Age has not been reported to be a predictor of poor outcomes. In fact, in a recent study by Thompson et al. [47], there was no significant difference in Knee Society Score (KSS) at 1 year; however, at 2 years there was a statistically significant difference in KSS with patients <60 years old scoring higher (Fig. 7.2).
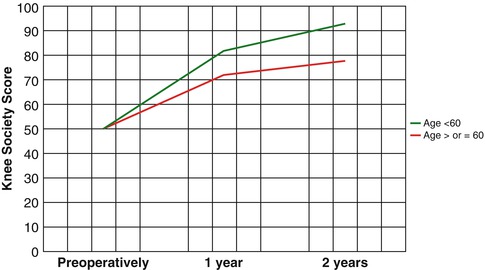
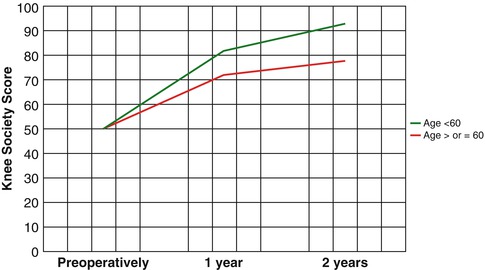
Fig 7.2
KSS scores in patients <60 and >60 years, 1 and 2 years post MUKA (Data from Thompson et al. [47]. P-value >0.05 at 1 year, which becomes significant (p-value 0.01) at 2 years postoperatively)
The outcomes for MUKA in young patients have been reported before, and there seems to be differing opinion between the studies conducted in the United States and those in Europe with regard to survival. For example, the Swedish Knee Arthroplasty Registry found a 10-year survival rate of 83 % in patients <65 years of age who received a UKA for osteoarthritis. However, there was no mention of patient selection or surgical experience, and the data included at least nine different prostheses [25]. Besides the lack of patient data, the registry data’s lack of surgical experience data leaves the outcomes suspect as it has been reported that long-term results for unicompartmental arthroplasty are related to the number of surgeries performed by a given unit (study center) and reduce the failure of the UKA [48].
A recent study by Heyse et al. [49] studied lateral and medial UKA in patients <60 years old (average age at index operation – 53.7 (SD 5.8, range 30–60) years) with a mean follow-up of 10.8 years. The KSS was 94.3 (SD 7.8), and the function score was 94.9 (SD 6.8) with a 94.3 implant survival rate. Survivorship for the entire cohort was 93.5 % at 10 years (MUKA 94.1 % vs. lateral 91.8 %) and 86.3 % at 15 years (85.1 % medial vs. 91.7 % lateral). This seems to be consistent with other literature on MUKA in young patients (Table 7.4) [7, 49, 19, 50, 51, 25, 52].
Table 7.4
Summary of literature reporting results of MUKR in young patients
Study | Year | Age | ROM preoperatively (°) | ROM postoperatively (°) | Mean KSS preoperatively | Mean KSS postoperatively | Survival (years) | UCLA activity score at follow-up |
|---|---|---|---|---|---|---|---|---|
Biswas et al. [7] | 2014 | 49 | 120 | 124 | 49 | 95.1 | 96.5 % at 10 years (95 % confidence interval, 89.4 %–98.8 %) | 7.5 |
Dalury et al. [53] | 2013 | 46–59 | Significant increase postoperatively | 94.1 % at 6 years (95 % CI, 78.3–98.5) | ||||
Heyse et al. [49]a | 2012 | 53.7 | 50.1 | 94.3 | 93.5 % at 10 years, 91.3 % at 12 years, and 86.3 % at 15 years (MUKA was 94.1 % at 10 years, 91.2 % at 12 years, and 85.1 % at 15 years) (91.8 % at 10 and 15 years for LUKA) | |||
Felts et al. [19] | 2010 | 54.7 | 110 | 132 | 50 | 94 | 94 % at 12 years (95 % CI, 0.87–0.96) | 6.8 |
Parratte et al. [50] | 2009 | 46 | 110 | 132 | 54 | 97 | 80.6 % at 12 years and 70 % at 16 years | |
Cartier et al. [51] | 2007 | 53 | 94.02 | 94 % at 10 years, 92 % at 11 years, and 88 % at 12 years | ||||
Price et al. [25]
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




